Community-acquired pneumonia (CAP) is associated with high morbidity and mortality rates. Despite methicillin-resistant Staphylococcus aureus (MRSA) having often been associated with nosocomial pneumonia, the condition of some MRSA CAP patients is severe enough to warrant their being admitted to ICU.
ObjectiveThe purpose of this study is to conduct a systematic review of the literature on antibiotic treatment of MRSA CAP in critically-ill patients.
Material and methodsAn online search was conducted for locating articles on MRSA CAP in critically ill patients. Relevant publications were identified in PUBMED, the BestPractice database, UpToDate database and the Cochrane Library for articles published in English within the December 2001 - April 2016 time frame.
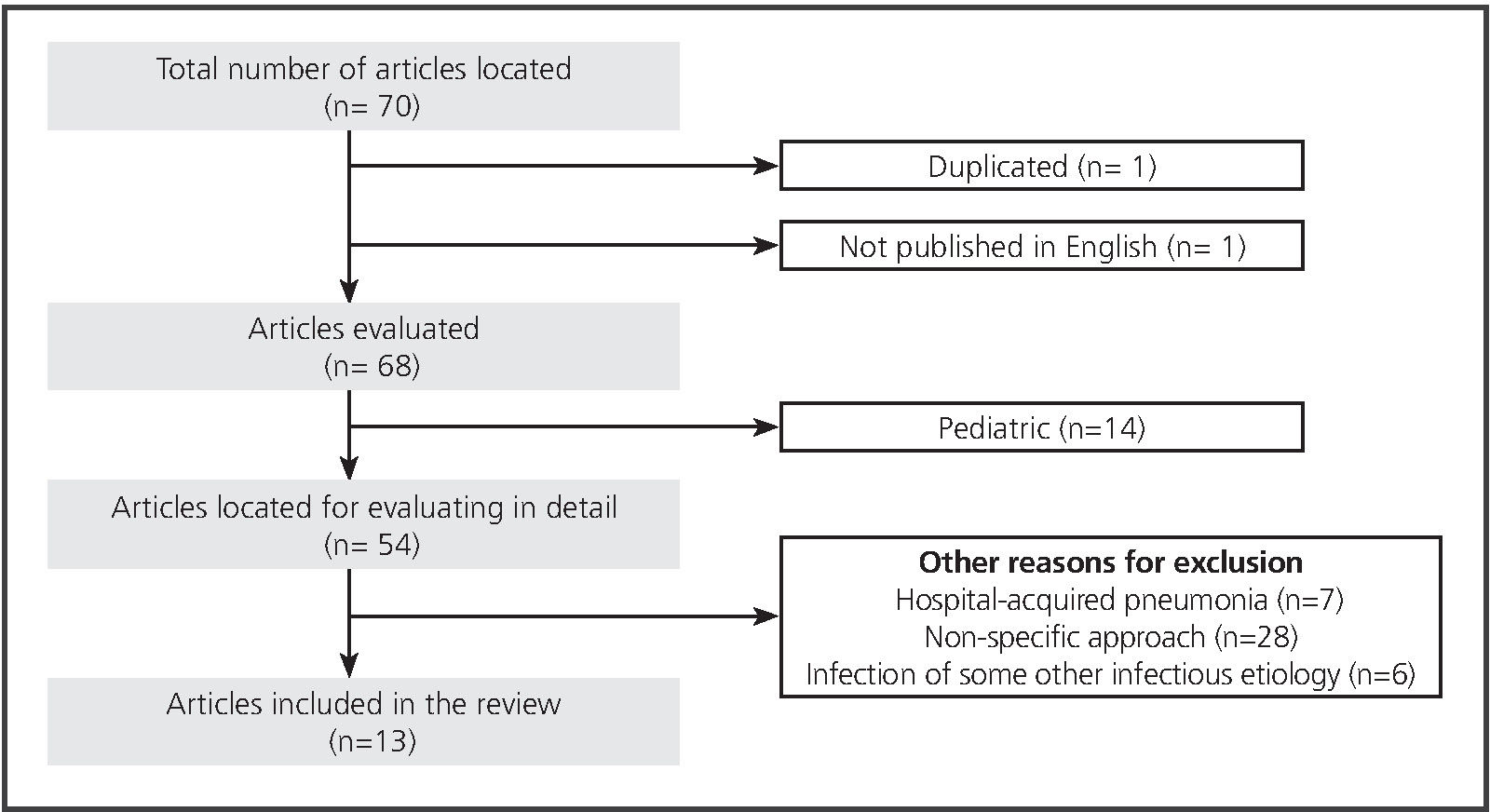
ResultsA total of 70 articles were found to have been published, 13 (18.8%) having been included and 57 (81.4%) excluded. Cohort studies were predominant, having totaled 16 in number (20.7%) as compared to one sole cross-sectional study (3.5%).
