To provide a practical guide for the implementation and use of Pharmaceutical Care through Telepharmacy by healthcare professionals and patients in its different scopes of application. To establish a definition of Telepharmacy and describe the technological tools necessary, advantages, and keys to facilitating its implementation.
MethodBetween December 2020 and January 2021, the Board of Directors of the Spanish Society of Hospital Pharmacy, along with the coordinators of the project “Outpatient Care Strategies” (“Mapa Estratégico para la Atención al Paciente Externo”) designed a strategy to foster the development and expansion of Telepharmacy in Spain. This strategy involved four courses of action. To develop the first course of action, a call was made in March 2021 among the Spanish Society of Hospital Pharmacy members to develop seven methodological guidelines. The purpose of these documents was to meet the needs for the implementation of Telepharmacy, the most relevant being the development of specific guides for professionals and patients. The guides were developed in four stages between May and October 2021, including a literature review; consensus-based interviews, online workshops, and, finally, the drafting and validation of the final documents. Once the final draft was prepared, a public evaluation of suggestions and observations was performed for a month. The documents were also presented to the Patient Committee of the Spanish Society of Hospital Pharmacy.
ResultsThe Guide for Professionals provides guidelines for the development and implementation of Telepharmacy in its different scopes of application. These guides provide a description of specific goals, healthcare benefits, tools required, and keys to the implementation of Telepharmacy. The Guide for Patients is complementary to face-to-face pharmaceutical care from the point of view of the patient, with special emphasis being placed on the most frequently used tools, the potential benefits, and the keys to facilitating patients’ understanding of the purpose and use of Telepharmacy.
ConclusionsA Practical Guide for Professionals and Patients was developed to ensure the standard development, implementation, and spread of Telepharmacy in all its scopes. This guide is intended to help Hospital Pharmacy professionals benefit from Telepharmacy as a complementary tool to face-to-face pharmaceutical care.
Desarrollar una guía práctica sobre atención farmacéutica mediante Telefarmacia para profesionales y pacientes, en cada uno de sus ámbitos de aplicación. Definir en qué consiste, las herramientas utilizadas, los potenciales beneficios y las claves para facilitar su comprensión.
MétodoEntre diciembre de 2020 y enero de 2021, la Junta directiva de la Sociedad Española de Farmacia Hospitalaria, junto con coordinadores del proyecto “Mapa Estratégico para la Atención al Paciente Externo”, diseñaron una estrategia para favorecer el desarrollo y expansión de la Telefarmacia en España. Esta estrategia incluyó cuatro líneas de actuación. Para el desarrollo de la primera, en marzo de 2021 se llevó a cabo una convocatoria dirigida a los socios de la Sociedad Española de Farmacia Hospitalaria con objeto de desarrollar siete documentos de apoyo metodológico destinados a cubrir las necesidades para la implantación de la Telefarmacia, entre las cuales se consideraron como claves el desarrollo de una guía específica para profesionales y otra para pacientes. Las guías se desarrollaron en cuatro fases entre mayo y octubre de 2021: revisión de literatura, entrevistas de consenso, desarrollo de talleres de trabajo online y debate y, por último, elaboración y validación de los documentos finales. Una vez elaborado el borrador definitivo se llevó a cabo una valoración pública de sugerencias y alegaciones durante un mes, así como una presentación al comité de pacientes de la Sociedad Española de Farmacia Hospitalaria.
ResultadosLa guía para profesionales se ha orientado para dar las pautas para el desarrollo e implementación de programas de Telefarmacia en cada uno de sus ámbitos de aplicación. Está estructurada de forma que resalte los objetivos concretos, los beneficios asistenciales, las herramientas necesarias, así como las claves para implantarla. La guía para pacientes se ha desarrollado como herramienta complementaria a la atención farmacéutica presencial desde la visión del paciente, destacando las herramientas más comúnmente utilizadas, los potenciales beneficios y las claves para facilitar la comprensión sobre la finalidad y uso de estas intervenciones.
