The objective of this study was to assess the implementation of safe medication practices in hospital emergency services, in order to understand the points of greatest risk as well as the safety challenges faced by these departments, and to plan collaboratively improvement initiatives.
MethodMulticentric and descriptive study based on completion of the “Medication safety self-assessment of emergency services” from May 16, 2023 to November 16, 2023, at voluntarily participating emergency services. The survey contained 93 items grouped into 10 key elements. Mean score and mean percentages based on the maximum possible values for the overall survey, for the key elements and for each individual item of evaluation, were determined.
ResultsA total of 72 emergency services completed the questionnaire. The mean score obtained for the overall questionnaire was 428.3 points (51.1% of the maximum score). Results showed a large variation among the scores of the participating services (range: 164.0–620.5). Four key elements had values below 50%, corresponding to competence and training of professionals in safety practices (38.4%); incorporation of pharmacists in emergency departments (42.1%), availability and accessibility of information about patients (43.1%), and patient education (48.1%). The highest values corresponded to labeling, packaging, and naming of medications (69.2%) and communication of prescriptions and other medication information (64%). No differences were found between emergency departments in the key elements according to the dependency or size of the hospital, or the type of department, except for the item referring to the incorporation of pharmacists in the emergency service, where differences were observed between hospitals with less than 200 beds (28.9%) and those with more than 500 (52.2%).
ConclusionThe application of the specific self-assessment questionnaire has made it possible to identify safety practices that are insufficiently implemented into emergency departments in our country and to identify critical points for improvement for which planning collaborative initiatives to reduce medication errors in these units should become a priority.
El objetivo principal de este estudio ha sido evaluar la implantación de prácticas seguras de medicación en los servicios de urgencias hospitalarios, con el fin de conocer los puntos de mayor riesgo y los retos de seguridad a los que se enfrentan estos servicios, para planificar iniciativas de mejora colaborativas.
MétodoEstudio multicéntrico de tipo descriptivo basado en la cumplimentación voluntaria del “Cuestionario de autoevaluación de la seguridad del uso de los medicamentos en los Servicios de Urgencias”, del 16/5/2023 al 16/11/2023. El cuestionario incluye 133 ítems de evaluación agrupados en 10 elementos clave. Se determinó la puntuación media y el porcentaje medio sobre el valor máximo posible en el cuestionario completo, en los elementos clave y en los ítems de evaluación.
ResultadosUn total de 72 servicios de urgencias cumplimentaron el cuestionario. El promedio de puntuación obtenida en el cuestionario fue de 428,3 puntos (51,1% de la puntuación máxima), observándose una gran variación entre las puntuaciones de los servicios participantes (rango: 164,0–620,5). Cuatro elementos clave mostraron valores inferiores al 50%, los correspondientes a: competencia y formación de los profesionales en prácticas seguras (38,4%), incorporación de los farmacéuticos en los servicios de urgencias (42,1%), disponibilidad y accesibilidad a la información sobre los pacientes (43,1%) y educación al paciente (48,1%). Los valores más altos correspondieron a los referentes al etiquetado, envasado y nombre de medicamentos (69,2%) y a la comunicación de las prescripciones y de información sobre la medicación (64%). No se encontraron diferencias entre los servicios de urgencias en los elementos clave según la dependencia o el tamaño del hospital, o el tipo de servicio de urgencias, excepto para el referente a la incorporación de farmacéuticos en los servicios de urgencias, donde se observaron diferencias entre los hospitales con menos de 200 camas (28,9%) y los de más de 500 (52,2%).
ConclusiónLa aplicación del cuestionario de autoevaluación específico ha permitido conocer prácticas de seguridad que están implementadas de forma insuficiente en los servicios de urgencias de nuestro país e identificar puntos críticos de mejora sobre los que sería prioritario planificar iniciativas colaborativas para reducir los errores de medicación.
Emergency services are among the areas with the highest prevalence of preventable adverse drug events, according to a recent report by the World Health Organization1. Various factors converge in these settings, creating a high risk of medication errors that may lead to adverse events for patients. Emergency services attend diverse types of patients presenting with a variety of conditions, often requiring the use of high-risk medications. Besides, healthcare professionals may not always have access to the patient's complete medical history; medications are generally administered at the point of care without pharmaceutical validation; there is a higher prevalence of verbal orders, particularly in urgent and high-stress situations; and physicians and nursing staff often treat multiple patients simultaneously, facing intense care pressure, frequent interruptions, etc.2,3
Medication errors in emergency services occur more frequently during the prescribing and administration processes, although they also happen in other processes, such as in care transitions, where errors have increased in recent decades, likely because the patients who come to these services are increasingly complex and take multiple medications3–7. The prevalence of preventable adverse drug events in emergency departments ranges from 2% to 12%8. In Spain, the EVADUR study showed that 12% of patients treated in these departments experienced some type of incident or adverse event related to their healthcare, of which 24.1% were related to medications9. To reduce errors and preventable adverse drug events, emergency services need to understand the etiology of these errors and establish effective safety practices in their processes, focusing on the points most prone to errors.
The Institute for Safe Medication Practices (ISMP) in the USA has developed several Medication Safety Self-Assessments© for different settings10. These questionnaires systematically outline the safe practices that, according to available evidence and ISMP's experience in error analysis, should be implemented in relevant settings to reduce risks in their processes. They serve as a proactive tool for improving safety, helping professionals assess the implementation of safe medication practices in their systems and identify and prioritiz improvement practices to minimize the risk of medication errors. Various organizations and scientific societies have recommended their use11,12.
In Spain, the Ministry of Health and ISMP-Spain published in 2007 the ‘Medication Use Safety Self-Assessment Questionnaire for Hospitals13, which is an adaptation of the Medication Safety Self-Assessment for Hospitals© to Spanish healthcare practice, and was updated in 201814. Based on this document, ISMP-Spain, the Redfaster Working Group of the Spanish Society of Hospital Pharmacy (SEFH), and the Spanish Society of Emergency Medicine (SEMES) developed the ‘Medication Safety Self-Assessment Questionnaire for Emergency Services‘,considering the distinctive characteristics of these services and the etiology of the most common types of errors15. This specific questionnaire is useful at the local level to help professionals become familiar with safe practices, identify high-risk areas, and establish programs to improve medication safety.
Once this tool was available, the present study was undertaken for the purpose of evaluating the implementation of safe medication practices in emergency departments at the national level and identifying high-risk areas and the safety challenges that these services face and, from there, planning collaborative improvement initiatives.
