Intensive Care Units (ICU) are recognized as high-risk settings for medication errors, primarily due to the complex pharmacological regimens and the critical condition of patients. It is estimated that the probability of errors occurring in these units is two to three times higher than in general hospital patients, with prescribing and administration being the stages most frequently associated with such incidents.
ObjectiveTo evaluate the applicability and satisfaction with electronic prescribing systems in Intensive Care Units of hospitals in Spain.
MethodsA nationwide survey was conducted targeting pharmacists to assess the functionalities of the electronic prescribing systems used in these units. The evaluation covered hospital characteristics, features of the prescribing software, and healthcare professionals' satisfaction, with the aim of understanding the current situation and proposing improvement strategies to enhance medication safety through prescribing systems in the context of critically ill patients.
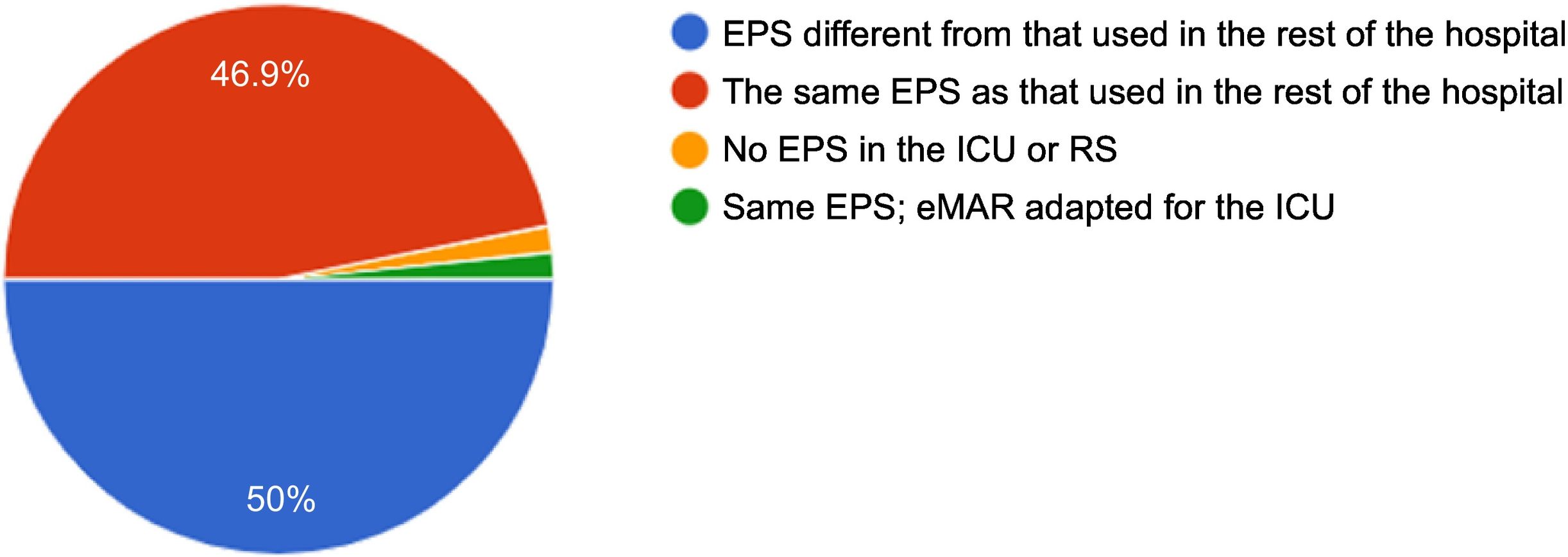
ResultsA total of 64 surveys were completed across 55 different hospitals. In 50.8% of cases, a prescribing system different from that used in general hospital wards was employed. In 84.4% of cases, the system had been developed by a commercial vendor. In 65.1% of hospitals, the system enabled communication with the pharmacy, and in 57.7% it allowed for pharmaceutical validation. However, 50.8% of the systems were not capable of interfacing with automated dispensing or administration systems. In 71.9% of cases, the system allowed for direct data extraction. Pharmacists reported satisfactory overall perceptions in only 43.8% of cases, while 42.9% identified unmet needs requiring improvement.