ConclusionesSe ha desarrollado una guía práctica de apoyo, tanto a profesionales como a pacientes, para estandarizar el desarrollo, implantación y expansión de la Telefarmacia en todos sus ámbitos de actuación. La guía pretende ayudar al colectivo de farmacia hospitalaria a alcanzar los potenciales beneficios de una herramienta que se presenta como complementaria a la atención farmacéutica presencial.
In recent years, the social and demographic changes, along with improvements in public health and continued therapeutic advances, have caused a dramatic increase in the volume of chronic patients attended at Hospital Pharmacy Services (HP)1. Meeting the population's needs as effectively as possible is a challenge for national health systems2.
In Spain, to standardize the evolution of outpatient hospital pharmacy care, the Spanish Society of Hospital Pharmacy (SEFH) launched the MAPEX project (Outpatient care strategy) in 2014 by adopting an anticipatory and updated perspective of hospital pharmacy care3. Based on this new approach, Morillo-Verdugo et al.4 developed a new definition of pharmaceutical care (PC) based on the three primary needs of patients: individualized dynamic care; target-oriented pharmacotherapy; and continued follow-up based on the use of new technologies.
The use of Telemedicine in pharmaceutical care is not a novelty5. This service, called Telepharmacy, has been developed and tested by numerous authors who have pioneered Telepharmacy in their countries6,7. Different international scientific societies have defined the concept of Telepharmacy. In Spain, the SEFH defined Telepharmacy as “remote pharmacy practice based on new technologies” and established four scopes of application: drug therapy monitoring; patient education and information; communication with a multidisciplinary team; and remote dispensing and informed delivery of medication8. The latter is the most widely known service, as the SARS-CoV2 pandemic generated multiple experiences and studies. The ENOPEX study in 9,442 patients revealed that 96.7% of patients reported being “satisfied” or “very satisfied” with Telepharmacy and considered it a complementary activity to standard follow-up by the Hospital Pharmacy9.
Despite the growing demand for Telepharmacy services, a national or international document for professionals and patients has not yet been published. A guide was necessary to foster the development of Telepharmacy and describe its advantages as a complementary service to face-to-face pharmaceutical care. A guide for the implementation of Telepharmacy will assist pharmacists in providing remote pharmaceutical care. In addition, the guide for patients will help patients make real-time decisions about their drug therapies with the counseling of their professionals of reference.
This study aims to develop a practical structured guide on Telepharmacy for professionals and another for patients. These guides will define Telepharmacy and describe the most common technologies, potential benefits, and the keys to helping users understand the purpose and use of Telepharmacy services.
MethodsBetween December 2020 and January 2021, the Board of Director of the SEFH, in collaboration with the coordinators of the MAPEX project and the Telepharmacy Strategy, developed a plan to favor the development and spread Telepharmacy. This plan included four courses of action: development of methodological guidelines, healthcare support, innovation and research, and technological support.
An open, public call was issued among SEFH members to recruit 24 candidates to develop the first course of action. Candidate hospital pharmacy specialists were required to have previous experience in the development and use of Telepharmacy and to have taken part in some of the initiatives developed within the framework of the MAPEX project. A geographically representative sample of professionals was recruited to ensure that the particularities of the different autonomous communities were considered during the drafting of the documents.
This first course of action resulted in the development of seven methodological guidelines aimed at meeting the methodological needs for the implementation of Telepharmacy in Spain: “Patient prioritization model”10; “Guide for pharmaceutical teleconsultation”11; “Effective, Safe Telepharmaceutical Care”12; and “Health Indicators”13; “Validation of Technological Tools”14 and two reference guides for patients and professionals.
The “Guide of Telepharmacy for professionals”15 was established as the core document, and the other documents would be based on this guide to ensure homogeneity and coherence. The “Guide of Telepharmacy for Patients”16 is considered an adaptation of the core guide for professionals.
