The purpose of this article is to report the experience of the Department of Hospital Pharmacy of a mid-size hospital during the peak of the COVID-19 pandemic. The human and material resources available in a mid-size hospital were more limited than in larger hospitals of the region. In this article, we describe how this Department of Hospital Pharmacy was reorganized to meet the increase in activity, the strategies developed and the lessons learned for future pandemics.
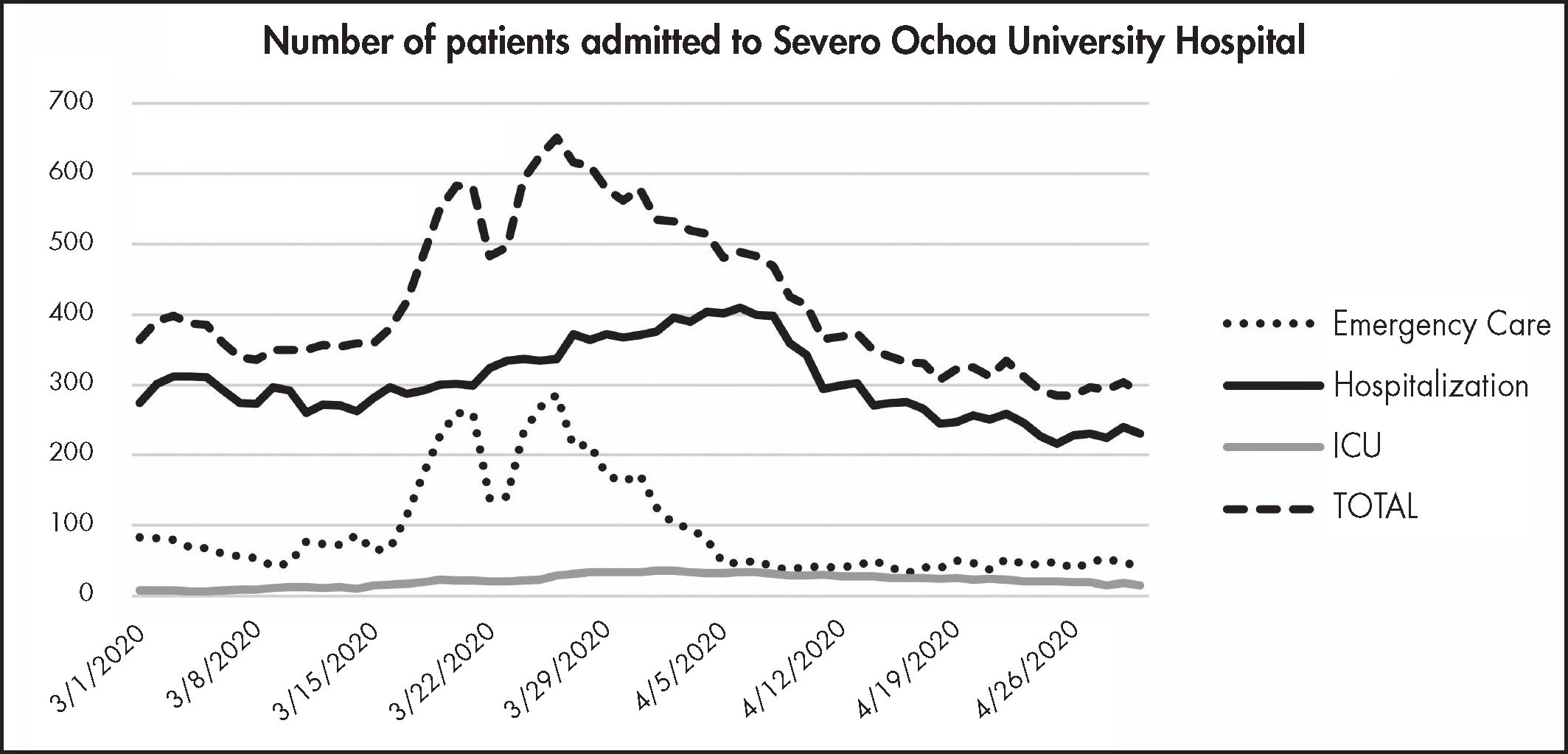
The COVID-19 pandemic had a higher impact in Leganes, a city in the south of Madrid, with a population of 190,000. In the face of the dramatic increase in the proportion of patients attending our hospital between March and April 2020, the Severo Ochoa University Hospital increased the number of beds by 24.5% and fitted out new premises inside and outside the hospital (sports centers). The mean number of patients seen in our Emergency Department every day passed from 70-80 to a peak of 286 patients, with 652 hospitalized patients.
