Antimicrobial Stewardship Programs (ASPs) have appeared as very useful tools in order to improve the use of antimicrobial agents. The objective of this study is to assess the impact of an ASP on haematological patients hospitalized in an Intensive Care Unit (ICU).
MethodsA quasi-experimental pre-post intervention study, which included haematological patients admitted to an ICU and assessed by the ASP program during 3 years. The impact of the program on patient evolution was assessed by comparison between the previous period and the intervention period in terms of mortality, mean stay, number of re-hospitalizations, and duration of mechanical ventilation for intubated patients.
ResultsThe ASP team assessed 324 antimicrobial agents in 169 patients; they recommended 121 modifications, including 55 treatment discontinuations. Compared with the pre-intervention period, there were no significant differences in the variables assessed. No variation was observed in colonization by multi-resistant bacteria.
ConclusionsThe implementation of an APS on critical haematological patients will lead to a relevant number of treatment modifications, without any impact on the clinical evolution of patients.
Los programas de optimización de antimicrobianos (PROA) han surgido como herramientas de gran utilidad para mejorar el uso de estos. El objetivo del presente estudio es evaluar el impacto de un PROA sobre pacientes hematológicos ingresados en una unidad de pacientes críticos.
MétodosEstudio cuasi-experimental pre-post intervención. Se incluyeron pacientes hematológicos ingresados en una unidad de críticos evaluados por el equipo PROA durante 3 años. El impacto del programa sobre la evolución de los pacientes se evaluó mediante la comparación entre el periodo previo y de intervención de la mortalidad, estancia media, número de reingresos y duración de ventilación mecánica en los pacientes intubados.
Resultados324 antimicrobianos de 169 pacientes fueron evaluaron por el equipo PROA, recomendando un total de 121 modificaciones, incluyendo 55 suspensiones de tratamiento. Comparados con el periodo pre-intervención, no se observaron diferencias significativas en las variables consideradas. No se observó variación en la colonización por bacterias multirresistentes.
ConclusionesLa implantación de un PROA sobre el paciente crítico hematológico conduce a un número relevante de modificaciones en el tratamiento, sin afectar la evolución clínica de los pacientes.
Infection management in the haematological patient admitted in an Intensive Care Unit represents a high-complexity challenge. The severe consequences of inadequate treatment on prognosis will frequently lead to the prescription for these patients of multiple antimicrobial agents during long periods of time. However, this situation presents some risks, such as the development of adverse events, and the selection of multi-resistant strains. This article shows our experience after implementing an Antimicrobial Stewardship program for this group of high-complexity patients without any previous experience prescribed. Our outcomes show that antimicrobial prescription for this group of patients presents a major number of opportunities for improvement, and reinforces the need to implement this type of programs in these units.
IntroductionBacterial or fungal infection is a frequent cause of morbimortality in patients with haematological disease, particularly during neutropenia episodes1. In fact, around 20-30% of these patients will develop severe sepsis during their disease2,3 and up to 7% of patients can develop an invasive fungal infection4. The number of patients with immunosuppression has increased significantly during recent years, due to the increase in the number of aggressive treatments for the disease, the increasing number of transplants, and an increase in the age of the population receiving said treatments5. The application of these aggressive therapies, chemotherapy toxicity, deep immunosuppression induced during prolonged periods of time, and the development of the graft-against-host disease, will lead to severe complications that entail admitting these patients in Intensive Care Units (ICUs).
During the last decades, there has been a significant increase in bacterial resistances to antimicrobial agents, and this is particularly important in oncohae-matological patients. In these units, there has been a particularly relevant increase in resistances of enterobacteriaceae to betalactam antibiotics, and resistances to multiple antimicrobial agents by Pseudomonas Aeruginosa6-8. In these setting, there has been a boost during recent years of the development of antimicrobial stewardship programs (ASPs), with the aim to optimize and reduce the use of antimicrobial agents; these programs appear as a tool with potential impact in order to reduce or restrict the development of resistances to said agents9-11. However, there are still a limited number of studies published about this type of programs on haematological patients. The purpose of this study is to assess the clinical impact of an ASP on the clinical evolution of haematological patients admitted in a Critical Patient Unit.
