Nuevos roles y retos del farmacéutico de hospital. New roles and challenges of the hospital pharmacist
Más datosHospital Pharmacy is today a profession marked by therapeutic advances, with a proactive attitude, focussed on people and their health. The evolution of processes is constant, with the full presence of digitalisation, robotisation, and even artificial intelligence, in an environment that also requires the efficient and sustainable use of these tools. In this context, it is necessary to have a roadmap that guides the advancement of the profession and Hospital Pharmacy Services.
Continuing with the philosophy of the 2020 initiative which, with the slogan “Towards the future, safely”, defined the strategic lines to advance in the improvement of Hospital Pharmacy practice, the Spanish Society of Hospital Pharmacy wanted to raise the challenges the profession is currently facing and with a view to 2030.
With this strategic planning objective, 20 challenges have been identified and developed, which cover the different areas of action and involvement of Hospital Pharmacy and which cover clinical activities, transversal aspects, training, and research, as well as areas related to people and to the organisations or health systems. For each of them, the objectives, standards, tools, and resources have been defined. It is also planned to provide tools that facilitate monitoring of implementation and the impact on the profession, patients, and the environment.
La Farmacia Hospitalaria es hoy una profesión marcada por los avances terapéuticos, con una actitud proactiva, centrada en las personas y en su salud. La evolución de los procesos es constante, con plena presencia de la digitalización, la robotización e incluso de la inteligencia artificial, en un entorno que además exige el uso eficiente y sostenible de estas herramientas. En este contexto, es necesario contar con una hoja de ruta que guíe el avance de la profesión y de los servicios de farmacia hospitalaria.
Siguiendo con la filosofía de la iniciativa 2020 que, con el lema “Hacia el futuro, con seguridad”, definió las líneas estratégicas para avanzar en la mejora de la práctica de la Farmacia Hospitalaria, la Sociedad Española de Farmacia Hospitalaria ha querido plantear los retos a los que se enfrenta la profesión actualmente y con una mirada hacia el 2030.
Con este objetivo de planificación estratégica se han identificado y desarrollado 20 retos, que cubren las distintas áreas de actuación e implicación de la Farmacia Hospitalaria y que abarcan aspectos asistenciales, transversales, formación e investigación, así como áreas relacionadas con las personas y con las propias organizaciones o sistemas de salud. Para cada uno de ellos se han definido los objetivos, estándares, herramientas y recursos. También está previsto proporcionar herramientas que faciliten el seguimiento de la implementación y del impacto sobre la profesión, los pacientes y el entorno.
Hospital Pharmacy, as originally defined, is a pharmaceutical speciality concerned with serving the pharmaceutical needs of the population through various activities aimed at ensuring the appropriate, safe, and cost-effective use of medications and medical devices for the benefit of patients.1 The core of this definition remains entirely valid. However, our profession has constantly evolved over recent decades and will continue to do so, adapting to the needs and demands of patients, the public, and healthcare organisations.2
In the early days, the main activities of hospital pharmacists included providing information about medications, selecting them, medication procurement, storage, preservation, dispensing, distribution, and pharmacotechnics. Over time, the clinical aspects were expanded to include activities such as the monitoring of artificial nutrition, clinical pharmacokinetics, and clinical trials. At the same time, leadership and management activities became increasingly relevant.2
In recent years, specialisation in pharmaceutical care has broadened in several areas, improving the care of special populations, such as oncology patients, paediatric patients, and outpatients treated with hospital-prescribed medications. Even more recently, this trend has also extended to areas such as infectious diseases, critical care, and emergencies. These developments in the activities of specialist pharmacists have been accompanied by changes in technological resources and innovation that impact healthcare, reflecting the various advances taking place in our environment.3
Currently, we find ourselves in a profession characterised by therapeutic advances, focussed on providing proactive, collaborative, and humanised care centred on people and their health. We are witnessing a continuous reformulation of processes that integrate digitalisation, robotics, and artificial intelligence, along with the challenge of using all these tools efficiently and sustainably. Against this background, it is essential to have available a roadmap to advance the profession and Hospital Pharmacy Services (HPSs).