The situation of emergency created by this infectious disease, with management protocols changing constantly, had a dramatic impact on the activity of hospital pharmacies. Thus, the pandemic has affected areas of economic management, magistral preparation, dispensing of medication to inpatients, ambulatory patients, patients monitored at home, institutionalized patients, and patients from private hospitals and field hospitals. Other areas affected include training, clinical trials, pharmacovigilance, and counseling boards.
Two strategies were adopted to overcome these problems: a strategy centered on human resources (staff reinforcement, reallocation of responsibilities), and a strategy centered on processes (some processes were reinforced to meet the increase in activity, whereas other were temporarily suspended or reduced to the minimum).
ConclusionsThe Department of Hospital Pharmacy plays a key role in hospitals and has been significantly reinforced to meet the dramatic impact of the pandemic on this department. This Department has been able to reorganize its processes and take over new responsibilities such as telepharmacy and home dispensing. Hospital pharmacies play a crucial role in pharmacotherapeutic decisions in hospitals. As in other Departments, training is the area more significantly affected by the pandemic.
El objetivo de este artículo es describir la experiencia del servicio de farmacia de un hospital mediano, en el período álgido de la pandemia de COVID-19, con recursos humanos y materiales más limitados que otros hospitales de su entorno de mayor tamaño. Se analiza cómo afrontó su reorganización, debido al incremento de su actividad, así como las estrategias desarrolladas y las lecciones aprendidas para afrontar el futuro.
La pandemia por COVID-19 tuvo especial repercusión en el municipio de Leganés, una ciudad de 190.000 habitantes al sur de Madrid. Ante el incremento de la afluencia de pacientes entre los meses de marzo y abril de 2020, el Hospital Universitario Severo Ochoa llegó a asumir un 24,5% más de camas, incluyendo nuevas ubicaciones tanto dentro como fuera del hospital (pabellón deportivo). Siendo la media de frecuentación del Servicio de Urgencias de 70-80 pacientes, se llegó a alcanzar un pico de 286 pacientes y 652 pacientes ingresados.
Esta situación de emergencia y el abordaje de una patología infecciosa, con protocolos de tratamiento en continua revisión, impactó en todas las áreas y actividades del servicio de farmacia: adquisiciones, gestión económica, elaboración de medicamentos y dispensación a pacientes hospitalizados, pacientes externos y ambulantes, domiciliaria, a centros geriátricos, hospitales de gestión privada y hospitales de campaña. Se vieron afectadas áreas como la formación, los ensayos clínicos, la farma-covigilancia y las comisiones hospitalarias.
Para superar los problemas, se aplicaron dos estrategias: una centrada en los recursos humanos (reforzamiento de áreas, reasignación de responsabilidades) y otra focalizada en los procesos (procesos que se reforzaron por un aumento de la actividad, procesos que se suspendieron temporalmente por la pandemia y procesos que se redujeron al mínimo).
ConclusionesEl servicio de farmacia es una pieza clave en el hospital cuyas funciones principales son las primeras perjudicadas, pero a la vez las más reforzadas durante la pandemia. Ha tenido la capacidad de reorganizar sus procesos para asimilar nuevas actividades, como la telefarmacia y la dispensación domiciliaria. Juega un papel importante en las decisiones farmacoterapéuticas del hospital. Al igual que otros servicios clínicos, la formación ha sido el área más perjudicada.
The COVID-19 pandemic had a higher impact in Leganes, a city in the south of Madrid, with a population of 190,000. During the peak of the pandemic from 13th to 30th of March, 2020, 3,562 patients with suspicion of COVID-19 (2,171 confirmed) were admitted to the Severo Ochoa University Hospital (HUSO) in Leganes. As of May 18th, the incidence of COVID-19 in Leganés was estimated to be 1,570 cases per 100,000.
In the light of the avalanche of patients, the hospital extended the number of beds from 392 to 488 (24.5% more). Of the 96 beds, 30 were installed in a nearby sports hall, with the remainder having been installed in the rehabilitation gym, waiting rooms, and the intensive care unit (ICU), which capacity was extended from 12 to 35 beds. Only 94 beds (20%) were left for non-COVID patients. The mean length of stay was 9 days in hospitalization wards, and 23 days in the ICU. A total of 388 patients died between March and April.
Figure 1 shows the evolution in the number of hospitalized patients. Admissions peaked in the last week of March, with 652 patients hospitalized. Of them, 286 were admitted to the Emergency Department, which accounts for a 250% increase in the proportion of Emergency Department patients, which is generally 70-80. The increasing number of patients forced the hospital to refer 525 patients to 11 centers, 10 hospitals and the IFEMA field hospital, which received a total of 348 patients (two thirds of the patients transferred).