MethodsThis is a multicenter descriptive study conducted to assess the implementation of safety practices as outlined in the ‘Medication Use Safety Self-Assessment for Emergency Services’ questionnaire. The option to participate in the study was offered to all emergency services that completed the questionnaire within a predetermined period (from May 16, 2023 to November 16, 2023).
The study was distributed by SEFH and SEMES to their members via their email distribution lists. Participating services were instructed to create an interdisciplinary team to carry out the evaluation, and were provided with a password to access a software application for recording their responses. This application, hosted on the ISMP-Spain website, ensures data confidentiality.
Questionnaire and assessmentThe self-assessment questionnaire for emergency services was developed by ISMP-Spain with the collaboration of a panel of experts from the Redfaster and Clinical Safety groups of SEFH, and SEMES15. It comprises 133 evaluation items representing specific practices or measures aimed at preventing medication errors in emergency services. Of these, 99 are items from the hospital questionnaire, 30 are items whose content was adapted to the emergency setting, and 4 are new items corresponding to specific safety practices. The questionnaire is structured into 10 sections which represent the 10 key elements that, according to ISMP's conceptual model, determine the safety of the medication use system.
The degree of implementation of each evaluation item in the emergency department must be assessed using a scale with the following 5 possible responses:
- a.
No initiative has been taken to implement this item.
- b.
This item has been discussed for possible implementation, but has not been implemented.
- c.
This item has been partially implemented across some or all areas, patients, medications, or healthcare professionals.
- d.
This item has been completely implemented across some areas, patients, medications, or healthcare professionals.
- e.
This item has been completely implemented across all areas, patients, medications, or healthcare professionals.
The evaluation items are assigned different values based on their effectiveness in reducing medication errors. Option A always scores 0, while the values for options B, C, D, or E increase, with option E ranging from 2 up to a maximum score of 16, corresponding to practices whose implementation is highly effective in preventing medication errors. Additionally, in the questionnaire, there are 3 items with the option to be marked as ‘not applicable,’ considering the possibility that a particular emergency department may not have automated dispensing systems. If these are marked as ‘not applicable,’ they are subtracted from the overall calculation.
Completion of the questionnaireThe members of the interdisciplinary teams established in the emergency departments evaluated the degree of implementation for each item in the questionnaire. Once the self-assessment was completed, the responses were recorded by the responsible personnel from each center in the questionnaire's software application, which is always accessible so that each emergency department can access its information. In this way, each service obtained the evaluated results of its data according to key elements and evaluation items. They were also able to compare their results with the aggregated information from other emergency services.
Data analysisThe analysis of the results from the participating services in the study included the calculation of the mean absolute score obtained for the entire questionnaire, as well as for each key element and evaluation item. The percentage of the maximum possible score or value for each key element and evaluation item was also calculated to reflect their degree of implementation and identify opportunities for improvement, as well as to enable comparisons, since the maximum possible or achievable scores for each of them differ. This average percentage would range from 0% (indicating no implementation) to 100% (full implementation).
A descriptive statistical analysis of the characteristics of the emergency services participating in the study was performed. The scores and percentages of the maximum possible scores achieved for the complete questionnaire and for the key elements were compared among the emergency services in the sample, which were stratified according to their characteristics. The following variables were considered: 1) functional dependency (public or private hospitals); 2) number of beds (less than 200 beds, 200–499 beds, and more than 500 beds); 3) type of emergency service (general and others); and 4) postgraduate teaching or not. The mean percentages of the dichotomous variables were compared using the Student t-test. The variable number of beds was compared using the ANOVA test. A p-value of <.05 was used as a cutoff for statistical significance. All statistical analyses were performed using SPSS version 25 (IBM, Chicago).
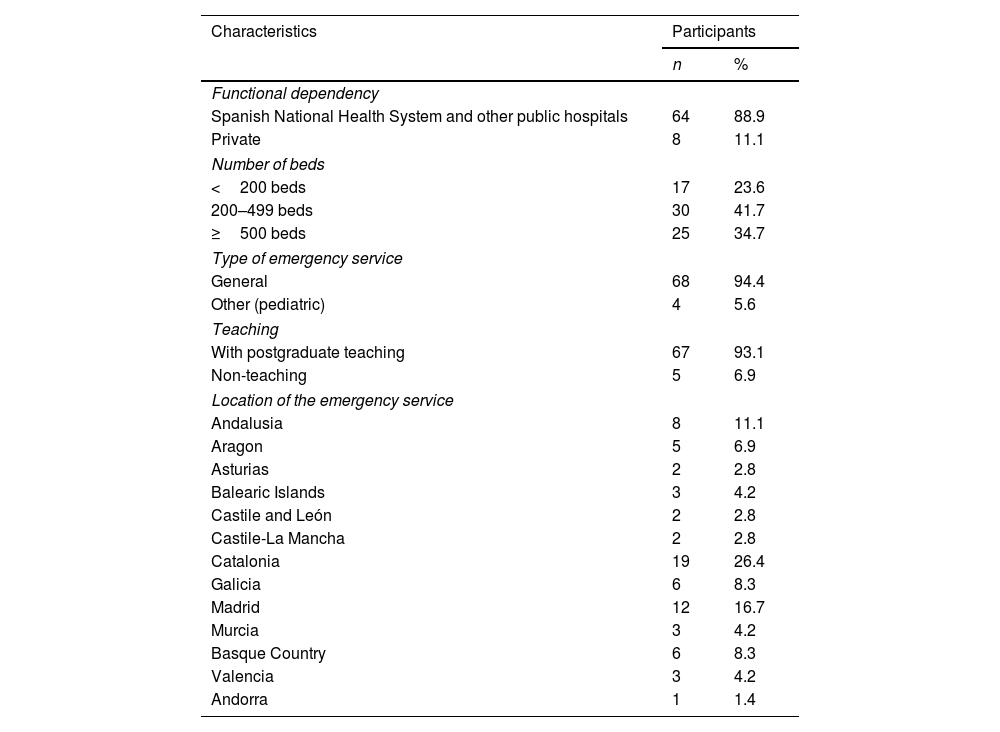
ResultsBy the end of the study, 72 emergency services had completed the questionnaire, 71 from 12 Spanish autonomous communities and 1 from Andorra. Table 1 shows their characteristics. Of the 72 participating emergency services, 68 were general and 4 were pediatric.