The importance of having a roadmap. Initiatives in our environmentStrategic planning is increasingly common in organisations, including healthcare systems, hospital centres, or clinical services and units. A roadmap provides an orderly and systematic way of outlining the steps needed to move from the current situation to the desired future situation.4,5
In a constantly changing environment, it is crucial to plan the strategy to be followed. We now find ourselves in an environment previously described by experts as "VUCA" (volatile, uncertain, complex, and ambiguous), but which the coronavirus pandemic transformed into a "BANI" (brittle, anxious, non-linear, and incomprehensible) world.6 In this setting, informed individuals and competent trained professionals are caught up in a seemingly unstoppable technological and knowledge revolution, in the midst of complex health system funding models, and with the concept of "One Health" more present than ever.
Aware of the importance of planning for progress, in 2008, a group of hospital pharmacists worked on the Initiative 2020 project. Under the slogan "Towards the future, safely", they defined 6 strategic lines and the keys to progress in improving Hospital Pharmacy practice and healthcare systems. The project was presented at the 53rd National Congress of the Spanish Society of Hospital Pharmacy (SEFH) and became an open and shared tool for all Hospital Pharmacy professionals.7
Based on the general principles of strategic planning, Initiative 2020 was articulated by defining objectives for each of the 6 strategic lines, totalling 28 in all. Information on the baseline situation for the year 2010 was provided along with cross-references and literature of interest for each objective. The aim was to significantly improve HPSs in 6 areas7:
- 1.
Organisational development: To incorporate new technologies to improve the organisation and quality of pharmacy services, as well as the safety and comprehensive care of patients in the pharmacotherapeutic process.
- 2.
Scientific evidence in clinical practice: To increase the degree to which hospital pharmacists apply the principles of evidence-based medicine to improve individualised pharmacotherapy.
- 3.
Safety practices: To lead, develop, and implement actions to improve the safety of the system for the use of medications in hospitals.
- 4.
Pharmaceutical care: To increase the involvement of pharmacists in optimising individualised pharmacotherapy.
- 5.
Teaching: To develop individualised professional development programmes for pharmacists and pharmacy service technicians, and to expand teacher-training programmes.
- 6.
Research: To increase the scientific contributions of hospital pharmacists.
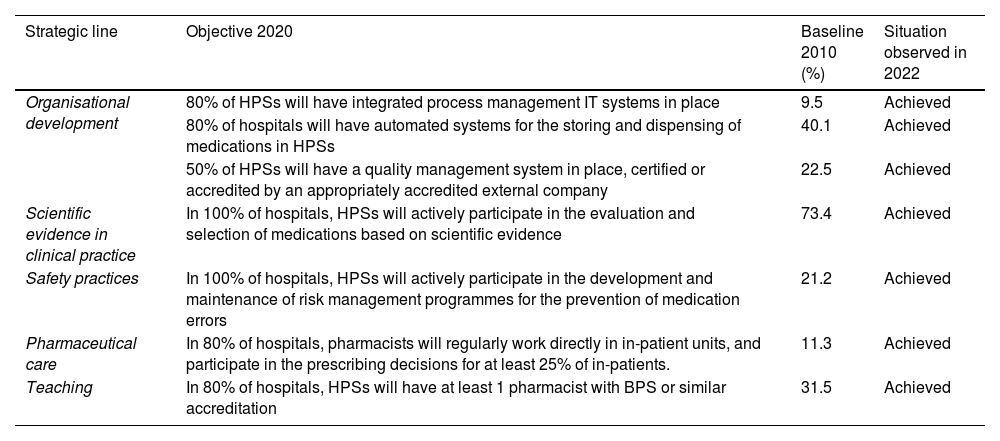
Initiative 2020 has been widely used by HPSs to deploy their strategic lines and objectives. Its scope has not been systematically measured, but the White Paper on Hospital Pharmacy—which outlines the situation of the services in terms of infrastructure, resources, and activity—describes the advances achieved.8 Thus, Table 1 shows some of the objectives of Initiative 2020, the baseline situation reported in 2010, and the situation observed in 2022.7,8
Examples of 2020 targets, the baseline situation reported in 2010, and the situation observed in 2022.