This Guide was developed between May-October 2021 in four stages: literature review; consensus interviews using the nominal group technique (with direct communications among experts and face-to-face discussion); development of online workshops to discuss the essential aspects of the documents drafted; and drafting and validation of final documents.
Literature reviewA literature review was conducted to identify guidelines and recommendations for Telepharmacy programs. This review included recommendations from international and national pharmacy societies. This review aimed to identify successful experiences and help detect best practices in Telepharmacy.
Consensus interviewsAfter an analysis of the literature, a battery of interviews was conducted with the Working group both, individually and in groups, to identify impro vement points in Telepharmacy (safety, effectiveness, humanization) and key aspects for the validation of technologies (accessibility, usefulness, privacy, and confidentiality).
WorkshopsA total of four online workshops were held. The conclusions obtained from the literature review and interviews were presented, discussed, and validated in the first workshop. In the other workshops, recommendations were accepted, and priorities were established based on the impact and feasibility of each recommendation. The purpose was to assist professionals and patients in the use and implementation of Telepharmacy.
Drafting and validation of final documentsWhen the final draft was completed, a public evaluation of suggestions and observations was performed between December 2021 and January 2022 using the website of the MAPEX project. The final document was also presented to the Patient Committee of the SEFH.
ResultsGuide of Telepharmacy for Healthcare ProfessionalsThe Guide of Telepharmacy for Professionals provides guidelines for the development and implementation of Telepharmacy programs in their different scopes of application. These guidelines focus on specific goals, healthcare benefits, tools required, and keys to the implementation of Telepharmacy. This Guide is the core document on which the other documents are based.
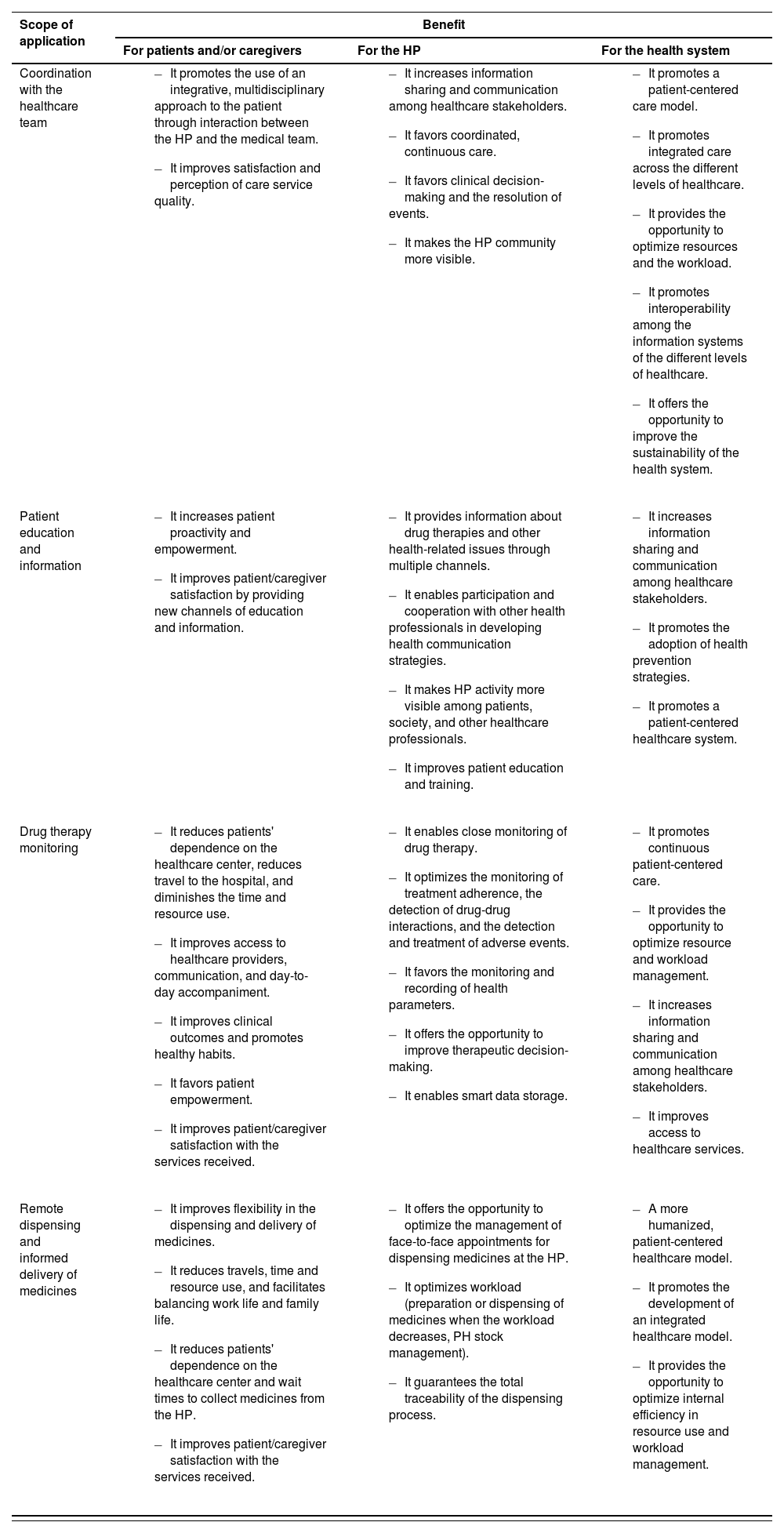
Below are described the main advantages of Telepharmacy concerning the four areas of application from the perspective of the patient, Hospital Pharmacy, and the health system (Table 1). For further information on the most relevant aspects of the document, visit https://www.sefh.es/mapex/cmo-oportunidad.php.
Below are described the main benefits of Telepharmacy concerning the four scopes of application from the perspective of the patient, Hospital Pharmacy, and the health system