ConclusionsDespite significant heterogeneity in the functionalities of electronic prescribing systems across Spanish ICUs, such systems are widely implemented nationwide and are regarded as a key element in ensuring medication safety within these units. Clinical pharmacists reported a generally acceptable level of satisfaction; however, there remains considerable scope for improvement.
las unidades de cuidados intensivos (UCI) se consideran espacios de alto riesgo para que se produzcan errores de medicación debido a las condiciones específicas de utilización de los fármacos y al estado crítico de los pacientes. Se estima que en estas unidades la probabilidad de que se produzca un error es de 2 a 3 veces mayor respecto a las salas de hospitalización, siendo en los procesos de prescripción y administración las etapas en las que más incidentes se producen.
Objetivoevaluar la aplicabilidad y la satisfacción de los sistemas de prescripción electrónica en las UCI de los hospitales en España.
Métodosse realizó una encuesta a nivel nacional dirigida a farmacéuticos para conocer las funcionalidades del sistema de prescripción electrónica utilizado en estas unidades, en el que se evaluaron las características del hospital, del programa de prescripción y la satisfacción por parte del personal sanitario, con el objetivo de conocer el estado actual y proponer acciones de mejora en la seguridad del medicamento a través de los sistemas de prescripción en el ámbito del paciente crítico.
Resultadosse completaron 64 encuestas por 55 hospitales diferentes. El 50,8% disponían de un programa de prescripción diferente al utilizado en el resto de plantas de hospitalización. En el 84,4% de los casos, se trataba de un programa desarrollado por un promotor comercial. En el 65,1% el programa permitía la comunicación con farmacia y en un 57,7%, la validación farmacéutica; sin embargo, el 50,8% no era capaz de comunicarse con sistemas automáticos de dispensación o administración. En el 71,9% era posible la explotación directa de datos desde el sistema. La percepción por parte del farmacéutico fue satisfactoria únicamente en 43,8%, y en 42,9% describió necesidades de mejora no cubiertas.
Conclusionesa pesar de existir una gran heterogeneidad en las funcionalidades de los sistemas de prescripción electrónica en las UCI españolas, están instaurados en gran parte del territorio nacional como un elemento clave de seguridad respecto al manejo de los medicamentos en estas unidades. La satisfacción por parte del farmacéutico clínico es adecuada; sin embargo, existe aún un amplio margen de mejora.
Patients admitted to intensive care units (ICUs) are at a higher risk of medication errors (MEs) and adverse events than patients admitted to conventional hospital units. This increased risk arises from multiple factors, including the use of complex regimens involving numerous, often high-risk, medications; the high proportion of parenteral medications; the need for complex calculations; pathophysiological alterations requiring continuous treatment adjustments; and the severity of the diseases being treated.1,2 In these units, MEs may include errors in dosage, frequency, or route of administration; misinterpretation of medical orders; omission of previously prescribed medications; lack of review before transcription; labelling errors; or incorrect reconstitution.3
In this context, electronic prescribing systems (EPSs) have been shown to significantly reduce the incidence of MEs, with this effect persisting in the long term after their adoption, although it may not be apparent in the short term.1 These systems facilitate the rapid and accurate transmission of patient information and the standardisation of medical procedures. They can also incorporate clinical decision support tools aimed at promoting safe pharmacotherapy.4
However, implementing these systems in ICUs poses significant challenges, including data overload, inaccurate software, a lack of integration between systems, and the need to adapt them to the healthcare workers' routines.5 Furthermore, electronic interventions have not been shown to have a significant effect on mortality, length of hospital stay, or cost. This may be due to the small number of studies available for combined analysis, given the significant variations in populations, interventions, and outcome measures used.6 In addition to the initial financial investment, these systems require ongoing maintenance to meet the needs arising from their daily use by doctors, pharmacists, and nursing staff.7 The lack of standardisation of EPSs remains a significant challenge, highlighting the need for up-to-date guidelines or protocols in place to facilitate their design and implementation in hospitals that require them.8 In this context, clinical pharmacists have taken on an increasingly important role in identifying and resolving problems associated with electronic prescribing, which can be adapted to the workflow applied in ICUs.9
The aim of this study was to evaluate the applicability of and satisfaction with EPSs in Spanish ICU settings, describe their characteristics and their degree of integration with other systems, assess hospital pharmacists' perceptions of their usefulness, and identify areas for improvement.