ConclusionsThe experience in the treatment of MRSA CAP in patients requiring admission to ICU is quite limited. Vancomycin or linezolid seem to be the treatments of choice for MRSA CAP, although there not be any specific recommendation in this regard. It may be useful to use alternative routes, such as administration via aerosolized antibiotics, continuous infusion or in association with other antibiotics.
La neumonía adquirida en la comunidad (NAC) está relacionada con unas tasas elevadas de morbi-mortalidad. A pesar de que Staphylococcus aureus resistente a meticilina (SARM) se ha relacionado frecuentemente con la neumonía nosocomial, algunos pacientes con NAC por este microorganismo revisten la suficiente gravedad como para precisar su ingreso en la UCI.
ObjetivosEfectuar una revisión sistemática de la literatura sobre el tratamiento antibiótico de la NAC por SARM en pacientes críticos.
Material y métodosSe realizó una búsqueda de artículos sobre NAC por SARM en el paciente crítico. Se identificaron las publicaciones pertinentes en PUBMED, BestPractice database, UpToDate database y Cochrane Plus Library para artículos publicados en inglés desde diciembre del 2001 hasta abril del 2016.
ResultadosSe encontraron 70 publicaciones, incluyendo 13 (18,8%) y excluyendo 57 (81,4%). Predominaron los estudios de cohortes con un total de 6 (20,7%), frente a una única publicación en forma de estudio transversal (3,5%).
ConclusionesLa experiencia en el tratamiento de la NAC por SARM en pacientes que precisen ingreso en la UCI es muy limitada. La vancomicina o el linezolid parecen ser las terapias en las que se dispone de una mayor experiencia, aunque no existe ninguna recomendación específica al respecto. Puede ser útil la utilización de vías alternativas como la nebulizada, administración en perfusión continua o en asociación con otros antibióticos.
Community-acquired pneumonia (CAP) is associated with high morbidity and mortality rates often giving rise to hospital admissions, especially among elderly patients1. In the “Global Burden of Disease Study”, the pneumonias within the context of lower respiratory tract infections were found to be the fourth-ranked cause of global mortality and the second-ranked cause of loss of potential years of life2. In a review conducted for the purpose of determining the incidence rate and the risk factors regarding CAP being acquired by adults in Europe, the major co-morbidities found to exist included chronic respiratory, cardiovascular and cerebrovascular diseases, Parkinson’s disease, epilepsy, dementia, dysphagia, HIV infection or chronic kidney or liver disease, which double or quadruple the probability of acquiring this disease3.
The CAP incidence in Europe rose from 1.07-1.20 to 1.54-1.70 cases per 1,000 persons per year3. A study conducted in the area of Tarragona involving the participation of 3 hospitals (Joan XXIII, Santa Tecla and Pius Hospital) and 8 primary care centers (Tarragona-Valls, Bonavista-La Canonja, Torreforta-La Granja, Sant Pere i Sant Pau, Tarraco, Sant Salvador, Salou and Valls) included 11,240 persons age 65 or older and showed the CAP incidence to increase significantly with age, having totaled an incidence of 9.90 cases per 1,000 persons per year within the 65-74 age range as compared to the 29.40 cases per 1,000 persons per year in persons over 85 years of age (p < 0,001)4.