| Scope of application | Benefit | ||
|---|---|---|---|
| For patients and/or caregivers | For the HP | For the health system | |
| Coordination with the healthcare team |
|
|
|
| Patient education and information |
|
|
|
| Drug therapy monitoring |
|
|
|
| Remote dispensing and informed delivery of medicines |
|
|
|
HP: hospital pharmacist; HPS: hospital pharmacy service.
Telepharmacy applied to coordination with the care team involves using information and communication technologies (ICTs) to enable interaction among healthcare professionals. The main purpose is to improve continued healthcare and promote an integral multidisciplinary approach to the patient. These communication channels can be established among hospital pharmacy professionals and the healthcare team (care team, nursing staff, or others) to improve drug therapies’ selection and follow-up and adopt a multidisciplinary approach to cases. This scope of application may also provide the opportunity to disseminate information and education among professionals, promote networking, or raise awareness about the role of hospital pharmacy professionals.
There is a wide range of technologies that enable coordination, synchronous/asynchronous communication and information-sharing among healthcare professionals. Synchronous communication via phone or video call favors real-time communication among professionals. In contrast, asynchronous communication is performed through electronic mail, instant messaging, Web 2.0 (i.e., websites, blogs, professional forums, and social networks, to name a few); cross-consultation tools through the electronic medical record (EMR), or through platforms combining instant messaging and the EMR. These tools may favor rapid information dissemination and sharing among professionals, foster networking, and enhance the visibility and consideration of pharmacy hospital professionals as healthcare professionals. Other cross-consultation tools, such as EMRs, are necessary for Telepharmacy, since they make it possible to record clinical information in an interoperable and integrative way with hospital information systems.
To coordinate healthcare teams through Telepharmacy, we suggest the following scheme: analysis and goals; selection of the tools and resources required; development of the service; education and training; results and identification of improvement points. For further information about Telepharmacy technologies, please consult the document “Validation of Telepharmacy technologies”14.