MethodsThe design of the study was quasi-experimental and pre-post intervention. The ICU where the program was implemented is a medical ICU with 24 beds, in a tertiary hospital with 961 beds, which receives 1735 admissions per year as average, during the 2013-2015 period. This study included all those patients with haematological disease who were admitted to the Critical Patient Unit from October, 2013 to September, 2016.
Work Methodology of the ASPOn October, 2013, an ASP program was implemented in the unit. Summing up, the ASP team is formed by an Intensive Care Specialist with expertise in infection management in critical patients, and a Clinical Pharmacist, supported by a Microbiologist. They assessed three times per week all patients on antibiotic treatment in the unit. In case they found any incidence in prescription, there was a face-to-face intervention with the prescriptor (prospective audit)12, and there was follow-up of the evolution of the patient involved after the modification by consensus.
The following data were collected from patients included in the study: demo-graphical details, underlying haematological condition, cause of admission to the unit, severity scale at admission (APACHE II), as well as the need for vasoactive agents. For those patients who were admitted due to infection, or who developed infection during admission, the infectious agent responsible was also recorded.
In order to analyze the impact of the program on the clinical evolution of hae-matological patients in the unit, there was a comparison of mortality within the ICU, days of stay in the unit, the percentage of re-admissions within 30 days after discharge from the unit, as well as the number of days on mechanical ventilation in intubated patients, between the period before the intervention (from October, 2012 and September, 2013), and the intervention period (from October, 2013 to September, 2016).
Additionally, in those patients for whom an intervention was conducted, there was an evaluation of the number of relapses of the infectious condition after the intervention. A relapse of the infectious condition was described as the new presentation of the infectious episode that required the re-introduction of the antimicrobial agent withdrawn, or the modification of the dosing regimen after the intervention by the ASP, within 72 hours after said intervention. In order to determine the impact of the program on the colonization and infection by multi-resistant bacteria (MRB), there was an assessment of the evolution of the number of patients with new MRB colonization during their stay at the unit (defined as the presence of a new MRB after > 48 hours of stay in the unit), as well as the number of hospital infections caused by these during the same period. There was an analysis of epidemiological surveillance twice a week, in order to detect MRB colonization, through rectal and oropharyngeal cultures, and bronchial aspiration culture for intubated patients. At the same time, there was a record of the use of antimicrobial agents in the unit per year during the period of the study. The statistical analysis was conducted through the Stata v.13.0 program. Comparison of variables between the pre and post intervention groups was performed through parametric tests (Fischer, Student’s t) or non-parametric tests (χ2, Mann-Whitney’s U), according to the normality analysis of the sample. Mortality at 30 days of admission in the unit was analyzed with Cox Regression.
The study was approved by the Hospital Ethics Committee.
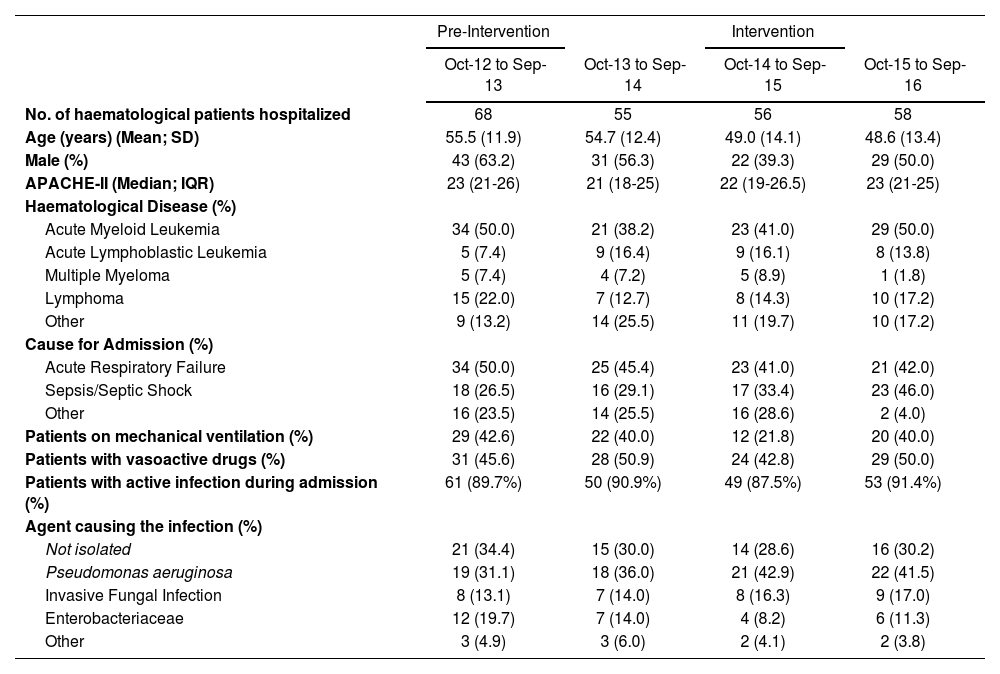
ResultsDuring the period of the study, the ASP team evaluated 324 antimicrobial agents in 169 haematological patients. The characteristics of the patients reviewed are defined in Table 1.