Materials and methodsStudy design and contextAn online survey was designed for hospital pharmacists working in ICUs to describe the characteristics of the EPS software implemented in these units. The project was co-led by the Pharmacists in Intensive Care and Critical Patients Working Group (FarMIC) and the New Technologies and Digital Hospital Pharmacy Working Group (DIGIFHAR) of the Spanish Society of Hospital Pharmacy (SEFH).
A descriptive, cross-sectional, multicentre study was conducted using the online survey to identify the characteristics of ICU software.
Population and sampleThe target population comprised hospital pharmacists working in public, subsidised, or private hospitals in Spain. A non-probability convenience sample was used, comprising professionals who voluntarily responded to the survey between January 7 and February 7, 2025.
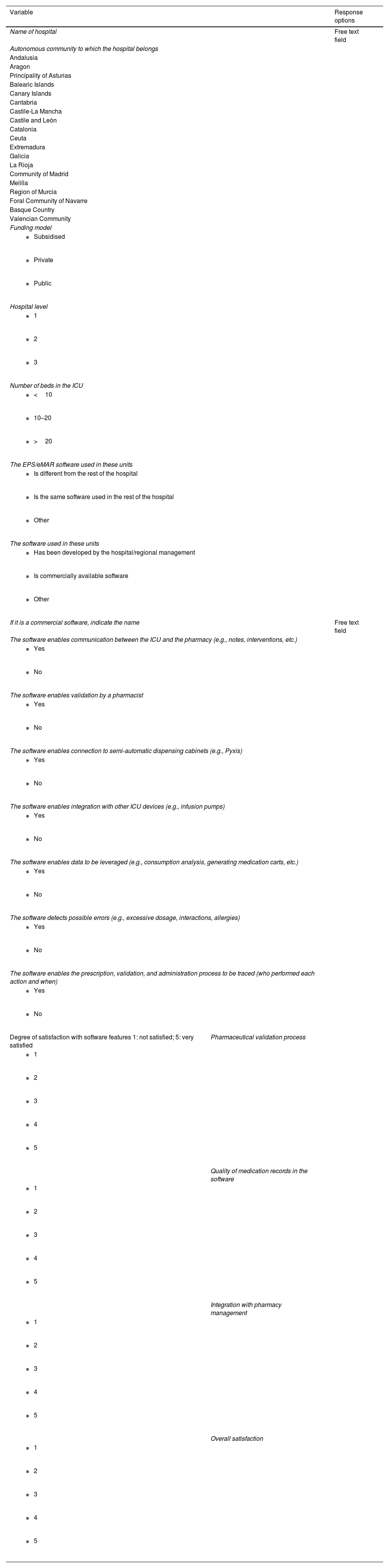
Data collectionThe questionnaire comprised 3 sections, which collected the following data (Table 1):
- (1)
Hospital characteristics: location; funding model; hospital level (first level: <200 beds; second level: 200–500 beds; and third level > 500 beds); and number of ICU beds. The cluster classification was applied to data from the National Hospital Catalogue in order to determine hospital level.10
- (2)
Characteristics of the EPS: software developer; description of its applicability in the pharmaceutical validation process; multidisciplinary communication; capacity for integration with other electronic devices; and safety.
- (3)
Satisfaction with the EPS in terms of data recording, software quality, and overall satisfaction.