Characteristics of the emergency services that participated in the study (n = 72).
| Characteristics | Participants | |
|---|---|---|
| n | % | |
| Functional dependency | ||
| Spanish National Health System and other public hospitals | 64 | 88.9 |
| Private | 8 | 11.1 |
| Number of beds | ||
| <200 beds | 17 | 23.6 |
| 200–499 beds | 30 | 41.7 |
| ≥500 beds | 25 | 34.7 |
| Type of emergency service | ||
| General | 68 | 94.4 |
| Other (pediatric) | 4 | 5.6 |
| Teaching | ||
| With postgraduate teaching | 67 | 93.1 |
| Non-teaching | 5 | 6.9 |
| Location of the emergency service | ||
| Andalusia | 8 | 11.1 |
| Aragon | 5 | 6.9 |
| Asturias | 2 | 2.8 |
| Balearic Islands | 3 | 4.2 |
| Castile and León | 2 | 2.8 |
| Castile-La Mancha | 2 | 2.8 |
| Catalonia | 19 | 26.4 |
| Galicia | 6 | 8.3 |
| Madrid | 12 | 16.7 |
| Murcia | 3 | 4.2 |
| Basque Country | 6 | 8.3 |
| Valencia | 3 | 4.2 |
| Andorra | 1 | 1.4 |
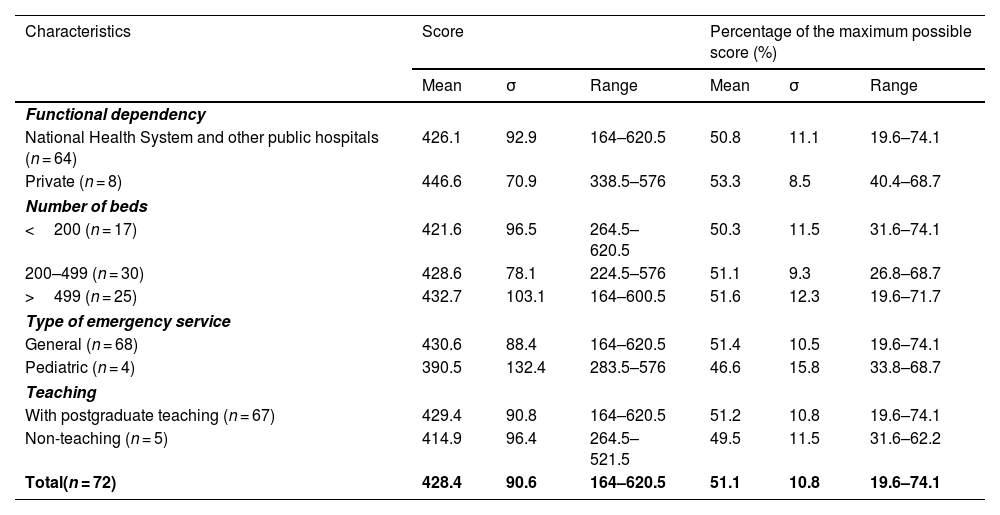
Table 2 shows the results obtained for the entire questionnaire in the 72 emergency departments and in the different groups established based on the characteristics considered. The mean score for the entire questionnaire in the total sample was 428.3 points, corresponding to 51.1% of the maximum possible score (838 points). A large variation was observed in the scores obtained by the different participating emergency departments, ranging from 164 to 620.5 points. No statistically significant differences were found between the percentages of the maximum possible scores obtained among the different groups established.
Results for the complete questionnaire according to the characteristics of the emergency services (n = 72).
| Characteristics | Score | Percentage of the maximum possible score (%) | ||||
|---|---|---|---|---|---|---|
| Mean | σ | Range | Mean | σ | Range | |
| Functional dependency | ||||||
| National Health System and other public hospitals (n = 64) | 426.1 | 92.9 | 164–620.5 | 50.8 | 11.1 | 19.6–74.1 |
| Private (n = 8) | 446.6 | 70.9 | 338.5–576 | 53.3 | 8.5 | 40.4–68.7 |
| Number of beds | ||||||
| <200 (n = 17) | 421.6 | 96.5 | 264.5–620.5 | 50.3 | 11.5 | 31.6–74.1 |
| 200–499 (n = 30) | 428.6 | 78.1 | 224.5–576 | 51.1 | 9.3 | 26.8–68.7 |
| >499 (n = 25) | 432.7 | 103.1 | 164–600.5 | 51.6 | 12.3 | 19.6–71.7 |
| Type of emergency service | ||||||
| General (n = 68) | 430.6 | 88.4 | 164–620.5 | 51.4 | 10.5 | 19.6–74.1 |
| Pediatric (n = 4) | 390.5 | 132.4 | 283.5–576 | 46.6 | 15.8 | 33.8–68.7 |
| Teaching | ||||||
| With postgraduate teaching (n = 67) | 429.4 | 90.8 | 164–620.5 | 51.2 | 10.8 | 19.6–74.1 |
| Non-teaching (n = 5) | 414.9 | 96.4 | 264.5–521.5 | 49.5 | 11.5 | 31.6–62.2 |
| Total(n = 72) | 428.4 | 90.6 | 164–620.5 | 51.1 | 10.8 | 19.6–74.1 |
σ: standard deviation.