Nosocomial pneumonia is one of the most frequent infections in critically-ill patients5. From the etiological standpoint, methicillin-resistant Staphylococcus aureus (MRSA) is one of the most prevalent microorganisms in this infection and may be found in 27% of the critically-ill patients who have this infectious disease6. Despite methicillin-resistant Staphylococcus aureus (MRSA) having often been associated with nosocomial pneumonia in patients admitted to ICU, MRSA CAP in Europe is estimated to fall within the range of 0.51-0.64 cases per 100,000 inhabitants, entailing a mortality rate of 10%-25% in patients requiring hospitalization7.
In order to select the best option for treating MRSA community-acquired pneumonia, it is indispensable to know both the clinical characteristics of the patients and the pharmacokinetic variations which have a bearing on the concentrations of the antibiotics used in their treatment, as well as their sensitivity to MRSA.
The purpose of this review is to conduct a systematic review of the literature on the antibiotic treatment of MRSA CAP in critically-ill patients.
Material and methodsA thorough online search was conducted of the bibliography published on MRSA CAP in critically-ill patients. The relevant publications were identified in PUBMED, the BestPractice database, UpToDate database and the Cochrane Plus Library for articles published in English within the December 2001 – April 2016 time frame. The key words used for this search were: “pneumonia” and “critically ill” or “intensive care unit” and “methicillin resistant staphylococcus aureus” and “community-acquired”. On the basis of the articles found in the search, a manual search was conducted in the reference lists for the purpose of identifying the relevant articles.
Figure 1 includes meta-analyses, systematic reviews and revisions, clinical trials, observational studies, clinical practice manuals, consensus conferences and abstracts in English. Those articles on in-vitro efficacy, animal model studies, pediatric studies and those not including a diagnosis of CAP or whenever the article included CAP of a different etiology and did not make a specific analysis of the results of the MRSA CAP cases, termed as being non-specific in approach, were excluded. Two independent reviewers took part in the process of selecting the articles and, in view of any discrepancy, a third senior reviewer having made the selection.
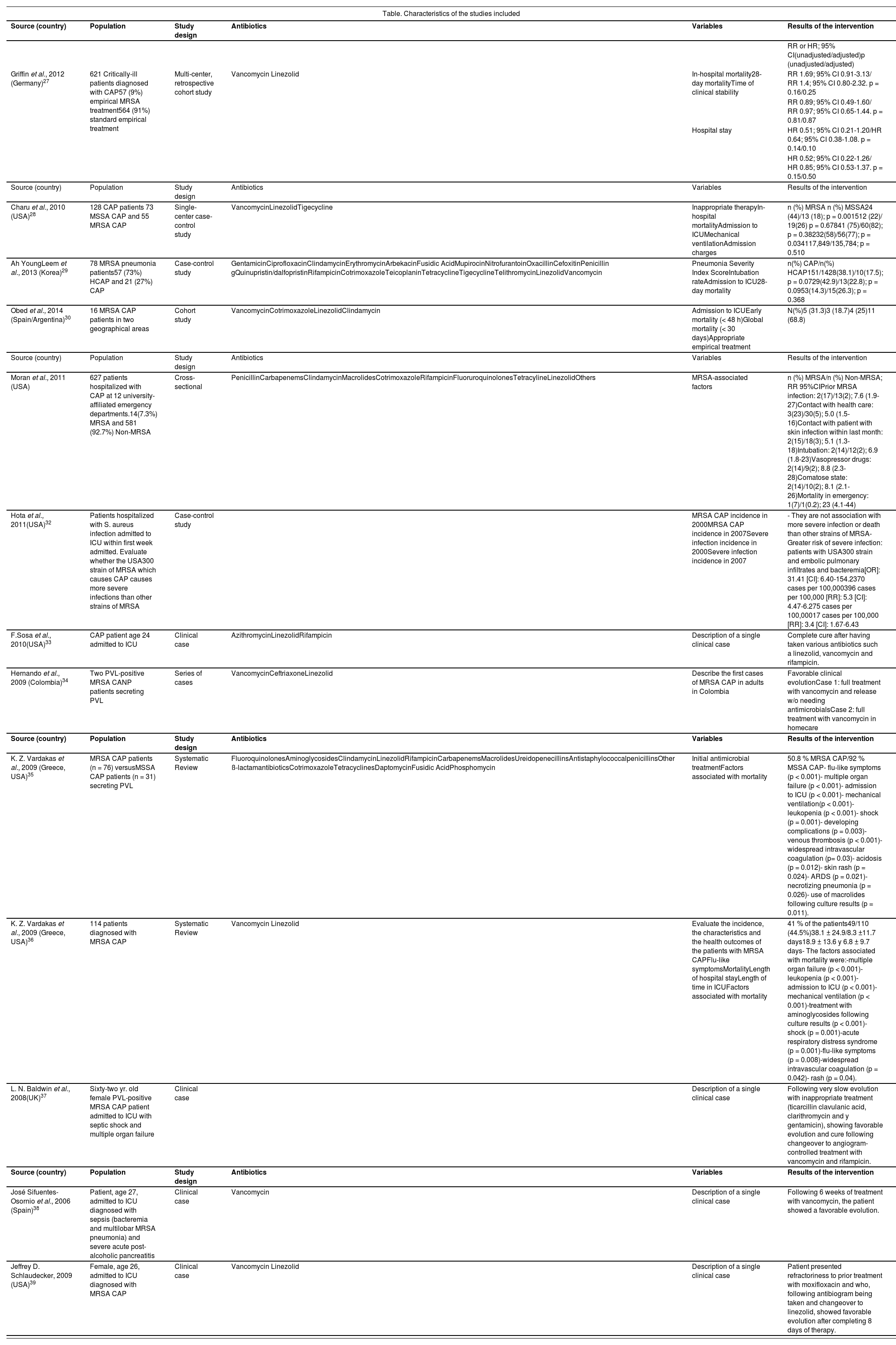
ResultsA total of 70 potentially-relevant articles were identified. After having conducted a complete review of the texts, a total of 13 studies (18.84%) met the requirements for inclusion, a total of 57 (81.4%) having been excluded (Table 1). The cohort studies were predominant, having totaled six in number (20.69%) as compared to one sole article published on a cross-sectional study (3.45%).