Questionnaire used in the survey.
| Variable | Response options | |
|---|---|---|
| Name of hospital | Free text field | |
| Autonomous community to which the hospital belongs | ||
| Andalusia | ||
| Aragon | ||
| Principality of Asturias | ||
| Balearic Islands | ||
| Canary Islands | ||
| Cantabria | ||
| Castile-La Mancha | ||
| Castile and León | ||
| Catalonia | ||
| Ceuta | ||
| Extremadura | ||
| Galicia | ||
| La Rioja | ||
| Community of Madrid | ||
| Melilla | ||
| Region of Murcia | ||
| Foral Community of Navarre | ||
| Basque Country | ||
| Valencian Community | ||
| Funding model | ||
| ||
| ||
| ||
| Hospital level | ||
| ||
| ||
| ||
| Number of beds in the ICU | ||
| ||
| ||
| ||
| The EPS/eMAR software used in these units | ||
| ||
| ||
| ||
| The software used in these units | ||
| ||
| ||
| ||
| If it is a commercial software, indicate the name | Free text field | |
| The software enables communication between the ICU and the pharmacy (e.g., notes, interventions, etc.) | ||
| ||
| ||
| The software enables validation by a pharmacist | ||
| ||
| ||
| The software enables connection to semi-automatic dispensing cabinets (e.g., Pyxis) | ||
| ||
| ||
| The software enables integration with other ICU devices (e.g., infusion pumps) | ||
| ||
| ||
| The software enables data to be leveraged (e.g., consumption analysis, generating medication carts, etc.) | ||
| ||
| ||
| The software detects possible errors (e.g., excessive dosage, interactions, allergies) | ||
| ||
| ||
| The software enables the prescription, validation, and administration process to be traced (who performed each action and when) | ||
| ||
| ||
| Degree of satisfaction with software features 1: not satisfied; 5: very satisfied | Pharmaceutical validation process | |
| ||
| ||
| ||
| ||
| ||
| Quality of medication records in the software | ||
| ||
| ||
| ||
| ||
| ||
| Integration with pharmacy management | ||
| ||
| ||
| ||
| ||
| ||
| Overall satisfaction | ||
| ||
| ||
| ||
| ||
| ||
EPSs, electronic prescribing system; eMAR, electronic medication administration record; ICU, intensive care unit.
Section 1 collected data using a nominal (categorical) scale. Sections 2 and 3 used quantitative scales, with some items in a dichotomous format (yes/no) and others using a numeric scale ranging from 1 to 5.
ProcedureThe questionnaire was distributed to hospital pharmacists through the SEFH mailing list. An initial invitation was sent at the beginning of the study period, followed by a reminder email on day 21. Participation was voluntary and anonymous, with a deadline of 1 month.
To ensure respondent confidentiality and the storage of population data, the survey was conducted using questionnaires created using Google Forms.
Data analysisThe data obtained were analysed using descriptive statistics, including measures of central tendency and dispersion of quantitative variables. Categorical variables are expressed as absolute and relative frequencies. A Likert scale11 was used to assess satisfaction with the software. The results were also analysed based on ICU size—categorised as small (<10 beds), medium (10–20 beds), or large (>20 beds)—applying the chi-square test for dichotomous qualitative variables or analysis of variance for continuous variables. A P-value of ≤0.05 was used as a cutoff for statistical significance. All statistical analyses were conducted using STATA v.14.2.
ResultsA total of 64 completed surveys were received from 55 hospitals across Spain. The main autonomous communities to respond were Catalonia (18.8%), Andalusia (15.6%), Valencia (14.1%), and Castile and León (9.4%). When analysing hospital and software characteristics, the percentages were calculated based on the total number of hospitals (n = 55). The results from the user perception and satisfaction sections were based on the total number of surveys received (n = 64).
Hospital characteristicsOf the 55 participating hospitals, 84.4% were publicly owned, with 76.6% being tertiary hospitals, 21.9% secondary hospitals, and 1.6% primary hospitals. In total, 62.5% of the hospitals had ICUs with more than 20 beds, 31.3% had ICUs with between 10 and 20 beds, and 6.2% had ICUs with 10 beds or fewer.