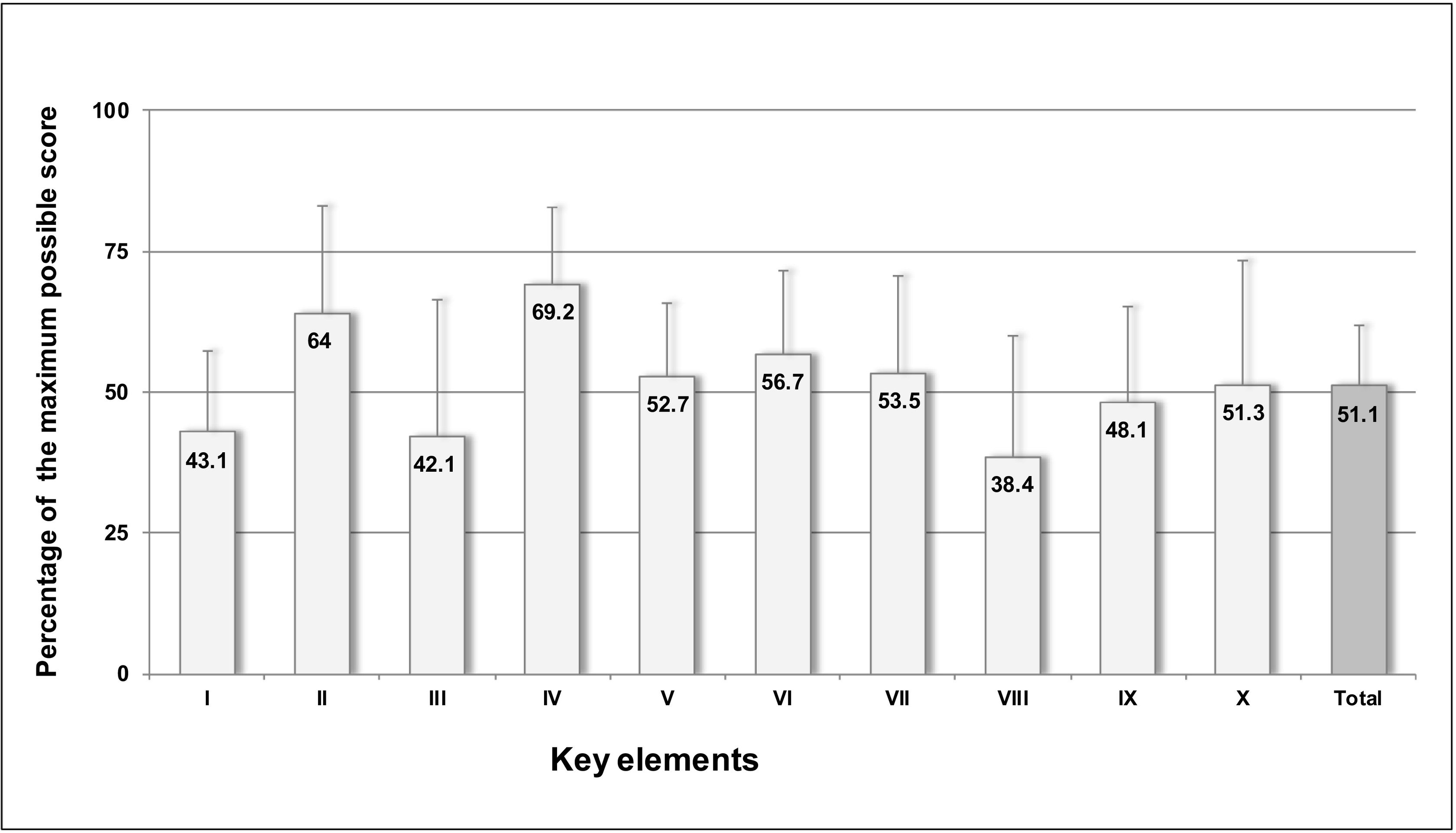
Fig. 1 shows the results for the key elements expressed as a percentage of the maximum possible score, allowing for comparison and identification of the areas of greatest risk. Four key elements scored less than 50%: element VIII on competency and training of healthcare professionals in safety practices (38.4%); element III on incorporating pharmacists into emergency services (42.1%); element I on availability and accessibility of essential patient and drug information (43.1%); and element IX on patient or family education (48.1%). The remaining key elements scored close to or more than 50%. The highest scores were for element IV on drug labeling, packaging, and naming (69.2%) and element II on communication of prescriptions and other drug information (64%).
Results from the 72 emergency services expressed as percentages of the maximum possible score by the 10 key elements and for the complete questionnaire.
Abbreviated description of the key elements: I. Availability and accessibility of patient and drug information. II. Communication of prescriptions and other drug information. III. Incorporation of pharmacists into emergency service teams. IV. Drug labelling, packaging, and naming. V. Drug standardization, storage, and distribution. VI. Medication device acquisition, use, and monitoring. VII. Environmental factors and human resources. VIII. Staff competency and training in medications and safety practices. IX. Patient or family education. X. Quality processes and risk management.
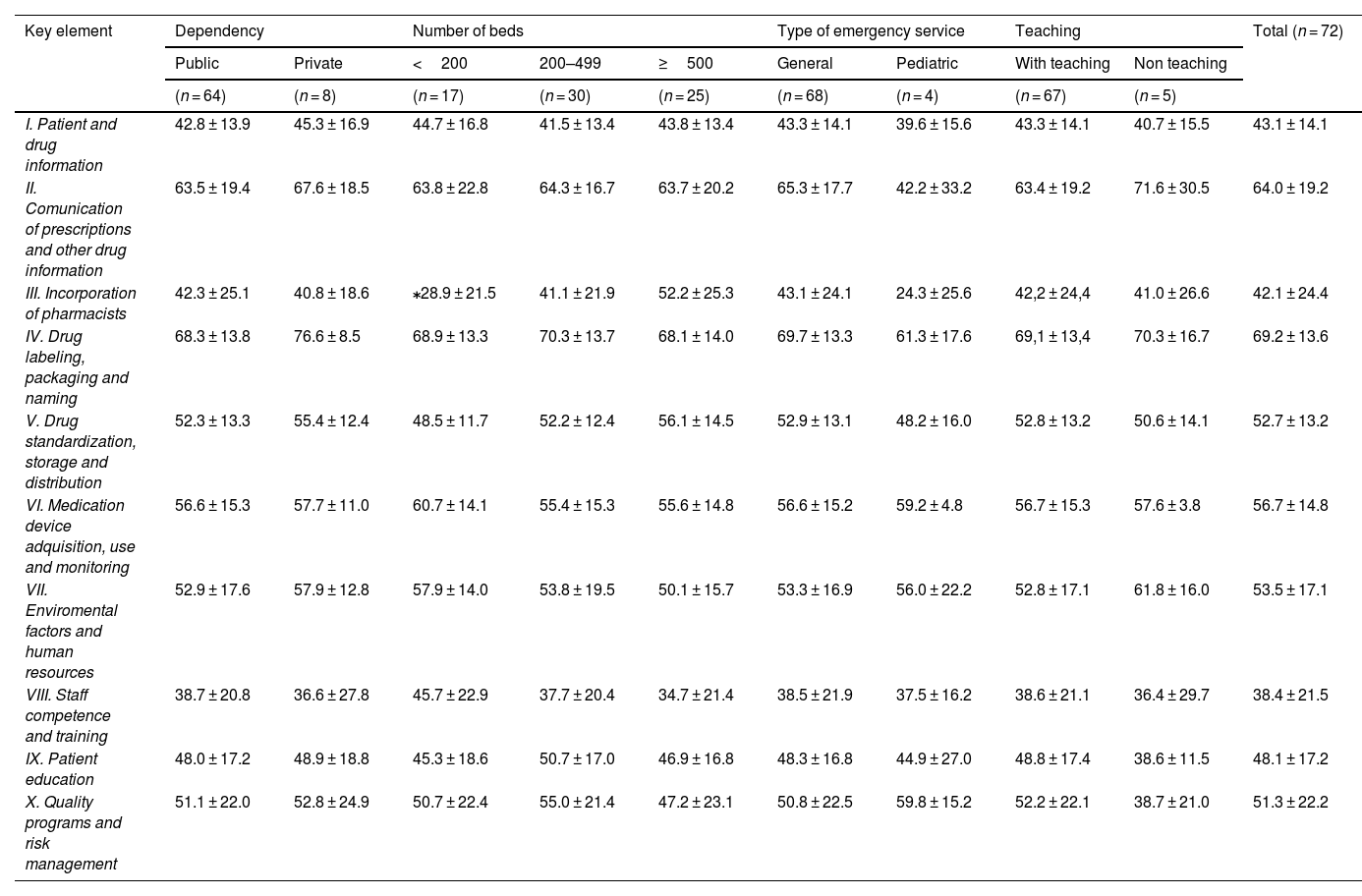
Table 3 presents the results expressed as a percentage of the maximum possible scores for the 10 key elements in the totality of emergency services, as well as in the groups categorized by the hospital's functional dependency and size, type of emergency service, and teaching activity. No statistically significant differences were found between public or private hospitals, number of beds, type of service, or teaching activity, except for key element III corresponding to the incorporation of pharmacists in emergency services. In this case, statistically significant differences (p = .008) were observed between hospitals with less than 200 beds (28.9%) and those with more than 500 beds (52.2%).