Patient education and informationTelepharmacy applied to patient information and education involves using ICTs to establish communication channels that enable patient education and the transmission of rigorous, truthful, updated information. It is also an alternative communication channel for patient-clinician interaction.
The use of Telepharmacy in this scope contributes to collaborative learning (i.e. education programs), provides information about the therapy (dosing, adverse events, drug-drug interactions, adherence); help share experiences; promotes the empowerment of patients and/or caregivers; and improves autonomy and awareness about the relevance of the therapy. In addition, it improves professional-patient communication and awareness of the therapeutic needs and therapies of the patient.
The hospital pharmacist is responsible for sharing with their patients the information and educational resources available concerning their drug therapies, whether designed by the Hospital Pharmacy itself or developed by other sources of reference. Thus, the hospital pharmacist must get involved in the whole process, i.e., management, generation, dissemination, and sharing of information.
There are numerous technologies available that enable information sharing and patient education. These technologies include blogs, social networks, wikis, interconnected multimedia services, videos, discussion forums, online infographics, training platforms or interactive online games, to name a few. The accessibility of these tools makes it possible that hospital pharmacies provide information and educational resources to their patients and caregivers via online or face-to-face channels. For further information about Telepharmacy technologies, please consult the document “Validation of Telepharmacy technologies” (14).
To use a Telepharmacy program for patient education and training, we suggest the following scheme: analysis and goals; selection of the tools and resources required; development of the service; education and training; results and identification of improvement points.
Drug therapy monitoringThe implementation of Telepharmacy for drug therapy monitoring involves using ICTs to attain the individual pharmacotherapeutic targets of each patient through the detection of drug-drug interactions, adverse events, management of therapeutic adherence, review of medication, evaluation of clinical outcomes, and measurement of PROs and PREMs.
Remote drug therapy monitoring can be performed via teleconsultation and/or telemonitoring. Teleconsultation enables scheduled two-way communication with the patient to resolve doubts and provide counseling.
Additionally, telemonitoring facilitates remote follow-up of pharmacological parameters (i.e., monitoring treatment adherence and other clinical parameters).
There is a broad range of ICT-based technologies that enable drug therapy monitoring through synchronous and/or asynchronous teleconsultation and telemonitoring. Synchronous technologies such as the phone or video call platforms allow two-way real-time communication between the patient and the professional to resolve doubts and provide guidance through tele-consultation. Although video call platforms are gaining ground, the most widely used tool is the telephone since they enable video sharing. It is necessary that patients and healthcare professionals have access to secure video call platforms and a stable Internet connection that supports video calls. Moreover, patients and professionals must have adequate technical skills.
Asynchronous tools include electronic mail, SMS, instant messaging, voice notes, videos or consultation via website. These technologies enable deferred communication and do not require that the patient and the professional are connected simultaneously. These tools are generally used to arrange appointments, send reminders, and resolve doubts. This technology group also encompasses mobile health services, including apps and wearables that monitor and record pharmacotherapeutic information and/or health parameters. The use of these technologies has increased in recent years due to advances in healthcare services, patient proactivity, and a reduction in the technology gap. Real-time data transfer with healthcare professionals is also possible through apps or wearables. The choice of teleconsultation/telemonitoring tools depends on the capacities and resources available in each pharmacy hospital and the technology skills of the patients and professionals involved.
For further information about the implementation of Telepharmacy in this scope, please, consult the documents: “Patient prioritization model”; “Guide for pharmaceutical teleconsultation”; “Effective, safe pharmaceutical care”; and “Health indicators”, available at: https://www.sefh.es/mapex/cmo-oportunidad.php.
Remote dispensing and informed deliveryThis application of Telepharmacy involves shipping medicines to the point of delivery close to the patient's place of residence, which contributes to flexibility in the informed delivery of medication.