Results of the published studies
| Table. Characteristics of the studies included | |||||
|---|---|---|---|---|---|
| Source (country) | Population | Study design | Antibiotics | Variables | Results of the intervention |
| RR or HR; 95% CI(unadjusted/adjusted)p (unadjusted/adjusted) | |||||
| Griffin et al., 2012 (Germany)27 | 621 Critically-ill patients diagnosed with CAP57 (9%) empirical MRSA treatment564 (91%) standard empirical treatment | Multi-center, retrospective cohort study | Vancomycin Linezolid | In-hospital mortality28-day mortalityTime of clinical stability | RR 1.69; 95% CI 0.91-3.13/ RR 1.4; 95% CI 0.80-2.32. p = 0.16/0.25 |
| RR 0.89; 95% CI 0.49-1.60/ RR 0.97; 95% CI 0.65-1.44. p = 0.81/0.87 | |||||
| Hospital stay | HR 0.51; 95% CI 0.21-1.20/HR 0.64; 95% CI 0.38-1.08. p = 0.14/0.10 | ||||
| HR 0.52; 95% CI 0.22-1.26/ HR 0.85; 95% CI 0.53-1.37. p = 0.15/0.50 | |||||
| Source (country) | Population | Study design | Antibiotics | Variables | Results of the intervention |
| Charu et al., 2010 (USA)28 | 128 CAP patients 73 MSSA CAP and 55 MRSA CAP | Single-center case-control study | VancomycinLinezolidTigecycline | Inappropriate therapyIn-hospital mortalityAdmission to ICUMechanical ventilationAdmission charges | n (%) MRSA n (%) MSSA24 (44)/13 (18); p = 0.001512 (22)/ 19(26) p = 0.67841 (75)/60(82); p = 0.38232(58)/56(77); p = 0.034117,849/135,784; p = 0.510 |
| Ah YoungLeem et al., 2013 (Korea)29 | 78 MRSA pneumonia patients57 (73%) HCAP and 21 (27%) CAP | Case-control study | GentamicinCiprofloxacinClindamycinErythromycinArbekacinFusidic AcidMupirocinNitrofurantoinOxacillinCefoxitinPenicillin gQuinupristin/dalfopristinRifampicinCotrimoxazoleTeicoplaninTetracyclineTigecyclineTelithromycinLinezolidVancomycin | Pneumonia Severity Index ScoreIntubation rateAdmission to ICU28-day mortality | n(%) CAP/n(%) HCAP151/1428(38.1)/10(17.5); p = 0.0729(42.9)/13(22.8); p = 0.0953(14.3)/15(26.3); p = 0.368 |
| Obed et al., 2014 (Spain/Argentina)30 | 16 MRSA CAP patients in two geographical areas | Cohort study | VancomycinCotrimoxazoleLinezolidClindamycin | Admission to ICUEarly mortality (< 48 h)Global mortality (< 30 days)Appropriate empirical treatment | N(%)5 (31.3)3 (18.7)4 (25)11 (68.8) |
| Source (country) | Population | Study design | Antibiotics | Variables | Results of the intervention |
| Moran et al., 2011 (USA) | 627 patients hospitalized with CAP at 12 university-affiliated emergency departments.14(7.3%) MRSA and 581 (92.7%) Non-MRSA | Cross-sectional | PenicillinCarbapenemsClindamycinMacrolidesCotrimoxazoleRifampicinFluoruroquinolonesTetracylineLinezolidOthers | MRSA-associated factors | n (%) MRSA/n (%) Non-MRSA; RR 95%CIPrior MRSA infection: 2(17)/13(2); 7.6 (1.9-27)Contact with health care: 3(23)/30(5); 5.0 (1.5-16)Contact with patient with skin infection within last month: 2(15)/18(3); 5.1 (1.3-18)Intubation: 2(14)/12(2); 6.9 (1.8-23)Vasopressor drugs: 2(14)/9(2); 8.8 (2.3-28)Comatose state: 2(14)/10(2); 8.1 (2.1-26)Mortality in emergency: 1(7)/1(0.2); 23 (4.1-44) |
| Hota et al., 2011(USA)32 | Patients hospitalized with S. aureus infection admitted to ICU within first week admitted. Evaluate whether the USA300 strain of MRSA which causes CAP causes more severe infections than other strains of MRSA | Case-control study | MRSA CAP incidence in 2000MRSA CAP incidence in 2007Severe infection incidence in 2000Severe infection incidence in 2007 | - They are not association with more severe infection or death than other strains of MRSA- Greater risk of severe infection: patients with USA300 strain and embolic pulmonary infiltrates and bacteremia[OR]: 31.41 [CI]: 6.40-154.2370 cases per 100,000396 cases per 100,000 [RR]: 5.3 [CI]: 4.47-6.275 cases per 100,00017 cases per 100,000 [RR]: 3.4 [CI]: 1.67-6.43 | |
| F.Sosa et al., 2010(USA)33 | CAP patient age 24 admitted to ICU | Clinical case | AzithromycinLinezolidRifampicin | Description of a single clinical case | Complete cure after having taken various antibiotics such a linezolid, vancomycin and rifampicin. |