Results for the key elements expressed as percentage of the maximum possible score (mean ± standard deviation) according to the emergency service characteristics (n = 72).
| Key element | Dependency | Number of beds | Type of emergency service | Teaching | Total (n = 72) | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Public | Private | <200 | 200–499 | ≥500 | General | Pediatric | With teaching | Non teaching | ||
| (n = 68) | (n = 4) | (n = 67) | (n = 5) | |||||||
| (n = 64) | (n = 8) | (n = 17) | (n = 30) | (n = 25) | ||||||
| I. Patient and drug information | 42.8 ± 13.9 | 45.3 ± 16.9 | 44.7 ± 16.8 | 41.5 ± 13.4 | 43.8 ± 13.4 | 43.3 ± 14.1 | 39.6 ± 15.6 | 43.3 ± 14.1 | 40.7 ± 15.5 | 43.1 ± 14.1 |
| II. Comunication of prescriptions and other drug information | 63.5 ± 19.4 | 67.6 ± 18.5 | 63.8 ± 22.8 | 64.3 ± 16.7 | 63.7 ± 20.2 | 65.3 ± 17.7 | 42.2 ± 33.2 | 63.4 ± 19.2 | 71.6 ± 30.5 | 64.0 ± 19.2 |
| III. Incorporation of pharmacists | 42.3 ± 25.1 | 40.8 ± 18.6 | ⁎28.9 ± 21.5 | 41.1 ± 21.9 | 52.2 ± 25.3 | 43.1 ± 24.1 | 24.3 ± 25.6 | 42,2 ± 24,4 | 41.0 ± 26.6 | 42.1 ± 24.4 |
| IV. Drug labeling, packaging and naming | 68.3 ± 13.8 | 76.6 ± 8.5 | 68.9 ± 13.3 | 70.3 ± 13.7 | 68.1 ± 14.0 | 69.7 ± 13.3 | 61.3 ± 17.6 | 69,1 ± 13,4 | 70.3 ± 16.7 | 69.2 ± 13.6 |
| V. Drug standardization, storage and distribution | 52.3 ± 13.3 | 55.4 ± 12.4 | 48.5 ± 11.7 | 52.2 ± 12.4 | 56.1 ± 14.5 | 52.9 ± 13.1 | 48.2 ± 16.0 | 52.8 ± 13.2 | 50.6 ± 14.1 | 52.7 ± 13.2 |
| VI. Medication device adquisition, use and monitoring | 56.6 ± 15.3 | 57.7 ± 11.0 | 60.7 ± 14.1 | 55.4 ± 15.3 | 55.6 ± 14.8 | 56.6 ± 15.2 | 59.2 ± 4.8 | 56.7 ± 15.3 | 57.6 ± 3.8 | 56.7 ± 14.8 |
| VII. Enviromental factors and human resources | 52.9 ± 17.6 | 57.9 ± 12.8 | 57.9 ± 14.0 | 53.8 ± 19.5 | 50.1 ± 15.7 | 53.3 ± 16.9 | 56.0 ± 22.2 | 52.8 ± 17.1 | 61.8 ± 16.0 | 53.5 ± 17.1 |
| VIII. Staff competence and training | 38.7 ± 20.8 | 36.6 ± 27.8 | 45.7 ± 22.9 | 37.7 ± 20.4 | 34.7 ± 21.4 | 38.5 ± 21.9 | 37.5 ± 16.2 | 38.6 ± 21.1 | 36.4 ± 29.7 | 38.4 ± 21.5 |
| IX. Patient education | 48.0 ± 17.2 | 48.9 ± 18.8 | 45.3 ± 18.6 | 50.7 ± 17.0 | 46.9 ± 16.8 | 48.3 ± 16.8 | 44.9 ± 27.0 | 48.8 ± 17.4 | 38.6 ± 11.5 | 48.1 ± 17.2 |
| X. Quality programs and risk management | 51.1 ± 22.0 | 52.8 ± 24.9 | 50.7 ± 22.4 | 55.0 ± 21.4 | 47.2 ± 23.1 | 50.8 ± 22.5 | 59.8 ± 15.2 | 52.2 ± 22.1 | 38.7 ± 21.0 | 51.3 ± 22.2 |
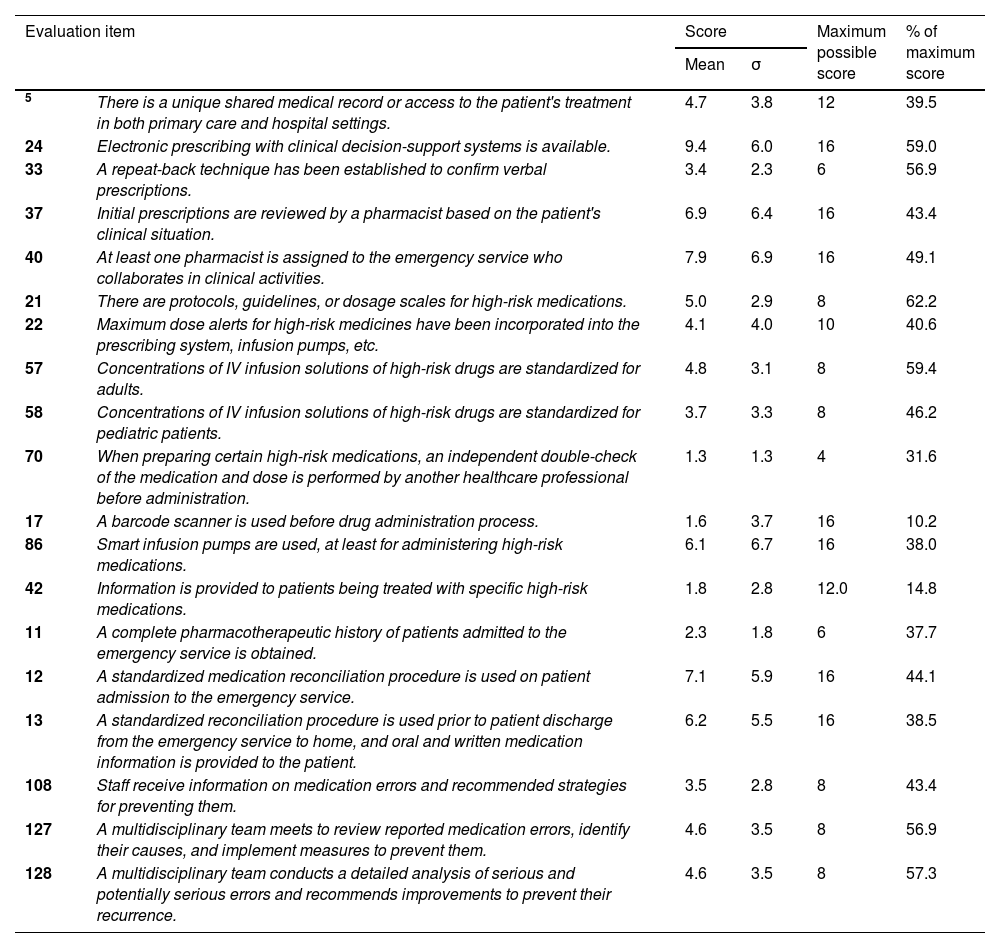
Table 4 includes the results for specific items corresponding to several safety practices recommended for implementation in emergency services, considering the processes most prone to errors and associated elevated risk factors.3,7,16 These practices include the following: accessibility to the patient's medical records; electronic prescribing systems with clinical decision-support; the establishment of a safe procedure for repeating verbal orders; incorporation of pharmacists in emergency care teams; the implementation of safe practices for high-risk medications, including the protocolization and standardization of intravenous solution concentrations, and the use of smart infusion pumps; barcode scanning in medication administration; medication reconciliation during care transitions; professional training, and analysis and learning from errors. Most of these items showed low implementation percentages, below or close to 50%, particularly the use of barcodes in administration (10.2%); the provision of information about high-risk medications to patients at discharge (14.8%); the use of smart infusion pumps (38%); and the availability of an integrated medical record (39.5%). Practices related to medication reconciliation such as obtaining a complete pharmacotherapeutic history (37.7%) and reconciling medications when discharging patients from the emergency department to their homes, also showed low implementation (38.5%).