Characteristics of haematological patients hospitalized in the unit
| Pre-Intervention | Intervention | |||
|---|---|---|---|---|
| Oct-12 to Sep-13 | Oct-13 to Sep-14 | Oct-14 to Sep-15 | Oct-15 to Sep-16 | |
| No. of haematological patients hospitalized | 68 | 55 | 56 | 58 |
| Age (years) (Mean; SD) | 55.5 (11.9) | 54.7 (12.4) | 49.0 (14.1) | 48.6 (13.4) |
| Male (%) | 43 (63.2) | 31 (56.3) | 22 (39.3) | 29 (50.0) |
| APACHE-II (Median; IQR) | 23 (21-26) | 21 (18-25) | 22 (19-26.5) | 23 (21-25) |
| Haematological Disease (%) | ||||
| Acute Myeloid Leukemia | 34 (50.0) | 21 (38.2) | 23 (41.0) | 29 (50.0) |
| Acute Lymphoblastic Leukemia | 5 (7.4) | 9 (16.4) | 9 (16.1) | 8 (13.8) |
| Multiple Myeloma | 5 (7.4) | 4 (7.2) | 5 (8.9) | 1 (1.8) |
| Lymphoma | 15 (22.0) | 7 (12.7) | 8 (14.3) | 10 (17.2) |
| Other | 9 (13.2) | 14 (25.5) | 11 (19.7) | 10 (17.2) |
| Cause for Admission (%) | ||||
| Acute Respiratory Failure | 34 (50.0) | 25 (45.4) | 23 (41.0) | 21 (42.0) |
| Sepsis/Septic Shock | 18 (26.5) | 16 (29.1) | 17 (33.4) | 23 (46.0) |
| Other | 16 (23.5) | 14 (25.5) | 16 (28.6) | 2 (4.0) |
| Patients on mechanical ventilation (%) | 29 (42.6) | 22 (40.0) | 12 (21.8) | 20 (40.0) |