A variety of delivery pathways are available: patient's home, healthcare center, nursing home, and community pharmacy. This variety requires flexibility in logistics to adapt to the patient's needs, which may vary across patients and change over time.
Whichever pathway and point of delivery are chosen, remote delivery will involve informed delivery and a follow-up teleconsultation, along with face-to-face consultations, when necessary, to verify pharmacotherapeutic targets. Transportation of medication, whether carried out by in-house or outsourced personnel (i.e., logistics companies, patient associations) will be performed in compliance with current laws and regulations to guarantee adequate storage, traceability, personal data protection, and proper medicine handling.
Remote dispensing and informed medication delivery can be provided via synchronous technologies such as telephone or video calls. These technologies enable two-way real-time communication between the patient and the professional, which is key to guaranteeing informed home delivery of medication. Asynchronous technologies (i.e., e-mail, SMS, web apps or mobile apps) are generally used to schedule shipping, send reminders, resolve doubts in remote dispensing, confirm medicine receipt, grant shipping authorization, and guarantee traceability, among other uses.
For further information about the implementation of Telepharmacy in remote dispensing and informed delivery of medication, please consult: “Patient prioritization model”; “Guide for pharmaceutical teleconsultation”11; “Effective, safe telepharmaceutical care”); and “Health indicators”, available at: https://www.sefh.es/mapex/cmo-oportunidad.php
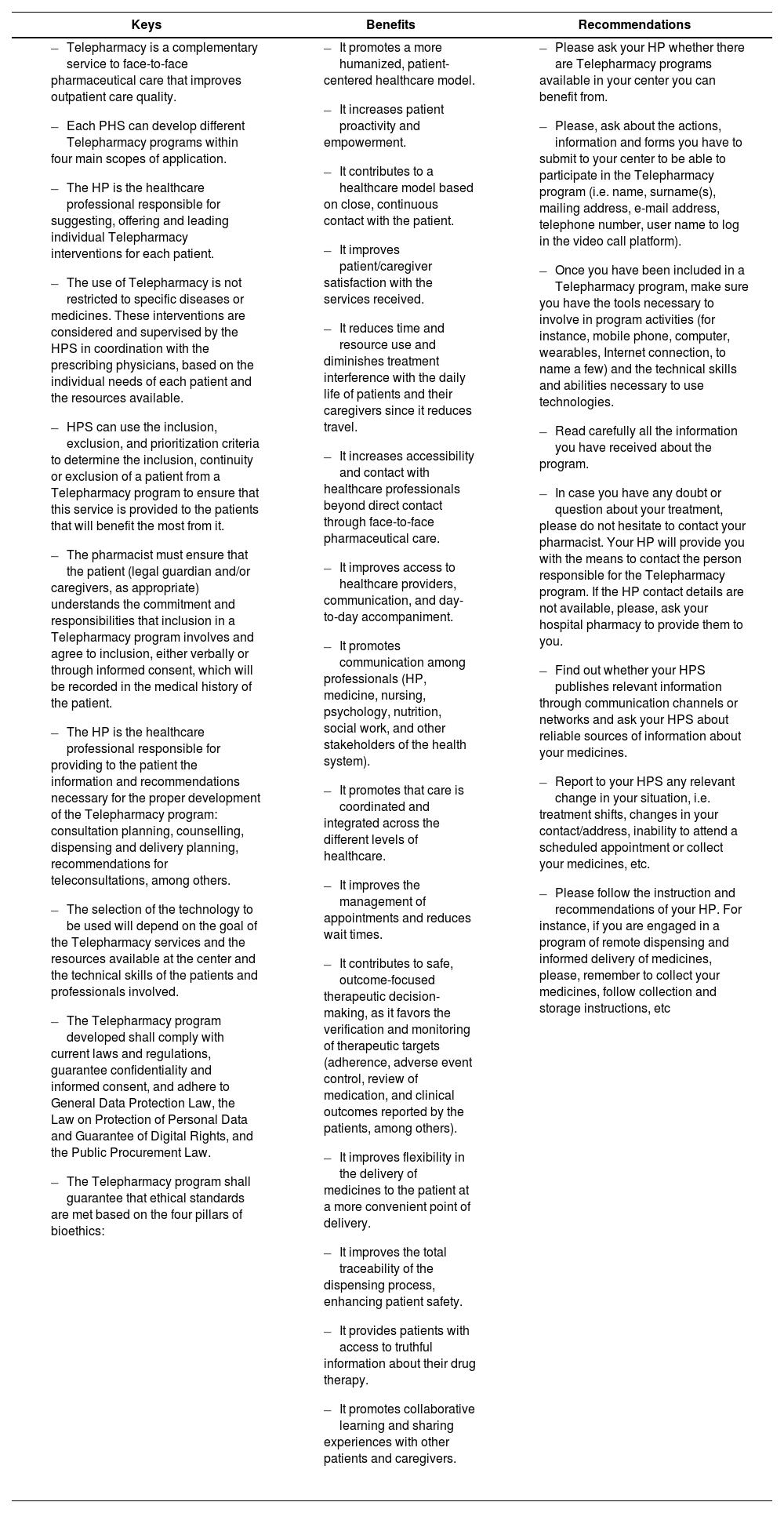
Guide of Telepharmacy for PatientsThis guide is addressed to patients and/or caregivers using Telepharmacy as a complementary tool to face-to-face pharmaceutical care.
To such purpose, the scopes of application of Telepharmacy are defined from patient's perspective. Emphasis is placed on the most common technologies, the advantages of Telepharmacy, and the keys to facilitating patients’ understanding of the purpose and use of these interventions (Table 2). The most relevant aspects of this Guide are described at: https:// www.sefh.es/mapex/cmo-oportunidad.php
Keys, benefits, and recommendations for Telepharmacy service recipients
| Keys | Benefits | Recommendations |
|---|---|---|
|
|
|