The purpose of this article is to share the experience of the Hospital Pharmacy Department of a mid-size hospital during the peak of the COVID-19 pandemic. The human and material resources available in a mid-size hospital are more limited than in larger hospitals of the region. In this article, we describe how this Hospital Pharmacy Department reorganized to meet the increase in activity, the strategies developed and the lessons learned for future pandemics.
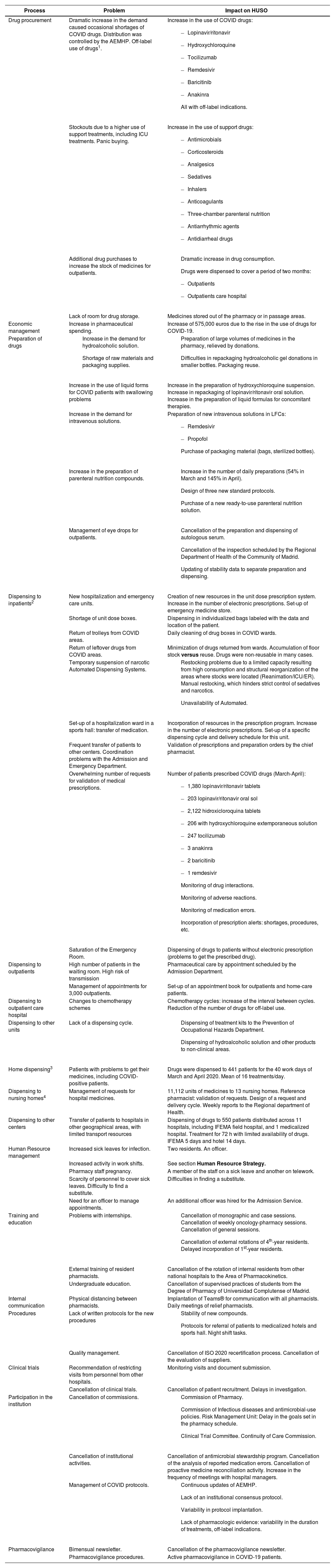
Challenges and impactAs expected, the pandemic affected most of the areas of our Hospital Pharmacy (HP) Department, which is composed of 8 pharmacists and 8 residents, 4 nurses and 15 pharmacy technicians. Table 1 summarizes the challenges faced by the HP and the impact of the pandemic on the different pharmacy processes.
Impact of the COVID pandemic on the acitivty of the Pharmacy Hospital of Severo Ochoa University Hospital
| Process | Problem | Impact on HUSO |
|---|---|---|
| Drug procurement | Dramatic increase in the demand caused occasional shortages of COVID drugs. Distribution was controlled by the AEMHP. Off-label use of drugs1. | Increase in the use of COVID drugs:
|
| Stockouts due to a higher use of support treatments, including ICU treatments. Panic buying. | Increase in the use of support drugs:
| |
| Additional drug purchases to increase the stock of medicines for outpatients. |
| |
| Lack of room for drug storage. | Medicines stored out of the pharmacy or in passage areas. | |
| Economic management | Increase in pharmaceutical spending. | Increase of 575,000 euros due to the rise in the use of drugs for COVID-19. |
| Preparation of drugs |
|
|
| Increase in the use of liquid forms for COVID patients with swallowing problems | Increase in the preparation of hydroxychloroquine suspension. Increase in repackaging of lopinavir/ritonavir oral solution. Increase in the preparation of liquid formulas for concomitant therapies. | |
| Increase in the demand for intravenous solutions. | Preparation of new intravenous solutions in LFCs:
| |
| Increase in the preparation of parenteral nutrition compounds. |
| |
| Management of eye drops for outpatients. |
| |
| Dispensing to inpatients2 | New hospitalization and emergency care units. | Creation of new resources in the unit dose prescription system. Increase in the number of electronic prescriptions. Set-up of emergency medicine store. |
| Shortage of unit dose boxes. | Dispensing in individualized bags labeled with the data and location of the patient. | |
| Return of trolleys from COVID areas. | Daily cleaning of drug boxes in COVID wards. | |
| Return of leftover drugs from COVID areas. | Minimization of drugs returned from wards. Accumulation of floor stock versus reuse. Drugs were non-reusable in many cases. | |
| Temporary suspension of narcotic Automated Dispensing Systems. |
| |
| Set-up of a hospitalization ward in a sports hall: transfer of medication. | Incorporation of resources in the prescription program. Increase in the number of electronic prescriptions. Set-up of a specific dispensing cycle and delivery schedule for this unit. | |
| Frequent transfer of patients to other centers. Coordination problems with the Admission and Emergency Department. | Validation of prescriptions and preparation orders by the chief pharmacist. | |
| Overwhelming number of requests for validation of medical prescriptions. | Number of patients prescribed COVID drugs (March-April):
| |
| Saturation of the Emergency Room. | Dispensing of drugs to patients without electronic prescription (problems to get the prescribed drug). | |
| Dispensing to outpatients | High number of patients in the waiting room. High risk of transmission | Pharmaceutical care by appointment scheduled by the Admission Department. |
| Management of appointments for 3,000 outpatients. | Set-up of an appointment book for outpatients and home-care patients. | |