Results for selected evaluation items corresponding to safe practices considered essential for implementation in emergency services.
| Evaluation item | Score | Maximum possible score | % of maximum score | ||
|---|---|---|---|---|---|
| Mean | σ | ||||
| 5 | There is a unique shared medical record or access to the patient's treatment in both primary care and hospital settings. | 4.7 | 3.8 | 12 | 39.5 |
| 24 | Electronic prescribing with clinical decision-support systems is available. | 9.4 | 6.0 | 16 | 59.0 |
| 33 | A repeat-back technique has been established to confirm verbal prescriptions. | 3.4 | 2.3 | 6 | 56.9 |
| 37 | Initial prescriptions are reviewed by a pharmacist based on the patient's clinical situation. | 6.9 | 6.4 | 16 | 43.4 |
| 40 | At least one pharmacist is assigned to the emergency service who collaborates in clinical activities. | 7.9 | 6.9 | 16 | 49.1 |
| 21 | There are protocols, guidelines, or dosage scales for high-risk medications. | 5.0 | 2.9 | 8 | 62.2 |
| 22 | Maximum dose alerts for high-risk medicines have been incorporated into the prescribing system, infusion pumps, etc. | 4.1 | 4.0 | 10 | 40.6 |
| 57 | Concentrations of IV infusion solutions of high-risk drugs are standardized for adults. | 4.8 | 3.1 | 8 | 59.4 |
| 58 | Concentrations of IV infusion solutions of high-risk drugs are standardized for pediatric patients. | 3.7 | 3.3 | 8 | 46.2 |
| 70 | When preparing certain high-risk medications, an independent double-check of the medication and dose is performed by another healthcare professional before administration. | 1.3 | 1.3 | 4 | 31.6 |
| 17 | A barcode scanner is used before drug administration process. | 1.6 | 3.7 | 16 | 10.2 |
| 86 | Smart infusion pumps are used, at least for administering high-risk medications. | 6.1 | 6.7 | 16 | 38.0 |
| 42 | Information is provided to patients being treated with specific high-risk medications. | 1.8 | 2.8 | 12.0 | 14.8 |
| 11 | A complete pharmacotherapeutic history of patients admitted to the emergency service is obtained. | 2.3 | 1.8 | 6 | 37.7 |
| 12 | A standardized medication reconciliation procedure is used on patient admission to the emergency service. | 7.1 | 5.9 | 16 | 44.1 |
| 13 | A standardized reconciliation procedure is used prior to patient discharge from the emergency service to home, and oral and written medication information is provided to the patient. | 6.2 | 5.5 | 16 | 38.5 |
| 108 | Staff receive information on medication errors and recommended strategies for preventing them. | 3.5 | 2.8 | 8 | 43.4 |
| 127 | A multidisciplinary team meets to review reported medication errors, identify their causes, and implement measures to prevent them. | 4.6 | 3.5 | 8 | 56.9 |
| 128 | A multidisciplinary team conducts a detailed analysis of serious and potentially serious errors and recommends improvements to prevent their recurrence. | 4.6 | 3.5 | 8 | 57.3 |
σ: standard deviation; IV: intravenous.