Software characteristicsThis section provides details of the responses from the 55 participating hospitals regarding the software. Of the hospitals that responded, 50.8% had EPS software for the ICU that differed from that used elsewhere in the hospital. At the time of the survey, only 1.6% of the hospitals reported not having an EPS (Fig. 1).
In 84.4% of cases, the software was developed by commercial companies. The main EPS software used in the ICUs was ATHOS-prisma, Farmatools, PICIS-Critical Care, MetaVision-sicca, ICCA, and FARHOS visual-limes.
Dichotomous questions were used to assess the usability and applicability of the EPSs. Of the participating hospitals, 65.1% reported that their software enabled direct communication between ICU and pharmacy services; 57.8% that it enabled prescription validation by a specialist pharmacist; 50.8% that it did not support communication with automatic dispensing systems; and 54.0% that it was not integrated with ICU devices (e.g., drug infusion systems). Overall, 71.9% of respondents confirmed that health data from EPSs could be used, 57.1% that the EPSs adequately detected errors in drug prescriptions (e.g., excessive doses, interactions, allergies), and 87.5% reported that their computer software could trace the healthcare personnel involved in the prescription, validation, and administration processes. No significant differences were found in relation to ICU size regarding the use of software different from that used in other hospital wards (p = 0.699), the use of commercial software (p = 0.322), the potential for direct communication with the pharmacy service (p = 0.239), or the capacity for pharmaceutical validation (p = 0.721). No differences were found regarding the potential to connect to automated dispensing cabinets (p = 0.538), smart administration pumps (p = 0.487), or export management data (p = 0.970).
User perception and satisfactionA Likert scale1–5 was used to assess user perception and satisfaction among hospital pharmacists. A total of 43.8% reported satisfaction4,5 with the EPS in the pharmaceutical validation process, whereas 39.1% suggested that improvements were needed.1,2 Regarding the quality of the documentation for prescribed medicines, 56.3% reported satisfaction,4,5 while 17.2% suggested that improvements were needed in this area.1,2 In relation to the process of integrating the EPS with the pharmacy, 31.7% reported a high level of satisfaction4,5 with the interoperability of the prescribing software and pharmacy software, while 42.9% noted a need for improvement that remained unaddressed. Finally, overall satisfaction among hospital pharmacists with the EPSs used in Spanish ICUs was 3.07 out of 51–5 (Fig. 2).
DiscussionThe results of this study reflect the perspective of hospital pharmacists on the implementation of EPSs in Spanish ICUs. According to the survey results, the use of EPSs in Spanish ICUs varies considerably between regions and hospitals in terms of implementation, software interoperability, and ease of use. In half of the cases, the EPSs are specific to ICUs and differ from those used in other hospital units.
The most frequent errors reported in ICUs occur during the prescription stage, followed by errors during administration.12 Incorporating new technologies is a key element to improving quality and safety in the strategy to reduce medication-related errors in these stages.13 The PREVEMED study14 focused on the ICUs of 112 Spanish hospitals, showing that a lack of technology was the most common cause of MEs (very frequent: 16.7%; frequent: 14.6%), even though 77.1% of the services had an EPS.
The Institute for Safe Medication Practices recommends implementing medication traceability systems, including EPSs with clinical decision support, electronic systems for preparing medications, automated dispensing systems, electronic administration records, barcode medication administration, and smart pumps for parenteral drug administration. These systems should be integrated with clinical information systems to help improve the safety, effectiveness, and efficiency of medication use in all ICUs.13 However, our study shows that these objectives are not being achieved at the national level in Spain. These results are consistent with those of a Spanish study involving 40 ICUs, which used a self-assessment questionnaire on safe medication practices and evaluated the adoption of new technologies in these units.15 It showed that, although a high percentage of hospitals had an EPS, only 37.5% of these were connected to the medical record or prescription system, and less than half (43.3%) of the EPSs incorporated support for clinical decision-making. It should be noted that the implementation of EPSs in ICUs is comparable to that in other specialised units, including emergency services, where 59% have EPSs with clinical decision support systems.16
Another important aspect is interoperability and integration with other healthcare systems. This is because, in half of the cases, the EPS software used in ICUs differs from that used in other hospital units, reflecting the special characteristics of ICUs (Fig. 1). The EPS must be able to communicate with electronic medical records, automated dispensing systems, or administration systems. However, more than half of ICUs do not have automated dispensing cabinets, and 40% are not connected to an EPS.14 These results are similar to ours: half of the respondents reported that their system does not allow communication with automated dispensing systems or smart administration devices. To achieve integration, the medication catalogue must be connected to the medical record and the automated dispensing system software, and recorded prescriptions and administrations must be transferred to the medical record. The latter aspect ensures that a complete record is kept of all drugs administered during the patient's stay in critical care, thereby facilitating medication reconciliation during care transitions. Given the specific characteristics of critically ill patients and the complexity of their treatment, improving this aspect is crucial for enhancing safety and reducing medication administration errors.