| Dispensing to outpatient care hospital | Changes to chemotherapy schemes | Chemotherapy cycles: increase of the interval between cycles. Reduction of the number of drugs for off-label use. |
| Dispensing to other units | Lack of a dispensing cycle. |
|
| Home dispensing3 | Patients with problems to get their medicines, including COVID-positive patients. | Drugs were dispensed to 441 patients for the 40 work days of March and April 2020. Mean of 16 treatments/day. |
| Dispensing to nursing homes4 | Management of requests for hospital medicines. | 11,112 units of medicines to 13 nursing homes. Reference pharmacist: validation of requests. Design of a request and delivery cycle. Weekly reports to the Regional department of Health. |
| Dispensing to other centers | Transfer of patients to hospitals in other geographical areas, with limited transport resources | Dispensing of drugs to 550 patients distributed across 11 hospitals, including IFEMA field hospital, and 1 medicalized hospital. Treatment for 72 h with limited availability of drugs. IFEMA 5 days and hotel 14 days. |
| Human Resource management | Increased sick leaves for infection. | Two residents. An officer. |
| Increased activity in work shifts. | See section Human Resource Strategy. | |
| Pharmacy staff pregnancy. | A member of the staff on a sick leave and another on telework. | |
| Scarcity of personnel to cover sick leaves. Difficulty to find a substitute. | Difficulties in finding a substitute. | |
| Need for an officer to manage appointments. | An additional officer was hired for the Admission Service. | |
| Training and education | Problems with internships. |
|
| External training of resident pharmacists. | Cancellation of the rotation of internal residents from other national hospitals to the Area of Pharmacokinetics. | |
| Undergraduate education. | Cancellation of supervised practices of students from the Degree of Pharmacy of Universidad Complutense of Madrid. | |
| Internal communication | Physical distancing between pharmacists. | Implantation of Teams® for communication with all pharmacists. Daily meetings of relief pharmacists. |
| Procedures | Lack of written protocols for the new procedures |
|
| Quality management. | Cancellation of ISO 2020 recertification process. Cancellation of the evaluation of suppliers. | |
| Clinical trials | Recommendation of restricting visits from personnel from other hospitals. | Monitoring visits and document submission. |
| Cancellation of clinical trials. | Cancellation of patient recruitment. Delays in investigation. | |
| Participation in the institution | Cancellation of commissions. |
|
| Cancellation of institutional activities. | Cancellation of antimicrobial stewardship program. Cancellation of the analysis of reported medication errors. Cancellation of proactive medicine reconciliation activity. Increase in the frequency of meetings with hospital managers. | |
| Management of COVID protocols. |
| |
| Pharmacovigilance | Bimensual newsletter. | Cancellation of the pharmacovigilance newsletter. |
| Pharmacovigilance procedures. | Active pharmacovigilance in COVID-19 patients. |
AEMHP: Spanish Agency of Medicines and Medical Devices; COVID: Coronavirus disease; ICU: Intensive Care Unit; ISO: International Standards Órganization; LFC: laminar flow cabinet.
Two strategies were adopted to overcome the problems detailed in the table below.
Human resource strategyThe following actions were taken:
- –
Outpatient care staff passed from two to four pharmacists (two full-time and two part-time).
- –
A person was assigned to dispense hospital medicines to nursing homes (part-time).
- –
A person was assigned to manage medication of patients transferred to other centers (part-time).
- –
A person was assigned to manage the procurement of drugs controlled by the Spanish Agency of Medicines and Medical Devices (AEMHP) (part-time).
- –
The oncology pharmacist was assigned the management of COVID patients (part-time).
- –
The pharmacy technical staff was reinforced with personnel from other departments.
