Bacterial infections of the central nervous system are relatively uncommon but highly lethal if not diagnosed and treated promptly. Specifically, cerebral abscesses often result from adjoining infectious foci or metastatic phenomena. Although the type of germ involved will depend on the nature of the primary focus, some microorganisms do occur more frequently than others. These include viridans group streptococci and/or anaerobic bacteria1. Many patients exhibit a torpid clinical course with neurologic or systemic complications and, in some cases, adverse reactions to treatment, which may result in increased morbidity and mortality in surviving patients, or even death.
As regards the occurrence of adverse reactions secondary to long-term antibiotic treatment, numerous mild events have been reported. Neurologic manifestations are uncommon and not necessarily related to the treatment. Such neurologic effects are more frequent in geriatric or multi-morbidity patients, who often present with pharmacokinetic alterations. Antimicrobial agents that have been associated with neurotoxicity include betalactams, quinolones, macrolides and sulfonamides1,2. Considering the potential occurrence of adverse events, administration of such agents should be discontinued in patients on long-term antibiotic treatment so as not to interfere with the resolution of the primary infection.
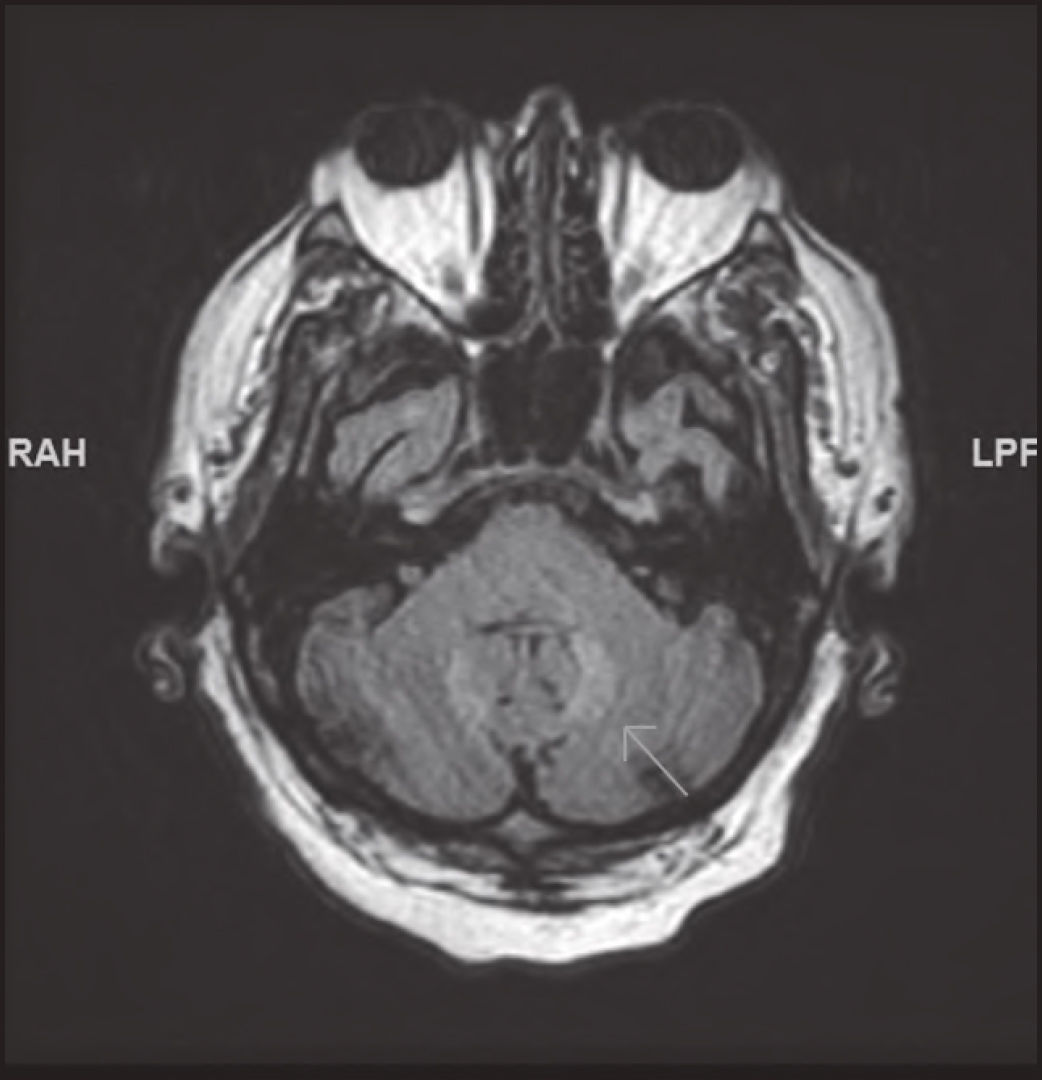
Case descriptionThe patient was a 69-year-old male with alcoholic cirrhosis and chronic obstructive pulmonary disease (COPD) who was admitted for a cerebral abscess with ventricular extension diagnosed against a background of longlasting fever and disorientation. After analyzing the case, the neurosurgery department ruled out surgery on account of the location of the infection. A lumbar puncture was performed and empirical antibiotic therapy was initiated with IV ceftriaxone (2 g) every 12 hours and IV metronidazole (10 mg/kg) every 8 hours. A cerebrospinal fluid culture tested positive for Streptococcus intermedius and Fusobacterium nucleatum, which resulted in a decision to maintain the antibiotic treatment. Up to the fifth week, the patient's clinical and radiological evolution was favorable. However, at that point he developed rapidly progressive dysarthria and ataxia. T2-FLAIR magnetic resonance (MR) images of the brain revealed not-previously-observed bilateral symmetrical signal intensity alterations in the cerebellar dentate nuclei (Figure 1). The initial abscess and the ventriculitis showed a satisfactory evolution. At the same time, the patient was receiving treatment with IV fluconazole for urinary candidiasis, induced by an indwelling bladder catheter.