| Strategic line | Objective 2020 | Baseline 2010 (%) | Situation observed in 2022 |
|---|---|---|---|
| Organisational development | 80% of HPSs will have integrated process management IT systems in place | 9.5 | Achieved |
| 80% of hospitals will have automated systems for the storing and dispensing of medications in HPSs | 40.1 | Achieved | |
| 50% of HPSs will have a quality management system in place, certified or accredited by an appropriately accredited external company | 22.5 | Achieved | |
| Scientific evidence in clinical practice | In 100% of hospitals, HPSs will actively participate in the evaluation and selection of medications based on scientific evidence | 73.4 | Achieved |
| Safety practices | In 100% of hospitals, HPSs will actively participate in the development and maintenance of risk management programmes for the prevention of medication errors | 21.2 | Achieved |
| Pharmaceutical care | In 80% of hospitals, pharmacists will regularly work directly in in-patient units, and participate in the prescribing decisions for at least 25% of in-patients. | 11.3 | Achieved |
| Teaching | In 80% of hospitals, HPSs will have at least 1 pharmacist with BPS or similar accreditation | 31.5 | Achieved |
Another example of strategic planning, which served as a model or inspiration for Initiative 2020, was the 2015 Initiative of the American Society of Health-System Pharmacists (ASHP), which later evolved into the still current ASHP Practice Advancement Initiative 2030 (PAI 2030).9,10 The 2015 Initiative was conceived as a collaborative effort to improve pharmacy practice in US hospitals and health systems, and included 6 goals and 31 specific objectives, which were expected to be achieved by 2015. The initiative as a whole was based on the expectation that hospital pharmacists would shift their activities toward direct patient care and that pharmacy services would focus on continuous quality improvement.
PAI 2030, which is still underway, provides tools and resources to advance the profession over the next decade, with the aim of focussing change at a local level and providing resources to ensure that the profession responds to the needs of the future and various models of patient care.11 The initiative is structured into 5 areas or domains: patient-centred care; the role, education, and training of pharmacy technicians (PTs); the role, education, and training of pharmacists; technology and data science; and leadership in medication use and safety. It includes 59 recommendations focussing on practices, organisations, and the profession, and identifies the following issues as priorities for change:
- •
Optimise care via comprehensive pharmacotherapeutic management provided by pharmacists.
- •
Integrate pharmacy activities for cost-effective care.
- •
Increase public health opportunities.
- •
Advance PT roles.
- •
Incorporate personalised therapies.
- •
Harness data analytics to improve patient health.
The PAI 2030 project also identifies 5 main initiatives (focussed initiatives) within the scope of the 5 domains mentioned, each with an objective and measurable outcomes. It also includes success stories, resources for students and teachers, periodic reports, and self-assessment tools.
The Spanish Society of Hospital Pharmacy 2030 projectThis national and international backdrop, ongoing advances in Hospital Pharmacy, and an ever-changing healthcare ecosystem prompted the development of the 2030 project within the SEFH. In line with the philosophy of Initiative 2020, the aim of the 2030 project is to provide pharmacy services with an updated roadmap to improve Hospital Pharmacy practice in our environment. It is important to emphasise that the project has been designed from the outset to be dynamic and able to adapt to and incorporate changes as they occur.
The aim of the SEFH 2030 project is to establish strategic lines and characterise key challenges that will facilitate advancements in improving Hospital Pharmacy practice and health systems; it also aims to propose resources and action plans that can help in the implementation and monitoring process. In this sense, work has been done to help all pharmacy services—regardless of their resources and the type of hospital to which they belong—to develop and advance in line with the needs of patients and the environment.
The project was developed through the creation of a coordinating group and a working team made up of colleagues from various pharmacy services and experts from different fields of knowledge. To characterise the challenges, the working team was divided into different groups, with each group concentrating on 1 or 2 of them, with other professionals providing guidance or advice as required.