- –
The night shift was reinforced with a on-call pharmacist and a pharmacy technician. An adiccional pharmacist was available until 10 pm all days of the week.
- –
An officer was hired to explain the new appointment system and dispensing cycle to patients.
- –
A driver was hired for home drug delivery in the morning shift.
Processes were divided into three groups: processes that were reinforced for a rise in activity, processes that were temporarily suspended for the pandemic, and processes that were reduced to the minimum.
The following processes were prioritized:
- –
Drug procurement:
- •
COVID treatment.
- •
Support medication.
- •
- –
Stock management.
- •
Daily reports of drug stocks to the Regional Department of Health.
- •
- –
Validation of treatments.
- –
Preparation of medicines:
- •
Preparation of propofol, oral antivirals (syringe), etc.
- •
Disinfectant solutions.
- •
Parenteral nutritions.
- •
- –
Dispensing of drugs to hospitalized COVID patients:
- •
In our hospital and the sports hall.
- •
Transferred to other centers.
- •
- –
Dispensing of drugs to outpatients:
- •
Set-up of an appointment book in SELENE to prevent an unexpected inflow of patients.
- •
Direct mobile phone number for patients to receive calls.
- •
- –
Home dispensing:
- •
Set-up of a SELENE appointment book with the involvement of the prescriber.
- •
Patient selection criteria: disabling disease, advanced age or low socioeconomic status, impossibility to travel to the hospital and high-risk disease as defined in the protocol3.
- •
- –
Dispensing of drugs for hospital use to nursing homes in collaboration with the Service of Geriatrics in accordance with the regulations4.
- –
Dispensing of drugs to healthcare professionals at the Service of Occupational Risk Prevention:
- •
Preparation of a treatment kit.
- •
- –
Internal communication:
- •
Daily meetings, Teams® app, telework.
- •
- –
Reinforcement of the night shift at the hospital pharmacy.
- •
Transfer of activity to the night shift.
- •
- –
External communication:
- •
Active communication with other hospital pharmacies of Madrid by e-mail and chat.
- •
Communication with the Regional Department of Health.
- •
Sharing of information with nursing homes and other hospitals.
- •
To take over new tasks, the HP suspended the following tasks and duties:
- –
Antimicrobial Stewardship Program.
- –
Preparation of autologous serum eye drops.
- –
Quality recertification.
- –
Training sessions for pharmacy residents.
- –
Rotation of residents to other units.
- –
Rotation of external residents to our Unit of Pharmacokinetics.
- –
Supervised internship program of the Universidad Complutense of Madrid.
- –
Visits from the pharmaceutical industry.
- –
Meetings of the Commissions of Pharmacy and Therapeutics, Infections and Antimicrobial Use Policy, Continuity of Care, Pain, Risk Management Unit, etc.
- –
Visits from clinical trial monitors.
- –
Pharmaceutical Inspection.
- –
Recruitment of patients for clinical trials.
Finally, other activities were limited to the minimum:
- –
Activity of the Unit of Clinical Pharmacokinetics.
- –
Medication error reports.
- –
Processing of drugs for off-label use.
- –
Evaluation of drug offers.
- –
Pharmacovigilance.
- –
Calculation and follow-up of indicators.
Learned lessons. Future applicability in pharmacy services
Some lessons that may be useful in the future have been learned from this experience, which include:
- •
Relevance of HP. Whatever the size of the hospital, hospital pharmacists play a major role in guaranteeing correct access to and use of medicines. The relevance of pharmacy professionals has been demonstrated during the public health emergency, where concerns but also professional talent and solidarity arose. Whereas other hospital services disappeared during the pandemic, HP were reinforced.
- •
Impact of the pandemic. Pharmacy services are confronted with numerous problems. These challenges can only be overcome through cooperation between HPs and Regional Health Departments. The healthcare and pharmaceutical care provided in nursing homes should be improved, which involves regulatory changes and reinforcing pharmacy resources.
- •
Big challenges mean great opportunities for emerging areas to be developed. Telemedicine and telepharmacy will be integrated in hospitals and will be an indispensable tool of pharmacy care. Home dispensing has come to stay, but will require regulatory changes.
- •
The pandemic is not over. We should prepare for a second or third wave. Normality will not be as in the past. Hospital activity will change, and hospital management will be focused on limiting patient visits to the hospital.
- •
A range of protocols will be established for the management of COVID patients, including pharmaceutical care, safety during contact with the patient, pharmacotherapeutic follow-up, drug dispensing to nursing homes, telepharmacy, home dispensing, etc. and the Spanish Society of Hospital Pharmacy will lead the way.