| Patients with vasoactive drugs (%) | 31 (45.6) | 28 (50.9) | 24 (42.8) | 29 (50.0) |
| Patients with active infection during admission (%) | 61 (89.7%) | 50 (90.9%) | 49 (87.5%) | 53 (91.4%) |
| Agent causing the infection (%) | ||||
| Not isolated | 21 (34.4) | 15 (30.0) | 14 (28.6) | 16 (30.2) |
| Pseudomonas aeruginosa | 19 (31.1) | 18 (36.0) | 21 (42.9) | 22 (41.5) |
| Invasive Fungal Infection | 8 (13.1) | 7 (14.0) | 8 (16.3) | 9 (17.0) |
| Enterobacteriaceae | 12 (19.7) | 7 (14.0) | 4 (8.2) | 6 (11.3) |
| Other | 3 (4.9) | 3 (6.0) | 2 (4.1) | 2 (3.8) |
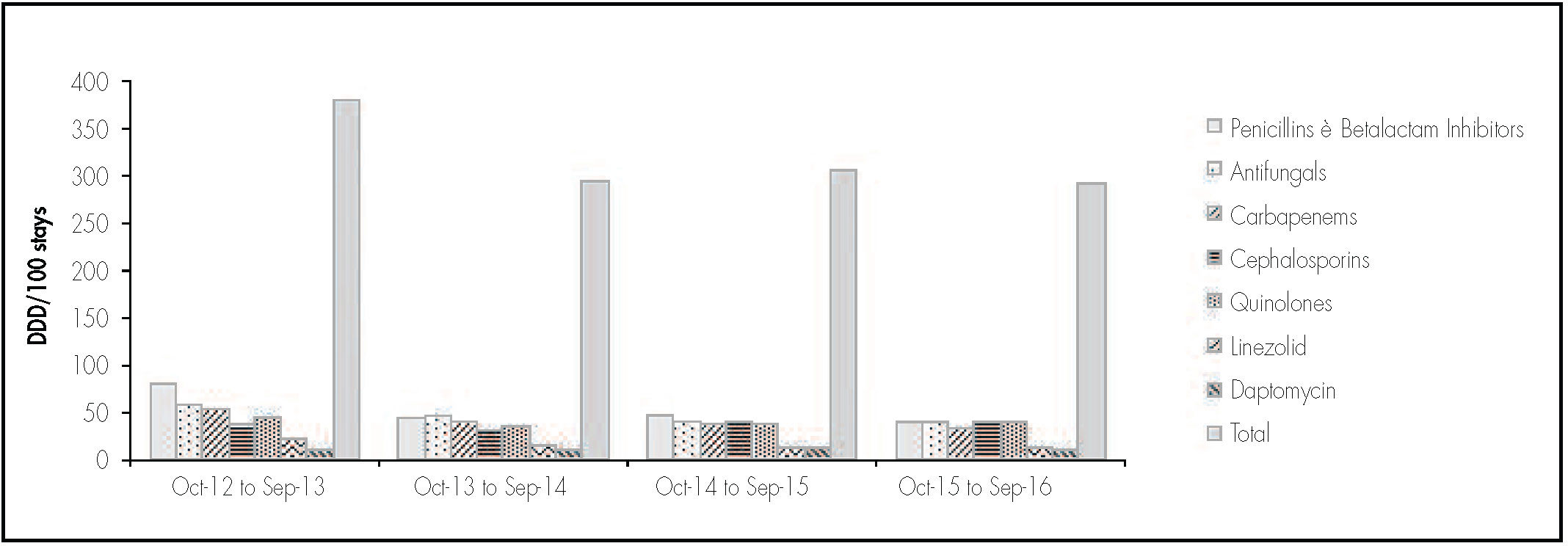
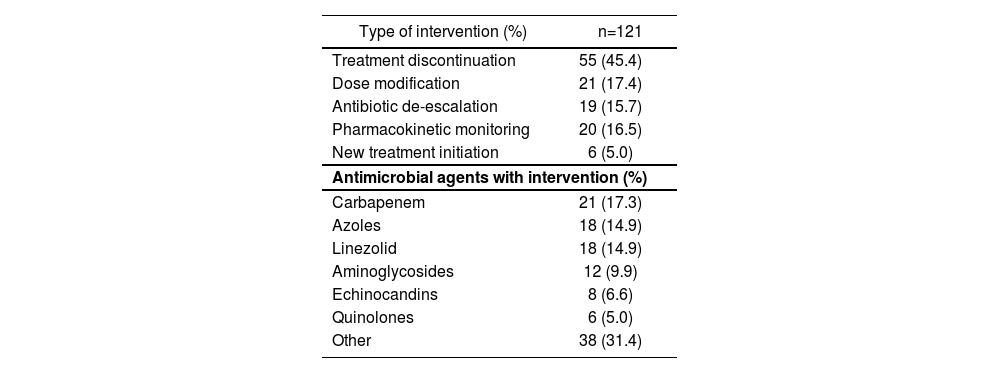
After treatment review, there were 121 treatment modifications. The recommendations by the ASP team appear in Table 2. The majority of recommendations (82.6%) were accepted by the physicians in charge. A relapse in the infectious condition was only observed in three patients (2.5%) after the proposed withdrawal of the antimicrobial agent, and treatment had to be re-initiated. The evolution in the use of antimicrobial agents after the ASP implementation in the unit appears in figure 1.