| Hernando et al., 2009 (Colombia)34 | Two PVL-positive MRSA CANP patients secreting PVL | Series of cases | VancomycinCeftriaxoneLinezolid | Describe the first cases of MRSA CAP in adults in Colombia | Favorable clinical evolutionCase 1: full treatment with vancomycin and release w/o needing antimicrobialsCase 2: full treatment with vancomycin in homecare |
| Source (country) | Population | Study design | Antibiotics | Variables | Results of the intervention |
| K. Z. Vardakas et al., 2009 (Greece, USA)35 | MRSA CAP patients (n = 76) versusMSSA CAP patients (n = 31) secreting PVL | Systematic Review | FluoroquinolonesAminoglycosidesClindamycinLinezolidRifampicinCarbapenemsMacrolidesUreidopenecillinsAntistaphylococcalpenicillinsOther ß-lactamantibioticsCotrimoxazoleTetracyclinesDaptomycinFusidic AcidPhosphomycin | Initial antimicrobial treatmentFactors associated with mortality | 50.8 % MRSA CAP/92 % MSSA CAP- flu-like symptoms (p < 0.001)- multiple organ failure (p < 0.001)- admission to ICU (p < 0.001)- mechanical ventilation(p < 0.001)- leukopenia (p < 0.001)- shock (p = 0.001)- developing complications (p = 0.003)- venous thrombosis (p < 0.001)- widespread intravascular coagulation (p= 0.03)- acidosis (p = 0.012)- skin rash (p = 0.024)- ARDS (p = 0.021)- necrotizing pneumonia (p = 0.026)- use of macrolides following culture results (p = 0.011). |
| K. Z. Vardakas et al., 2009 (Greece, USA)36 | 114 patients diagnosed with MRSA CAP | Systematic Review | Vancomycin Linezolid | Evaluate the incidence, the characteristics and the health outcomes of the patients with MRSA CAPFlu-like symptomsMortalityLength of hospital stayLength of time in ICUFactors associated with mortality | 41 % of the patients49/110 (44.5%)38.1 ± 24.9/8.3 ±11.7 days18.9 ± 13.6 y 6.8 ± 9.7 days- The factors associated with mortality were:-multiple organ failure (p < 0.001)-leukopenia (p < 0.001)-admission to ICU (p < 0.001)-mechanical ventilation (p < 0.001)-treatment with aminoglycosides following culture results (p < 0.001)-shock (p = 0.001)-acute respiratory distress syndrome (p = 0.001)-flu-like symptoms (p = 0.008)-widespread intravascular coagulation (p = 0.042)- rash (p = 0.04). |
| L. N. Baldwin et al., 2008(UK)37 | Sixty-two yr. old female PVL-positive MRSA CAP patient admitted to ICU with septic shock and multiple organ failure | Clinical case | Description of a single clinical case | Following very slow evolution with inappropriate treatment (ticarcillin clavulanic acid, clarithromycin and y gentamicin), showing favorable evolution and cure following changeover to angiogram-controlled treatment with vancomycin and rifampicin. | |
| Source (country) | Population | Study design | Antibiotics | Variables | Results of the intervention |
| José Sifuentes-Osornio et al., 2006 (Spain)38 | Patient, age 27, admitted to ICU diagnosed with sepsis (bacteremia and multilobar MRSA pneumonia) and severe acute post-alcoholic pancreatitis | Clinical case | Vancomycin | Description of a single clinical case | Following 6 weeks of treatment with vancomycin, the patient showed a favorable evolution. |
| Jeffrey D. Schlaudecker, 2009 (USA)39 | Female, age 26, admitted to ICU diagnosed with MRSA CAP | Clinical case | Vancomycin Linezolid | Description of a single clinical case | Patient presented refractoriness to prior treatment with moxifloxacin and who, following antibiogram being taken and changeover to linezolid, showed favorable evolution after completing 8 days of therapy. |
CA-MRSA: Community-acquired methicillin-resistant Staphylococcus aureus
RR: Relative Risk
HR: Hazard Radio
OR: Odds Ratio
CI: Confidence Interval
CAP: Community-acquired pneumonia
HAP: Hospital-acquired pneumonia
ICU: Intensive Care Unit
MRSA: Methiccillin-resistant Staphylococcus aureus
MSSA: Methicillin-sensitive Staphylococcus aureus
HCAP: Healthcare-associated pneumonia
PVL: Panton-Valentine Leukocidin
The information available on the treatment of MRSA community-acquired pneumonia in patients requiring admission to ICU is quite limited. This paucity of information could be due to the studies having focused mainly on nosocomial pneumonias. However, this disease shows itself to be significantly relevant in clinical practice, given that it is associated with a high mortality rate8.