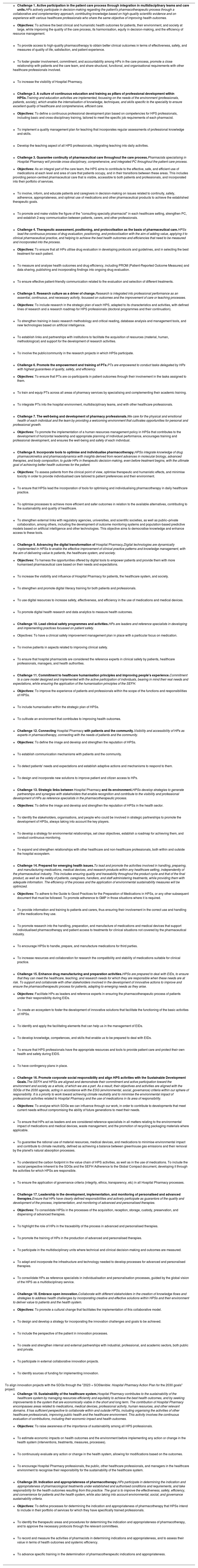
As a starting point, in the initial phase, the 30 SEFH working groups were consulted regarding the identification of the challenges facing pharmacy services in the coming years. From this point onward, after reviewing the strategic lines and the degree of achievement of the objectives of the 2020 group, the coordinating group developed a proposal and selection process that identified a total of 20 challenges for further characterisation. Table 2 shows the 20 challenges that form part of the project.
Challenges of the Spanish Society of Hospital Pharmacy 2030 project (challenges, definitions, and objectives).
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| To align innovation projects with the SDGs through the "2023 + SOStenible: Hospital Pharmacy Action Plan for the 2030 goals" project. |
|
|
|
|
|
|
|
|
PC, pharmaceutical care; HP, hospital pharmacist; SDG, sustainable development goals; EID, emerging infectious disease; SEFH, Spanish Society of Hospital Pharmacy; HPS, Hospital Pharmacy Service; PT, pharmacy technician.
The challenges identified and characterised cover the different areas of action and involvement within Hospital Pharmacy, envisioning its evolution and potential for the upcoming years. The complete document is available for consultation.12 These challenges encompass aspects of healthcare tasks, including the participation of patients in multidisciplinary teams through the use of integration models, the healthcare continuum, therapeutic optimisation, and individualisation, the development and monitoring of advanced therapies, and the determination of pharmacotherapeutic indications and appropriateness. The challenges also relate to multidisciplinary activities, such as drug evaluation and positioning, clinical safety, and drug development and manufacturing.
The project addresses training and research as pillars of development and drivers of change, and includes challenges related to people (professionals and the public), addressing aspects of well-being and development, technician training, humanisation of healthcare, and connections between Hospital Pharmacy, patients, and the community. Finally, the project also addresses challenges focussed on the healthcare organisations or systems themselves, such as digital transformation and innovation, local partnerships, readiness for emerging health problems, corporate social responsibility, integration of sustainable development goals, and the sustainability of the healthcare system itself.
The following elements were defined when characterising each challenge:
- •
Definition of the challenge.
- •
Objectives: Oriented from 3 perspectives (professional, patient, environmental).
- •
Standards.
- •
Tools and resources: Structured by training, research, technology, and human resource and process management.
- •
Scientific evidence and success stories.
The objectives attempt to answer the following question: What must be done to make it happen, and bring together the actions considered necessary to advance from the current situation to the desired future state. The standards address the question: How are we going to do it? They bring together a set of proposals for achieving the desired situation by 2030. Both the objectives and the standards have been proposed taking into account the diversity of our healthcare system and the differences between the different hospitals and their pharmacy services.
By way of example, we now outline some elements of the challenge of clinical safety—one of the pillars of our profession—in accordance with the guidelines of the World Health Organisation, which considers patient safety a fundamental right in healthcare.13 In this context and with this vision of the present and the future, the challenge of leading clinical safety programmes and activities is taken on, such that hospital pharmacists are reference specialists in the development and implementation of practices focussed on patient safety.
The objectives are to have a management plan for improving clinical safety, with a particular focus on medication; to involve patients in aspects related to improving clinical safety; and to ensure that hospital pharmacists are seen as reference specialists for clinical safety by patients, healthcare professionals, managers, and healthcare authorities. To this end, the following standards have been agreed:
- •
The HPSs have a comprehensive electronic prescribing system integrated with clinical information systems and decision-support elements in all healthcare settings.
- •
The pharmaceutical validation of prescriptions is conducted prior to dispensing and/or administration, particularly for high-risk medications.
- •
The dispensing and administration of the medication associated with the prescription is recorded electronically, with unambiguous identification of patient and medication, at least in high-risk units.
- •
Systems are implemented to improve traceability, quality, and safety throughout the entire drug use circuit: acquisition–prescription–validation–processing–dispensing–administration.
