To evaluate treatment persistence and dosing interval extension with faricimab in neovascular age-related macular degeneration (nAMD) in real-world practice.
MethodsRetrospective observational study conducted in a tertiary hospital (March 2024–March 2025). Patients receiving faricimab (treatment-naïve or pre-treated with anti-VEGF therapy), with ≥1 post-loading dose, were included. Dosing intervals were analyzed at baseline, 6 and 12 months, Adherence was assessed with the medication possession ratio (MPR), with >80% considered adherent. Persistence was defined as the time from treatment initiation to discontinuation or end of follow-up. Persistence was estimated using Kaplan–Meier survival analysis.
ResultsWe included 129 patients (148 eyes), mean age 74.5 ± 8.85 years; 55% were female. A total of 39 patients (30.2%) were treatment-naïve and 90 (69.8%) were pretreated. At 12 months, 48.8% of naïve and 55.5% of pretreated patients achieved 8–12 weeks intervals. Mean persistence was 12.2 months (SD 0.2; 95% CI: 11.8–12.6). The median was not reached by the end of the study. Persistence rate was 93% at 6 and 12 months. Only one patient discontinued due to inefficacy. No serious adverse events or endophthalmitis occurred.
ConclusionsFaricimab showed excellent persistence and extended dosing intervals in real-world practice. This is the first study specifically evaluating faricimab real-world persistence in nAMD.
Evaluar persistencia e intervalo de administración de faricimab en la degeneración macular asociada a la edad neovascular (DMAEn) en práctica clínica real.
MétodosEstudio observacional retrospectivo. Se incluyeron pacientes pretratados y no pretratados con anti-VEGF que recibieron faricimab entre marzo 2024–2025. Se analizaron los intervalos de dosificación al inicio, a los 6 y 12 meses, incluyendo únicamente a aquellos pacientes que recibieron al menos una dosis tras la fase de carga. Las tasas de persistencia se estimaron mediante análisis de supervivencia de Kaplan–Meier.
ResultadosSe incluyeron 129 pacientes (148 ojos), edad media 74,5 ± 8,85 años; 55% mujeres. 39 pacientes (30,2%) no pretratados y 90 (69,8%) pretratados con anti-VEGF. A los 12 meses, el 48,8% de los no pretratados y el 55,5% de los pretratados alcanzaron intervalos de 8–12 semanas. La persistencia media fue 12,2 meses (DE 0,2; IC 95%: 11,8–12,6), sin alcanzarse la mediana al finalizar el estudio. La tasa acumulada de persistencia fue del 93% a los 6 y 12 meses. Un paciente interrumpió el tratamiento por ineficacia. No se notificaron eventos adversos graves ni endoftalmitis.
ConclusionesFaricimab mostró una excelente persistencia y capacidad para extender los intervalos de dosificación en práctica clínica real.
Neovascular age-related macular degeneration (nAMD) is a leading cause of visual loss in older adults, and anti-vascular endothelial growth (VEGF) therapy has transformed its management, although frequent injections challenge a long-term adherence and treatment sustainability. According to the World Health Organization (WHO), adherence is the extent to which a person's behavior corresponds with agreed recommendations from a healthcare provider. Faricimab, a novel bispecific antibody targeting VEGF-A and angiopoietin-2 (Ang-2), demonstrated efficacy and safety in the TENAYA and LUCERNE trials were over 60% of patients maintained visual acuity with intervals extended up to 16 weeks.1,2 However, real-world evidence regarding faricimab persistence and dosing intervals remains limited. Persistence in this study is defined as the time from the first to the last faricimab injection before permanent discontinuation or switch, irrespective of the underlying cause. It integrates effectiveness, safety, adherence, and patient satisfaction.3 The objective of this study was to evaluate persistence taking into account adherence, retention rate and treatment interval extension with faricimab in patients with nAMD.
MethodThe team of hospital pharmacists retrospectively reviewed medical records of patients with nAMD between March 2024 and March 2025. Eligible patients received the complete loading phase of faricimab plus at least 1 additional injection. Both treatment-naïve and anti-VEGF pre-treated patients were included; those discontinuing after the loading phase were excluded.
Data extracted from electronic health records (HER) Integrador® and Abucasis® and Oncopharm® software included baseline characteristics, prior anti-VEGF treatments, dosing intervals, and adverse events. Faricimab was administered according to local protocols: four monthly loading doses followed by a Treat-and-Extend regimen with dosage frequency adjusted based on visual acuity, central macular thickness, and the presence of intra/subretinal fluid. In cases of anatomical or functional worsening, treatment intervals were shortened.4
Variables analyzed included sex, age, diagnosis, treatment initiation date, line of therapy, and number of treatment discontinuations. Reasons for discontinuation were not systematically collected, as this information was not consistently documented in HER. We also collected 12-month persistence, as well as patient distribution and persistence stratified by treatment-naïve and pretreated patients. Dosing intervals were assessed at baseline, 6 and 12 months. We calculated persistence in at least 6-month treated patients.