Interventions by the ASP.
| Type of intervention (%) | n=121 |
|---|---|
| Treatment discontinuation | 55 (45.4) |
| Dose modification | 21 (17.4) |
| Antibiotic de-escalation | 19 (15.7) |
| Pharmacokinetic monitoring | 20 (16.5) |
| New treatment initiation | 6 (5.0) |
| Antimicrobial agents with intervention (%) | |
| Carbapenem | 21 (17.3) |
| Azoles | 18 (14.9) |
| Linezolid | 18 (14.9) |
| Aminoglycosides | 12 (9.9) |
| Echinocandins | 8 (6.6) |
| Quinolones | 6 (5.0) |
| Other | 38 (31.4) |
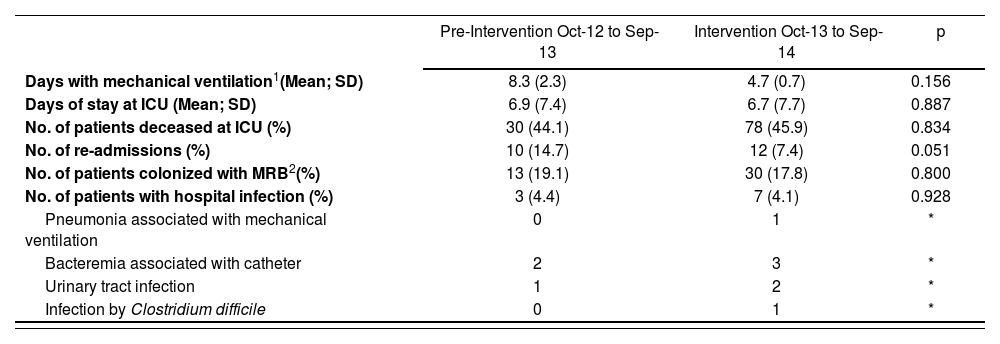
The clinical evolution of patients during the pre and post-intervention periods appears in Table 3. No significant differences were observed in terms of mean stay, mortality within ICU, or the proportion of haematological patients re-admitted to the unit. Likewise, no significant reduction was observed in mortality at 30 days of admission during the intervention period (HR: 0.893; p = 0.669). There were no differences in the duration of mechanical ventilation for intubated haematological patients.
Impact of the ASP program on clinical results of patients.
| Pre-Intervention Oct-12 to Sep-13 | Intervention Oct-13 to Sep-14 | p | |
|---|---|---|---|
| Days with mechanical ventilation1(Mean; SD) | 8.3 (2.3) | 4.7 (0.7) | 0.156 |
| Days of stay at ICU (Mean; SD) | 6.9 (7.4) | 6.7 (7.7) | 0.887 |
| No. of patients deceased at ICU (%) | 30 (44.1) | 78 (45.9) | 0.834 |
| No. of re-admissions (%) | 10 (14.7) | 12 (7.4) | 0.051 |
| No. of patients colonized with MRB2(%) | 13 (19.1) | 30 (17.8) | 0.800 |
| No. of patients with hospital infection (%) | 3 (4.4) | 7 (4.1) | 0.928 |
| Pneumonia associated with mechanical ventilation | 0 | 1 | * |
| Bacteremia associated with catheter | 2 | 3 | * |
| Urinary tract infection | 1 | 2 | * |
| Infection by Clostridium difficile | 0 | 1 | * |
Regarding the period before the intervention, we did not observe a significant reduction in the percentage of new MRB colonizations during their stay at the unit. There were no significant differences between both periods in the number of hospital infections in this group of patients.
DiscussionThe results of this study show that the implementation of an ASP based on prospective audit in a critical patient unit will entail a relevant number of interventions on antimicrobial prescription, including a major number of treatment discontinuations, without representing a negative impact on the clinical evolution of haematological patients in the unit. Infection management in haematological patients represents one of the great challenges for Intensive Care Specialists. The impact of an adequate selection of antimicrobial agent on the survival of these patients, as well as the high percentage of episodes without microbiological isolation, lead to the usual practice of prescribing broad spectrum antimicrobial agents for this group of patients13. However, there will often be a lack of coincidence between treatment selection or duration and the clinical evidence available, and this will favour an increase in the risk of toxicity, costs, and MRB selection.
It is widely known that the use of antimicrobial agents entails an increase in the selection and infection by multi-resistant strains14-16. In haematological patients, the need for a frequent use of antimicrobial agents has led to an alarming increase in resistance to these agents, particularly for Gram negative bacteria8. In fact, various authors have linked the infection by multi-resistant strains with bad prognosis for these patients17,18. Similarly to other published experiences about the implementation of ASP programs in Critical Care Units19-22, the most frequent intervention was the discontinuation of antimicrobial agents prescribed empirically. In patients with neutropenia, the potential infection by multi-resistant strains, as well as the difficulty to identify the germ causing said infection, will often lead to the use of broad-spectrum antimicrobial coverage, often during prolonged periods of time. In these patients, it is very important to discontinue treatment once the germ causing the infection has been identified, as well as when they have recovered from neutropenia, in order to prevent the selection and colonization by multi-resistant strains.