In the present systematic review, the predominant treatment in this infectious entity was found to be vancomycin. In addition thereto, as a major limitation, the studies have focused on populations affected by different etiological agents and not solely on MRSA, which totaled only a minor percentage.
Vancomycin has been the treatment of choice in recent years. However, the difficulty of achieving therapeutic levels at the pulmonary level, in conjunction with the current controversy concerning the influence of the minimum inhibitory concentration (MIC) on the efficacy of vancomycin has led to other treatment alternatives being sought9. In this regard, MRSA strains with a MIC for vancomycin ≥ 1.5 mcg/ml have been found to be associated with worse clinical outcomes in different types of infections10.
However, one must bear in mind that none of the studies analyzed specifically deal with the impact of higher vancomycin MICs on the prognosis of MRSA CAP patients, unlike what has been studied in MRSA nosocomial pneumonia11.
To deal with all of these limitations, the combination of rifampicin and vancomycin has recently been evaluated in one review, showing a possible benefit on the treatment of MRSA pneumonia, although it has not as yet been specifically evaluated in MRSA CAP11.
Linezolid is an antibiotic which has widely demonstrated its efficacy in treating pneumonia9, although no specific experience in MRSA CAP currently be available. However, given its ability to reach high concentrations in the pulmonary epithelial lining fluid12,13, it could be an effective alternative for the treatment of MRSA community-acquired pneumonia. Additionally, its use could be especially indicated in patients diagnosed with MRSA CAP who produce Panton-Valentine Leukocidin (PVL), taking into account the ability of linezolid to inhibit the production of this toxin14,15. Another of the advantages of using linezolid is its excellent pharmacokinetics, making a sequenced treatment from the intravenous route to the oral route possible due to its 100% bioavailability16.
Other antibiotics available on the market for treating MRSA CAP are telavancin, ceftobiprole (neither of which are not marketed in Spain), ceftaroline, clindamycin and cotrimoxazole. Telavancin has not been evaluated for MRSA CAP, but rather for the treatment of the hospital-acquired pneumonia (HAP) caused by this microorganism17. As far as the two cephalosporins are concerned, the only published studies available provide a low degree of scientific evidence, such cohort studies including a small number of patients or case series. In the case of the use of ceftobiprole, a clinical study is available comparing it to ceftriaxone, making it possible to add linezolid to this branch in view of clinical signs and symptoms of suspected MRSA18. This study revealed ceftobiprole not to be inferior to the drug with which it was compared. As far as the use of ceftaroline in CAP, there are only two clinical trials available, but they excluded patients admitted to the ICU in whom MRSA infection was confirmed.
The use of clindamycin is described only to a minor degree in patients diagnosed with MRSA CAP. However, the use of clindamycin associated with linezolid provided good results in comparison to the vancomycin and rifampicin combination, given its ability to block PVL in the case of a critically-ill patient diagnosed with MRSA CAP.15.