However, persistence is a multidimensional concept encompassing treatment duration, effectiveness and safety. In our study, we focused on the temporal component while evaluating clinical outcomes separately as complementary indicators of persistence. If the patient remained on treatment at the study's end, persistence was considered ongoing at the last documented visit, regardless of whether this could exceed the planned 12 months of follow-up. Discontinuation was defined as the absence of an injection within twice the planned interval plus a 2-week grace period. Patients lost to follow-up were represented as such in Kaplan–Meier curves. We also use the concept of retention rate to describe the proportion of patients remaining on treatment over time.
In bilateral cases, injections were administered simultaneously. Therefore, persistence analyses were conducted using the patient, as the unit of reference.
Statistical analyses were performed using SPSS Statistics v23.0®, using Pearson's chi-square test for categorical variables (reported as frequencies), and as means and standard deviations (SDs) when normally distributed (Shapiro–Wilk test), or as medians and interquartile ranges (IQRs) when not for continuous variables. Persistence was estimated using Kaplan–Meier survival curves.
Adherence was measured using the Medication Possession Ratio (MPR = total days covered by the dispensed doses/ total number of days in the observation period). Patients with MPR ≥80% were classified as adherent.5 Dispensing date was used as the reference, which coincided with the injection date. The study was approved by the hospital's Clinical Research Ethics Committee and conducted according to the Declaration of Helsinki.
ResultsA total of 129 patients (148 eyes) treated with intravitreal faricimab between March 2024 and March 2025 were included. 39 patients (43 eyes) were treatment-naïve, 90 patients (105 eyes) pre-treated. A total of 63 patients received aflibercept previously, and 27 received ranibizumab. Aflibercept dosing intervals were: 38.1% of patients treated every 4 weeks, 25.3% every 6 weeks, 17.4% every 8 weeks, and 19.2% longer than 8 weeks. For ranibizumab, 70.4% were treated every 4 weeks and 29.6% at longer intervals.
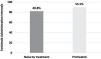
For naïve patients, planned faricimab dosing intervals were: 28.1% every 4 weeks, 24.1% every 6 weeks, and 48.8% achieved intervals of ≥8–12 weeks. In pretreated patients, 33.5% were treated every 4 weeks, 11.1% every 6 weeks, and 55.5% achieved intervals of ≥8–12 weeks (Fig. 1).
Three patients only received the loading dose. Two of them were due to referral to another center, resulting in loss to follow-up, and the other interruption was by the patient's decisión.
Ninety patients (105 eyes) (69.7%) completed at least 6 months of faricimab treatment. Their mean persistence was 12.2 months (SD 0.2; 95% CI: 11.8–12.6). The median was not reached by the end of the study. The cumulative persistence rate was 93% at 6 and 12 months. A total of 126 of the 129 patients analyzed were still on treatment at the end of the study. A summary of baseline characteristics, dosing intervals, adherence, and persistence outcomes is provided in Table 1.
Baseline characteristics, dosing intervals, adherence, and persistence outcomes.
| Variable | Result |
|---|---|
| Patients, n (eyes) | 129 (148) |
| Age, mean ± SD (years) | 74.5 ± 8.85 |
| Female, % | 55.0 |
| Naïve patients, n (%) | 39 (30.2) |
| Pretreated patients, n (%) | 90 (69.8) |
| Naïve dosing intervals at 12 mo: 4w/6w/≥8–12w (%) | 28.1/24.1/48.8 |
| Pretreated dosing intervals at 12 mo: 4w/6w/≥8–12w (%) | 33.5/11.1/55.5 |
| Persistence at 12 months (%) | 93 |
| Discontinuations, n | 1 (lack of efficacy) |
Subgroup analysis showed that pretreated patients had a mean persistence of 10.1 SD 2.1 months (with one discontinuation due to inefficacy), with a global retention rate of 98.9%. Naïve patients had a persistence of 9.9 SD 1.9 months and a 100% retention rate (Fig. 2). Regarding safety, no cases of endophthalmitis or serious adverse events associated with faricimab were reported.