Due to the suspicion that the patient could have developed cerebellar toxicity as a result of long-term administration of metronidazole (accumulated dose: 117 g), a decision was made to withdraw the drug (together with ceftriaxone). After conducting the relevant susceptibility tests, treatment with meropenem was initiated through extended infusion. The cerebellar syndrome resolved completely a week after discontinuation of metronidazole; cerebellar x-ray findings also went back to normal. The patient evolved favorably after 90 days’ administration of extended-perfusion meropenem, with complete resolution of the abscess and the ventriculitis as observed in follow-up MRIs. The case was reported to the Spanish pharmacovigilance system.
DiscussionMetronidazole is a commonly used antibiotic, whose activity is mainly directed against anaerobic germs1. It is a dose-dependent agent with bactericidal effect. Its most frequent adverse events are of a gastrointestinal nature, although the use of high doses over long periods of time has been associated with nervous system disorders1. This means that the metronidazole-induced cerebellar syndrome, which tends to manifest itself in the form of dysarthria or ataxia, is an uncommon yet clinically significant entity. Not surprisingly, it has received wide attention in the literature3.
The incidence of metronidazole-induced cerebellar syndrome is higher in males, especially in those over 40 years of age4, and cumulative dosedependent3. In our case, the accumulated metronidazole dose was 117 g, not dissimilar to the 126 g mean dose administered in 110 cases reported in a systematic review4. The physiopathologic profile of the condition is ill understood, but several hypotheses have been put forward that attribute the syndrome to the deleterious cellular effects resulting from the interference of metronidazole metabolites with the synthesis of neuronal RNA5.
The most common of all predisposing factors is cirrhosis of the liver5. In our case, the patient was also being treated with fluconazol, a metronidazole-metabolizing inhibitor of cytochrome P4506, which probably led to increased serum concentrations of metronidazole, facilitating the development of the condition. This could not be confirmed as no serum levels of metronidazole were detected.
Although the diagnosis of metronidazole-induced cerebellar syndrome requires a high level of suspicion, some specific x-ray findings have been described. The most common of such findings is bilateral, symmetrically increased signal intensity in the cerebellar dentate nuclei, detectable on T2 FLAIR MR imaging7.
The differential diagnosis comprises congenital and hereditary conditions caused by toxic substances (alcohol) or drugs (including metronidazole), infectious and vascular diseases, vitamin deficiencies, tumors, paraneoplasms, etc.8. In our case, the condition presented acutely and the patient had not consumed alcohol for many years. Our initial hypothesis was that the findings observed were attributable to a complication of his primary infection, but the MRi proved us wrong by revealing lesions pathognomonic of pharmacological toxicity.
The World Health Organization's and Naranjo's9 causality assessments were performed. The causal relationship was defined as “likely” (for ethical reasons the treatment was not reintroduced after it had been withdrawn; the response to re-exposure to the drug was significant enough in both algorithms to be defined as “proven”). The patient was also being treated with ceftriaxone, but this drug was not considered a potential causative agent of the disease as no connection was established between both.
The large majority of cases reported tend to resolve following withdrawal of the drug; the lesions observed on MRi also tend to disappear8. However, in some cases symptoms may persist despite discontinuation of treatment10.
In summary, special consideration must be given to metronidazole-induced toxicity when performing a differential diagnosis of cerebellar syndrome, particularly in cirrhotic patients receiving high cumulative doses of the drug and being concomitantly treated with agents with the potential of elevating serum levels of metronidazole.
FoundingWithout financing.
Conflict of interestsThere are no conflicts of interest.