- •
The processes for the preparation and administration of injectables are standardised in the hospital, following the guidelines of the Guide to Good Practice in the Preparation of Medicines, promoting their centralised preparation in the pharmacy services.
- •
High-risk medications available in the facility are clearly identified alongside error prevention practices in all processes.
- •
The HPSs have an updated and standardised procedure to facilitate medication reconciliation during care transitions, particularly for chronic patients with polymedication and/or being treated with high-risk medications.
- •
Clinical pharmacists are integrated into care teams, at least in units treating high-risk patients.
- •
HPSs develop and implement patient education programmes to encourage their active participation in treatment.
- •
Periodic evaluation (at least every 3 years) of medication use systems, using questionnaires or other self-assessment tools, to identify risks in the processes and to prioritise and incorporate improvement measures.
Regarding the tools and resources needed to achieve the 2030 objectives, aspects such as training, research, technology, human resource management, and process-related issues have been taken into consideration. Teaching resources include the inclusion of safety training into the induction plans for new professionals, active participation in clinical safety committees, the implementation of continuous safety education plans, and patient participation in safety aspects of the care process. Within the area of research-related tools, it is recommended to evaluate the impact of the safety practices implemented and their healthcare outcomes.
Technological resources focus on information systems, comprehensive electronic prescribing, automation, intelligent infusion pumps, and quality control. In terms of human resource management, the figure of the clinical safety leader, second-victim programmes, and patient involvement are now focuses of attention. Finally, regarding processes, challenges include promoting a safety culture, establishing reporting and analysis systems, obtaining quality accreditations, and identifying and implementing safe practices.
Any strategic project needs tools to facilitate its implementation in a way that is both practical and adapted to real-world conditions, as well as regular monitoring of its impact to ensure that it is achieving the desired developments in the target groups. For this reason, in addition to characterising the challenges, a self-assessment tool has been designed, modelled on other similar questionnaires already known in our setting.14 We hope that this questionnaire will be a useful tool for pharmacy services, enabling progress toward meeting the challenges.
Using the questionnaire, each pharmacy service will be able to take the pulse of its situation, identify areas for development, and decide which challenges to prioritise. It will help to establish a concise and realistic roadmap, as well as specify the actions to be taken, and measure their progress over time. The questionnaire is based on the standards established for each challenge, as they outline the actions required to meet them, while providing different response options based on the degree of development or implementation of each standard. In summary, the questionnaire is intended to serve as an improvement and planning tool, assisting HPSs in their efforts to improve their service portfolio and the overall value of their activities.
ConclusionsThe 2030 Project addresses the need for a roadmap for HPSs to strategically plan their development, ensuring they can meet the needs of society, organisations, and the environment, while taking into consideration the ongoing changes and advances that are taking place in the healthcare ecosystem. The challenges identified and characterised relate to the different areas of action of Hospital Pharmacy, with the aim of achieving the best health outcomes for the community, along with the commitment to safeguard the sustainability of the system, while taking into account the reality of our environment in the current decade.
Ethical responsibilitiesThe instructions for manuscript submission and all ethical responsibilities have been fulfilled.
FundingNone declared. The 2030 project of the Spanish Society of Hospital Pharmacy (SEFH) was funded directly by the scientific society itself. The authors of the article declare no financial support related to the project.
CRediT authorship contribution statementEdurne Fernández de Gamarra-Martínez: Writing – review & editing, Writing – original draft, Methodology, Conceptualization. Begoña Tortajada-Goitia: Writing – review & editing, Writing – original draft, Methodology, Conceptualization. Juan José Corte-García: Writing – review & editing, Writing – original draft, Methodology, Conceptualization. Isabel Martín-Herranz: Writing – review & editing, Writing – original draft, Methodology, Conceptualization. Mario García-Gil: Writing – review & editing, Writing – original draft, Methodology, Conceptualization. Javier Sáez de la Fuente: Writing – review & editing, Writing – original draft, Methodology, Conceptualization. Jordi Nicolás-Picó: Writing – review & editing, Writing – original draft, Methodology, Conceptualization.
The project was made possible thanks to the selfless collaboration of all colleagues involved in the working groups for each challenge. The SEFH working groups, as well as the SEFH Board of Directors and Governing Boards, also collaborated with their contributions.