DiscussionThis study focused on the temporal aspect of persistence, which represents one dimension of the broader, multidimensional concept, and demonstrates that extended dosing intervals are achievable while maintaining excellent persistence in both naïve and pretreated eyes. More than 50% of real-world patients (naïve or pre-treated) reached ≥8-week intervals in the first year. This sustained extension beyond intervals established in the Summary of Product Characteristics (SPCs) suggests that many patients can receive fewer annual injections without compromising treatment efficacy. This aligns with the pivotal TENAYA and LUCERNE trials, which reached almost 84% 24-month persistence among 665 treatment-naïve nAMD patients. This reinforces that our real-world findings are consistent with expectations from controlled clinical trial settings.1,2 A systematic review by Tahmasebi et al. analyzed 629 pre-treated eyes with persistent DME. After switching to faricimab, the mean injection interval increased by 1.53 weeks. More than 50% of patients achieved extended intervals, although yearly persistence was not directly measured. Still, sustained interval extension suggests improved persistence.6 Janmohamed et al. retrospectively analyzed 215 nAMD eyes pre-treated with anti-VEGF and switched to faricimab. After one year, injection intervals doubled (median: from 4 to 8 weeks), and 63.7% of patients achieved ≥8-week intervals.7
Recent studies further support the use of persistence as an integrated metric of effectiveness, safety, and adherence. A German database study including 5498 nAMD and 484 DME patients found that over 50% of nAMD and over 60% of DME/Diabetic retinopathy patients were non-persistent with anti-VEGF (ranibizumab or aflibercept) in the first year. Risk factors for non-persistence included older age, female sex, high level of care, and use of ranibizumab vs. aflibercept.8
Persistence reflects the period between treatment initiation and discontinuation, or the time during which a drug remains a suitable option for a patient. This concept is gaining recognition, even being proposed by some authors as part of the “6P” model of personalized medicine, expanding the traditional “5P” model by adding persistence to reflect the real-world value of therapy.3
Our data confirm that faricimab shows excellent persistence and retention, with a mean of 12.2 months and 93% cumulative persistence at 12 months. As 126 of 129 patients remained on treatment at study end, persistence rates could be even higher over a longer follow-up. While these findings are still maturing, faricimab emerges as a highly efficient and sustainable alternative to other anti-VEGF. A key strength of our study is that patients were considered adherent based on MPR data. This enhances the generalizability and reliability of persistence findings for clinical practice.3 MPR tends to overestimate adherence when used as a sole method. However, persistence provides a robust complementary indicator of treatment outcomes, safety, and adherence/satisfaction in nAMD.
Limitations include the small sample size, lack of anatomical or functional outcomes (e.g., visual acuity and macular thickness), and its retrospective design. The main methodological limitation is the lack of systematic data regarding reasons for treatment discontinuation or non-adherence. Persistence is influenced by multiple factors beyond efficacy and safety (intercurrent medical events, logistical barriers, and patient-related circumstances). The absence of documentation in our retrospective review did not allow us to differentiate among these causes. Future prospective studies should include discontinuation reasons in order to provide a more comprehensive understanding of persistence. In this regard, we also lacked systematic information on the cause of discontinuation of previous treatments in pre-treated patients.
Economically, extending dosing intervals in more than 50% patients could reduce annual injections compared to the SPC expectations. Fewer injections enhance adherence and decrease treatment burden and costs, allowing more patients to be treated within existing budgets.
Although treatment safety was not one of the objectives of the study, reviewing the clinical histories, we observed a good safety profile with no serious adverse reactions or cases of endophthalmitis.
In conclusion, faricimab demonstrated excellent persistence and allowed treatment interval extension, reducing annual injections and improving efficiency compared to the SPC. Systematically incorporating persistence as a complementary outcome may enhance therapeutic decisions and health policy in chronic diseases such as nAMD. To our knowledge, this is the first study specifically evaluating the real-world persistence of faricimab in nAMD.
Contribution to the scientific literatureThis study provides new real-world evidence on the persistence and dosing interval optimization of faricimab in neovascular age-related macular degeneration. Unlike pivotal clinical trials, it evaluates treatment behavior in routine clinical practice, demonstrating excellent persistence and extended intervals with minimal discontinuations. Its originality lies in being the first study specifically focused on real-world faricimab persistence, supporting its relevance for optimizing anti-VEGF treatment strategies and healthcare efficiency.
The work has not been previously published, nor is it under review by any other journal.
The instructions for manuscript submission and ethical responsibilities have been taken into account, including ensuring that all signing authors meet the authorship requirements and have declared no conflicts of interest.”
CRediT authorship contribution statementSilvia Cornejo-Uixeda: Writing – review & editing, Writing – original draft, Validation, Methodology, Investigation, Funding acquisition, Formal analysis, Data curation, Conceptualization. Joaquín Borrás-Blasco: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision, Methodology, Formal analysis. Alejandro Valcuende-Rosique: Writing – review & editing, Validation, Software, Methodology, Formal analysis. Leonor Perez Gil: Writing – review & editing, Validation, Supervision. Nuria Monteagudo-Martinez: Writing – review & editing, Validation, Supervision, Methodology, Investigation. Virginia Merino: Writing – review & editing, Validation, Supervision.
FundingThe authors received no financial support for the research, authorship, and/or publication of this article.
The authors have no affiliations with or financial interest in any company or organization that could conflict with the views expressed in this manuscript.