Emergency departments are environments with a high risk of medication errors. To minimize these errors, effective safe practices should be implemented in each and every process of the medication use system.
This study provides information on the current state of implementation of safety practices in the emergency departments of our hospitals, and highlights that there are numerous opportunities for improvement. The mean score for the entire questionnaire was 51.1%, with marked differences between participating services, showing values ranging from 19.6% to 74.1%. It should be noted, however, that the practices included in the questionnaire are not minimum safety standards, but rather, effective measures that emergency services should aim to implement to prevent errors; examples include barcode scanning during drug administration17 and double-checking before administration18.
To our knowledge, there are no similar studies conducted specifically in emergency departments with which the results can be directly compared. However, it is worth mentioning that the observed results are largely consistent with those of the latest study on the implementation of safety practices in Spanish hospitals, conducted in 2022 at 131 centers, using the general hospital questionnaire19. Although these studies are not entirely comparable as the hospital questionnaire is much broader and element III does not correspond, in both studies, the highest values were observed for the key elements related to medication labeling, packaging, and naming (69.2%) and the communication of prescriptions and other medication information (64%). Similarly, the elements with the lowest percentages in both studies were element VIII, related to the competency and training of professionals in medications and safe practices, and element I, concerning the availability of patient information. There is no doubt that these are areas in which the collaborative group from SEFH and SEMES will need to work together to promote the implementation of safe practices. In fact, training in safety within emergency departments has been established by both societies as one of the basic collaborative functions to be developed 20.
When comparing the results of this emergency department study with the general hospital study, it is also noteworthy that the scores obtained for most key elements in emergency departments were generally lower, particularly for element IX on patient education (48.1% vs 58%). Establishing appropriate education programs, though a recommended practice, is hindered by high patient turnover, rushed discharges to free up beds in emergency departments, heavy professional workload, and limited staffing.
The incorporation of clinical pharmacists into emergency care teams is one of the measures that has been shown to have the greatest impact on reducing medication errors in emergency departments21,22. For this reason, several scientific societies of emergency professionals consider it an essential aspect in their units20,23. The low score obtained in this element of the questionnaire requires a strong commitment to incorporating clinical pharmacists as one of the first and foremost steps needed to improve safety in these settings, especially in smaller hospitals, where the questionnaire results show a lower participation of pharmacy services.
The study has several limitations derived from the methodology used. The sample may not be representative of all the emergency departments, as it was not randomly assigned, and, in fact, the services that voluntarily chose to participate in the study might be more aware of medication error prevention, which could have introduced bias in the results. Another aspect limiting the results relates to the completion of the questionnaire. Although the instructions for self-assessment indicate that it should be carried out by a multidisciplinary team familiar with the reality of the emergency department, no control was implemented to verify this. Finally, another limitation to note, inherent to this type of self-assessment tool, is the potential variability in how different items of the questionnaire are interpreted by the teams in each department, which could affect the results.
In summary, this study should promote self-assessment for safe medication practices in emergency services, allowing professionals to understand the degree of implementation in their specific departments and to drive interventions for improvement. Furthermore, the present study has identified several safety practices that are insufficiently implemented in emergency departments across the country, highlighting areas for improvement where planning collaborative initiatives to minimize medication errors in patients treated in these units should be a priority.
Contribution to the Scientific LiteratureThis study provides detailed information on the safety of the medication use systems in emergency departments and quantifies the degree of implementation of safe practices considered essential to avoid the most common errors in this area.
Understanding the highest-risk points in the processes will be highly useful for planning collaborative improvement initiatives among emergency departments.
FundingThe present study was supported by the Spanish Society of Hospital Pharmacy (SEFH).
List of Participating Hospitals and their Respective CoordinatorsAndalusia: M.A. Castro Vida (Hospital Universitario de Poniente, El Ejido, Almería); I. Vallejo Rodríguez (Hospital Universitario San Cecilio, Granada); A. Sánchez Martín, F. Alonso Morales (SU General, Hospital Universitario Virgen de las Nieves, Granada); E. González del Valle, C. González Hervás (SU Pediátrico, Hospital Universitario Virgen de las Nieves, Granada); V. Faus Felipe (Hospital Costa del Sol, Marbella, Málaga); M.T. Serrato Llamas (Hospital Serranía de Ronda, Ronda, Málaga); A. Fernández de Simón Almela, D. Avilés (SU General, Hospital Universitario Virgen del Rocío, Sevilla); C. Álvarez del Vayo, M.J. Sánchez Álvarez (SU Pediátrico, Hospital Universitario Virgen del Rocío, Sevilla).
Aragon: F. Glave Royo, C. López Más (Hospital Obispo Polanco, Teruel); I. Navarro Pardo, M. Arenere Mendoza (Hospital Universitario Lozano Blesa, Zaragoza); J.M. Real Campaña, F.J. Abellán Antolín (SU General, Hospital Universitario Miguel Servet, Zaragoza); V. Gómez Barrena (SU Pediátrico, Hospital Universitario Miguel Servet, Zaragoza); J. Sánchez Melús, M.L. Catalán Ladrón (Hospital Ernest Lluch, Calatayud, Zaragoza).
Asturias: N. Pérez Domínguez, M. Albuerne Sergas (Hospital Universitario San Agustín, Avilés); C. Orallo Luna, C. Calzón Blanco (Hospital Universitario Central de Asturias, Oviedo).
Balearic Islands: J. Martínez Sotelo, F.J. Rodríguez Segura (Hospital de Inca, Mallorca); M. Vilanova Boltó; B. Calderón Herranz (Hospital Universitario Son Llatzer, Palma de Mallorca); M. Prats Riera, A.B. Berzosa Ortega (Hospital Can Misses, Ibiza).
Castile-La Mancha: M.R. Ortiz Navarro (Hospital Universitario de Albacete); E. Palacios Moya, A. Sánchez Cadena (Hospital General Universitario de Ciudad Real).
Castile and León: A.M. López González, J. García Criado (Hospital Universitario de Salamanca); J.A. Jodra Pérez, M.E. Fernández García (Complejo Asistencial de Soria).