HP: hospital pharmacist; HPS: hospital pharmacy service.
To the best of our knowledge, these are the first practical guides for healthcare professionals and patients providing guidelines for developing and incorporating Telepharmacy in its different scopes of application.
Mixed pharmaceutical care combining face-to-face and remote care is a reality17. However, developing a Telepharmacy system with adequate characteristics that meet the needs of healthcare professionals and patients is challenging. In this sense, each Hospital Pharmacy must define and incorporate the Telepharmacy program that best adapts to the HP, patients, and healthcare center18. Hospital Pharmacies planning to incorporate a Telepharmacy program must consider relevant aspects such as the program's purpose, the technologies that will be employed, the resources available, and the technical skills of healthcare professionals and patients.
These guides will assist HPs in implementing and initiating the program and promoting the use of Telepharmacy in its four scopes of application, namely: patient training and education; drug therapy monitoring; healthcare team coordination; and remote dispensing and informed delivery of medication, which require further development. Additionally, these documents will ensure that Telepharmacy programs are developed and implemented homogeneously to meet standard goals, regardless of variability in each HP's human and material resources. These programs will benefit both patients –the main beneficiaries– and health professionals.
According to Tortajada-Goitia et al.19, remote consultations were made available in 87.6% of hospitals during the pandemic. In contrast, a study conducted by Koster et al.20 in community pharmacies in the Netherlands revealed a lower percentage, 44.2%, which was explained by the low level of agreement between physicians and pharmacists added to confidentiality issues related to the information provided to patients.
In line with other initiatives concerning coordination of healthcare professionals, this Guide highlights that Telepharmacy offers an opportunity to improve communication among professionals at different levels of healthcare, promote the dissemination of information among professionals, foster joint activities, and position HP as a reference in the healthcare community. Making the role of HP visible will positively impact the level of satisfaction and experience of patients21.