Furthermore, clinical pharmacists play a key role in ensuring the safe use of medication in ICUs. Their integration into multidisciplinary teams has been shown to reduce errors, adverse events, and mortality rates. One of the most important tasks for pharmacists in ICUs is to proactively validate prescriptions.17,18 Our results show that while 65.1% of respondents reported that direct communication with pharmacies was possible, only 57.8% said that the software enabled pharmaceutical validation. These results are consistent with those of the PREVEMED study, which found that 77.1% of units had an EPS and that 67.6% had software integrated with the pharmacy for prescription validation. The latter task was available 24 h a day in 35% of these units.
Regarding user perceptions, the PREVEMED study found that 62.9% of respondents considered that electronic prescribing had significant potential to prevent MEs in ICUs.14 However, our study highlights potential areas for improvement, mainly in terms of the software's capacity for pharmaceutical validation and its interoperability with specific pharmacy service software. It should be noted that the survey targeted hospital pharmacists, who reported a neutral level of satisfaction with the software used for prescribing in ICUs.
One of the strengths of the survey is that it highlights the capacity of the EPS software to leverage data. This enables pharmacists to access relevant information to measure indicators, improve medication management, reduce costs, enhance safety, and continuously evaluate current processes. These are all essential actions for pharmacists working in ICUs.
In terms of the applicability of our study and its potential impact on clinical practice, we emphasise that our results can be used to optimise the pharmaceutical validation process, thereby promoting more consistent and efficient, validating prescription standards in ICU environments. The study identifies common issues, including the lack of integration with dispensing and infusion systems, thus highlighting priority areas that need to be addressed to improve the safety and traceability of medications used in ICUs. The results can also serve as a basis for establishing digital transformation plans that can be applied in local or regional settings and that align clinical objectives with health policies for digitisation and process automation. In this regard, the FarMIC and DIGIFHAR working groups of the SEFH could establish recommendations or technical guidelines. The level of satisfaction among ICU pharmacists with EPSs could serve as an indirect measure of their quality and safety.
A limitation of the study is that only 1.6% of the hospitals reported not having an EPS. However, the sample may not be fully representative, since Spanish hospitals without an EPS may have opted not to participate in the study. Additionally, these hospitals were predominantly regional, which highlights the disparity in the implementation of this type of software. It should also be noted that the questionnaire's reproducibility was not validated, and that variability in the interpretation of the different items could have affected the results.
In conclusion, the results of this survey show that the availability of EPSs is a key factor in ensuring quality and safety. Despite considerable variability, EPSs are implemented in most Spanish ICUs, thereby contributing to the reduction of medication-related errors. While hospital pharmacists are generally satisfied with electronic prescribing EPS software, significant opportunities for improvement remain.
Declaration of membership of SEFH working groupsEduardo Tejedor-Tejada and Maria Jesús Jimenez Cerezo are members of the Working Group on New Technologies and Digital Hospital Pharmacy (DIGIFHAR). Esther Domingo Chiva, Miguel Ángel Amor García and María Martín Cerezuela are members of the Working Group on Intensive Care and Critical Care Pharmacists (FarMIC).
None declared.