As far as cotrimoxazole is concerned, just as in the case of clindamycin, there is little evidence as to its use in MRSA CAP. Bearing in mind the major activity of both of these antimicrobials combatting out-of-hospital MRSA strains, as well as their easy handling on being possible to administer orally or intravenously, they theoretically seem to be treatment alternatives of interest for the treatment of MRSA CAP19. However, it is advisable to stress the absence of clinical evidence of these antibiotics for this indication.
Critically-ill patients show widely-varying pharmacokinetics regarding antibiotics20. Multiple organ failure, increased volume of distribution (hypoalbuminemia, resuscitation fluids, shock, edemas…), as well as the use of vasoactive drugs and extracorporeal circuits can give rise to a high degree of variability in the plasma concentrations20. As a result of all of the foregoing, different treatment strategies have been studied in an attempt to achieve a greater stability in the plasma concentrations, such as the administration of antibiotics in continuous infusion for those of time-dependent bactericidal activity.
This high degree of variability in the plasma concentrations gives rise to a great deal of uncertainty regarding the final quantity of antimicrobial reaching the site of infection, the lung in this case. In this regard, more selective administration routes have been studied, making it possible to achieve a higher concentration at the site of infection with less of a risk of adverse systemic effects. One such technique is the administration of aerosolized antibiotics.
In the present review, all of the studies analyzed the different treatments for MRSA CAP when the antimicrobials were administered as in standard practice, that is to say, in intermittent intravenous infusion. However, there are alternative treatment strategies, given that both linezolid and vancomycin could be administered in continuous infusion, and other administration routes could be used, such as via aerosolized administration, although there is no information of MRSA CAP.
Continuous infusion of vancomycin has not shown itself to provide efficacy-related benefits in comparison to intermittent administration in patients with different diseases, although it apparently might cause a lesser degree of nephrotoxicity22. However, its potential benefit in MRSA CAP is unknown, given that it has not been studied specifically.
In the case of linezolid, limited information exists on its administration in continuous infusion, said information having to do mainly with HAP23. A clinical case was presented recently in the form of a poster and oral presentation involving a critically-ill patient diagnosed with MRSA necrotizing pneumonia. After having initially undergone treaty with vancomycin, given the resulting poor evolution, linezolid in continuous infusion was started at higher than standard dosages of 600 mg/12 h, which enable the patient to show a proper evolution with clinical cure24.
Another more innovative strategy with a promising future lies in the administration of certain aerosolized antibiotics, given that the concentrations reached in the pulmonary lining fluid can be of less than 50% of those detected via plasma25. One of the possible tools for remedying this problem would be the use of aerosolized antibiotics, the use of which is scarcely reported in the literature. This administration route makes it possible to achieve local levels much higher than the serum levels (by following a suitable technique, the levels could be increased by up to 650%)25, with a lower systemic concentration of antibiotic and hence a lesser risk of adverse effects26.
ConclusionsMyriad active molecules are available for combating MRSA which have been used in the treatment of pneumonia, although the experience in patients with MRSA CAP requiring admission to ICU is quite limited. Especially in critically-ill patients, vancomycin or linezolid are apparently the treatments of choice for treating MRSA CAP, although there not be any specific recommendation in this regard. The clinical pharmacist may be useful in recommending and providing advice concerning alternative strategies for administering certain specific antibiotics, such as linezolid or vancomycin, both of which can be administered in continuous infusion or in association with other antibiotics. Clinical pharmacists may also be useful in assessing alternative routes, such as aerosolized, all of which are options with a promising future in treating this disease.
However, the clinical efficacy of these treatment strategies has not been evaluated in MRSA CAP, thus substantiating the need of conducting future studies on this infectious disease with a high morbidity and mortality rate.
- Inicio
- Todos los contenidos
- Publique su artículo
- Acerca de la revista
- Métricas