Catalonia: J. Martínez Casanova, A. Suarez-Lledó (Hospital Universitari de Bellvitge, Barcelona); J. Ruiz Ramos, M.T. Álvarez Arranz (Hospital de la Santa Creu i Sant Pau, Barcelona); R. López Martínez, M. Arranz Betegón (Hospital Universitari Vall d'Hebrón, Barcelona); A. Ayestarán Altuna, J. Fierro Banzo (SCIAS Hospital de Barcelona); J. Barceló Vidal, I. Cirera Lorenzo (Hospital del Mar, Barcelona); G. García Segarra, N. Pons Llobet (Hospital Universitari Sagrat Cor, Barcelona); V. de Dios Benito, A. Martín Val (Hospital Universitario Germans Trias i Pujol, Badalona, Barcelona); G. Zapata González, A. M. Armero Garrigos (Corporació de Salut del Maresme i la Selva, Calella, Barcelona); V. Arias Constantí, M. Duero Adrados (Hospital Sant Joan de Déu, Esplugues de Llobregat, Barcelona); T. Baeza Ransanz, P. Alonso Castell (Fundación Althaia de Manresa, Barcelona); Y. Campos Baeta (Hospital Sant Joan de Déu, Martorell, Barcelona); J. Ramos Rodríguez, C. Netto Miranda (Hospital Universitari Parc Taulí, Sabadell, Barcelona); L. Val Prat, P. Amorós Reboredo (Hospital General de Catalunya, San Cugat del Vallés, Barcelona); G. Garreta Fontelles (Hospital Universitari Mútua de Terrassa, Barcelona); A. Pérez Plasencia, C. Toro Blanch (Hospital Universitario Josep Trueta, Gerona); M.D. Malla Canet, M. Olmo Martínez (Hospital Santa Caterina, Parc hospitalari Martí i Julià. Salt, Gerona); J.M. Martínez Macías, J. Amores Vilà (Hospital de Palamós, Gerona); A. Morales Portillo, B. Martínez Castro (Hospital Universitario Arnau de Vilanova, Lérida); S. Conde Giner, I. Fonoll Tassier (Hospital Universitari Joan XXIII, Tarragona).
Galicia: M.I. Martín Herranz, S. González Piñeiro (Complejo Hospitalario Universitario de A Coruña); M. I. Pedreira Vázquez, A. M. Montero Hernández (Hospital Arquitecto Marcide, Ferrol, A Coruña); P. Sempere Serrano, P. Mayán Conesa (Complejo Hospitalario Universitario de Santiago de Compostela, A Coruña); R. Iglesias Barreira, C.A. Sandoval Aquino (Hospital Quirón Salud, Lugo); M. Samartín Ucha, A. Pichel Loureiro (Complejo Hospitalario Universitario de Vigo, Pontevedra); N. Ramos González (Hospital do Salnés, Villagarcía de Arosa, Pontevedra).
Madrid: C. Ortega Navarro, M. Vázquez Hernández (Hospital General Universitario Gregorio Marañón, Madrid); Á. García Martín, R. Torres Santos-Olmos (Hospital Universitario La Paz, Madrid); M. Muñoz García, M.J. Zamorano Serrano (Hospital Universitario Ramón y Cajal, Madrid); J.M. Caro Teller, L. Castro Arias (Hospital Universitario 12 de Octubre, Madrid); A. Delgado Latorre, N. López Laguna (Hospital Clínica Universidad de Navarra, Madrid); V. Gómez Tello (Hospital HLA Universitario Moncloa, Madrid); C. Ortega Navarro, S. Cruz Pardos (Hospital Virgen del Mar, Madrid); A. Carrero Fernández, R. Santoloya Perrín (Hospital Universitario Príncipe de Asturias, Alcalá de Henares, Madrid); J.J. Martínez Simón, S. Alonso Rodrigo (Hospital Universitario Fundación Alcorcón, Madrid); Y. Castellanos Clemente, C. Puivecino Moreno (Hospital Universitario de Fuenlabrada, Madrid); M. Hijazi Vega, M.V. Olalla Martin (Hospital Universitario de Getafe, Madrid); E. Díaz Gómez, M.J. Hernández Martínez (Hospital Universitario Severo Ochoa, Leganés, Madrid).
Murcia: C. Caballero Requejo, E. Cánovas (Hospital General Universitario Reina Sofía, Murcia); C. García Motos (Hospital Universitario Morales Meseguer, Murcia); A. Lázaro Cebas, A. Conesa Hernández (Hospital Universitario Santa Lucía, Cartagena, Murcia).
Basque Country: C. Ariz Arnedo, I. Iribar Dieguez (Hospital Bidasoa, Hondarribia, Guipúzcoa); L. Arteche Eguizabal, F. Melgosa Latorre (Hospital Alto Deba, Mondragón. Guipúzcoa); M.I. Fernández González, A.B. Maillo Arana (Hospital de Zumárraga, Guipúzcoa); A. Campino Villegas, M. de Miguel Cascón (Hospital Universitario de Cruces, Baracaldo, Vizcaya); M. Alonso Díez, M. Santisteban Bocos (Hospital Universitario de Basurto, Bilbao, Vizcaya); A. de Juan Arroyo, R. García Díez (Hospital de Urduliz, Vizcaya).
Valencia: C. Matoses Chirivella, J.A. Gutiérrez Navarro (Hospital General Universitario de Elche, Alicante); M. Sáez Bello, D. Castelló García (Hospital Universitaro Dr. Peset, Valencia); A. Rochina Astorga, P. Sánchez Llopez (Hospital de Manises, Valencia).
Andorra: A. Agulló Fenoll, I. Ruiz Vidal (Hospital Nostra Senyora de Meritxell, Andorra).
Liability and Transfer of RightsAll authors accept responsibility as defined by the International Committee of Medical Journal Editors.
In the event of publication, all the authors cede exclusive rights of reproduction, distribution, translation, and public communication (by any means or sound, audiovisual, or electronic support) of this work to Farmacia Hospitalaria and, by extension, to the SEFH.
CRediT authorship contribution statementMaría José Otero: Writing – review & editing, Writing – original draft, Validation, Supervision, Methodology, Formal analysis, Data curation, Conceptualization. Montserrat Alonso Díez: Writing – review & editing, Writing – original draft, Methodology, Investigation, Conceptualization. Helena Esteban Cartelle: Writing – review & editing, Methodology, Investigation. Sonia Jiménez Hernández: Writing – review & editing, Investigation. Iria Miguéns Blanco: Writing – review & editing, Investigation. Marisol Samartín Ucha: Writing – review & editing, Investigation. Rosario Santolaya Perrín: Writing – review & editing, Investigation. Jesús Ruiz Ramos: Writing – review & editing, Writing – original draft, Methodology, Investigation, Conceptualization.
None declared.
We would like to thank all hospital staff who participated in the study for their contributions.