A range of studies confirms that one of the most frequent demands to healthcare services during the COVID-19 pandemic in different countries and regions was the remote provision of health information through ICTs, even during the hardest times of restrictions, limitations to mobility, and information volatility22. These studies highlight the significant role that Telepharmacy may play in patient training and information. Telepharmacy in this scope will help confront current challenges to health systems and provide rapid truthful information to counter generalized misinformation. The Guide identifies three key points related to the role of HPs: information management leadership, content generation, and information dissemination. Telepharmacy also enables collaborative learning, raises awareness of the use of medicines among patients, and promotes patient autonomy. In addition, it improves clinician-patient communication and awareness on the therapeutic needs and therapies of the patient.
Although Telepharmacy is not a novelty, studies conducted before and during the pandemic have yielded promising results, as it reduces medication errors and improves the quality of pharmaceutical care23,24. Although some authors are certain that Telepharmacy has come to stay, it should be clarified that it complements face-to-face pharmaceutical care. The best example is that Telepharmacy enables remote drug therapy monitoring, which allows teleconsultation, telemonitoring and other activities that will help provide more individualized care, highlighted in the two Guides.
Some experiences in Spain reveal that ICT-based telemonitoring by hospital pharmacists was effective in improving clinical outcomes. In this line, Gomis et al. reported that Telepharmacy improved treatment adherence and patient understanding and use of medicines, reduced therapeutic complexity and adverse events, and enhanced the satisfaction and experience of complex cases such as heart transplant recipients. More than half of these patients could be monitored remotely, and face-to-face appointments were reserved for selected cases, which reduced wait times at the HP25. Collado-Borrell et al. demonstrated that drug therapy monitoring in cancer patients through a mobile app improved treatment adherence and health-related quality of life and reduced resource consumption26.
Telepharmacy makes it possible to anticipate patient needs and provide effective individualized care, which benefits our patients. The benefits of Telepharmacy have been widely demonstrated during the COVID-19 pandemic in the scope of remote dispensing and informed delivery of medication.
Offering different delivery points requires flexibility in logistics to adapt to the patient's needs, which may vary across patients and change over time. Although the different options have their advantages and disadvantages, it is important to note that the delivery of medication is as important as the provision of information and rapid action of multidisciplinary teams. Although Telepharmacy has been successfully implemented during the COVID-19 pandemic27, some authors highlight that it is necessary to design, develop and integrate Telepharmacy apps that include drug therapy monitoring and remote dispensing and delivery of medication. This would guarantee their traceability and control, reduce demand on the health system, and provide patients with timely access to pharmaceutical care, even when they are far from their health center.
Other key elements have been identified to contribute to attaining the goals described in this Guide. Firstly, to accelerate the development and implementation of Telepharmacy, it is necessary to identify the challenges, barriers, and enablers found in previous initiatives in a more advanced stage. Establishing an observatory of innovative practices is crucial for the HP community to take advantage of the lessons learned and previous experiences of other HPs. In addition, creating digital training centers will help patients and professionals get the most out of Telepharmacy tools. Training courses will enhance the digital skills, resources and abilities required to optimize the use of Telepharmacy technologies.
Finally, innovative, robust, multicentric, multidisciplinary, and international studies are needed to demonstrate the full range of advantages that Telepharmacy offers. Attaining this ambitious goal will require the leadership and support of the different scientific societies and healthcare entities.
This practical guide for professionals and patients was developed to ensure the standard development, implementation, and spread of Telepharmacy in all its scopes of application. This Guide is intended to help Hospital Pharmacy professionals benefit from Telepharmacy as a complementary tool to face-to-face pharmaceutical care.
FundingNo funding.
AcknowledgementsWe thank all members of the group responsible for the development of the “Methodological support documents for the development of Telepharmacy” of the MAPEX-SEFH project.
To Ascendo Consulting for its consulting and advisory services in the development of this document.
Conflict of interestsNo conflicts of interest.