On the other hand, it is worth highlighting the work conducted in terms of dose adjustment and pharmacokinetic monitoring of antimicrobial agents. It has been demonstrated that the optimization of the pk/pD parameters will be a key factor in order to ensure an adequate exposure to antimicrobial agents, thus reducing the possibility of therapeutic failure, resistance development, and presence of adverse effects associated with the treatment23. In this study, it has not been observed that the introduction of an ASP in the unit led to a reduction in the number of patients colonized by MRB. The implementation of this type of programs represents a significant reduction in the use of antimicrobial agents, and this could have a significant impact on the pressure of colonization by MRB and other opportunistic pathogens24,25. However, it must be considered that the transmission of MRB between patients through healthcare professionals represents the main source of colonization in patients admitted to Critical Care Units26. Not being able to identify which patients presented colonization by transmission is a limitation in this study. Regardless of this, various authors have associated the implementation of these programs with a lower incidence of colonization by MRB27. Given the existing link between colonization and infection in Critical Care Units14,16, we consider that this type of programs, in coordination with programs for prevention of hospital infection, will be essential in order to minimize the incidence of infections by multi-resistant strains. On the other hand, the limited number of hospital infection cases in this group of patients has prevented us from assessing the impact of the program on the incidence of hospital infection. It will be necessary to conduct comparative studies with a higher number of patients, in order to evaluate this hypothesis adequately.
It is worth highlighting that, unlike what has been published for other groups of patients9,28 the implementation of the ASP program has not represented a reduction in mean stay or mortality. So far, there have been few studies analyzing the impact of this type of programs on the clinical evolution of critical patients. Elliggsen and cols29, in their prospective study with 1-year intervention, observed that the implementation of an ASP program focused on specific antimicrobial groups achieved a reduction in their use, as well as the incidence of infection by C difficile, but there was no reduction in hospital stay or mortality. Taggart and cols30 also described the impact of an ASP program in a medical-surgical ICU. After one year of intervention, they did not observe significant reductions in mean stay and mortality. In this study, the authors reached the conclusion that studies with longer duration are necessary in order to assess the impact of the ASP on clinical evolution and resistances.
On the other hand, the haematological patient admitted to ICU presents a high complexity management, and their prognosis depends to a high extent on the fast intervention by specialists31; therefore, it will be difficult for this type of programs to have any effect on the clinical evolution of this group of patients at short term. However, we have observed a trend towards the reduction in the number of re-admissions to the unit since the program was implemented, and this leads us to think that an adequate selection and dose adjustment of treatment could have a positive impact on their evolution at mid-long term.
This study presents certain limitations. First of all, the results of the pre and post-intervention analysis could be influenced by other factors besides the intervention, which could modify the evolution of the patients in the unit, including changes in admission criteria, implementation of new programs for hospital infection control, or modifications in treatment protocols. Throughout the intervention period, various strategies have been set up with the objective of reducing the spread of MRB, including programs of active surveillance for handwashing, the incorporation of chlorhexidine to patients’ daily hygiene, as well as the use of silver-ion impregnated parabens. However, none of these strategies has demonstrated any clinical impact on patients in our unit, beyond a reduction in the incidence of MRB colonization. The measures included in the Bacteremia Zero and Pneumonia Zero programs32 have demonstrated a positive impact on patients admitted to Spanish ICUs. However, these measures had been implemented in the unit before the period of the study. It is worth highlighting that in our unit, no significant changes have been conducted during the period of intervention in terms of admission criteria or protocols for infection treatment in this type of patients; we have not found any significant changes in the severity criteria of haematological patients admitted to the unit. On the other hand, slight variations have been found regarding the type of underlying haematological disease in patients admitted to our unit. However, as previously discussed, the prognosis of haematological patients admitted to a Critical Care Unit will depend to a high extent on a fast and adequate clinical intervention30, beyond the haematological disease itself.
Summing up, the intervention of an ASP on critical haematological patients will achieve an optimization in antimicrobial treatment, without any negative consequences on patient evolution; it appears as a very valuable tool in order to reduce the selection of multi-resistant strains.