Describe the phases of implementation, scaling and integration of a pharmacy teleconsultation model in electronic history, to coordinate the care transition of patients.
MethodDescriptive and retrospective study in a health area of 500,000 inhabitants (3 years). In the first phase, a working group was created, a communication platform was designed and a continuity program was piloted between a hospital pharmacist and the 13 primary care pharmacists. The objective was to solve problems related to medications (especially those of sanitary approval) in polymedicated patients hospitalized in the Short Stay Unit-Emergency. In a second phase, the program included all the patients in any unit and all the pharmacists in the hospital. In the third phase, the program was extended to the teleconsultation format within the corporate information systems of the Health Service. Quantitative descriptive variables were recorded (number, motives and resolution of the teleconsultations).
ResultsIn total, more than 470 consultations were registered (118 in the first phase, 158 in the second and 194 in the third), which were resolved in 90% of the cases. The main reasons were discrepancies in type approval drugs, prescribed in the care transition and nutritional assessment.
ConclusionsTeleconsultation allows the coordination of pharmaceutical care between levels, quickly and easily. Increase the visibility and access of professionals. Problems are resolved without displacements or time delays for patients.
Describir las etapas de implantación, escalado e integración de un modelo de teleconsulta de Farmacia en la historia electrónica, para coordinar la transición asistencial de los pacientes.
MétodoEstudio descriptivo y retrospectivo en un área sanitaria de 500.000 habitantes (3 años). En la primera fase se creó un grupo de trabajo, se diseñó una plataforma de comunicación y se pilotó un programa de continuidad entre un farmacéutico de hospital y los 13 de atención primaria. El objetivo fue resolver problemas con medicamentos (especialmente los de homologación sanitaria) en pacientes polimedicados hospitalizados en la Unidad de Corta Estancia-Urgencias. En una segunda fase, el programa incluyó a todos los pacientes de cualquier unidad y a todos los farmacéuticos del hospital. En la tercera fase, se escaló el programa al formato de teleconsulta dentro de los sistemas de información corporativos del Servicio de Salud. Se registraron variables descriptivas cuantitativas (número, motivos y resolución de las teleconsultas).
ResultadosEn total, se registraron más de 470 consultas (118 en la primera fase, 158 en la segunda y 194 en la tercera), que fueron resueltas en el 90% de los casos. Los principales motivos fueron problemas con medicamentos de homologación, con medicamentos prescritos en la transición asistencial y con nutrición artificial domiciliaria.
ConclusionesLa teleconsulta permite coordinar la atención farmacéutica entre niveles de manera rápida y sencilla. Aumenta la visibilidad y el acceso de los profesionales, resolviendo los problemas sin desplazamientos ni demoras de tiempo para los pacientes.
For a long time, all the National Health System services were divided into two levels: Primary Care (PC) and Hospital Care (HC), which developed in parallel with each other. The coordination between both levels of care is the current priority for health services, organizations, and European Development programs1–3.
Life expectancy in Spain exceeds 80-years of age, with an expected increase by two years for 2020 in Europe. The economic development and advances in medicine are changing the expectations in conditions such as cardiovascular or cancer. All this is creating a new epidemiological pattern, characterized by ageing and chronicity, which generates an increasing healthcare demand4.
The European Union is developing a strategic line of priority research on “Active and Healthy Ageing”, which intends to address such important problems as polypharmacy and comorbidity5. Chronicity is another essential line of research, as shown by the investment in the HORIZONTE 2020 projects, targeted to the optimization in health care plans and pharmacotherapy6.
Addressing polypharmacy in chronic patients is one of the main challenges. Different studies show that a high number of drug-related adverse events can be avoided, and these problems can lead to hospitalizations or prolonged hospital stays7,8. In different autonomous communities, strategies such as Polymedicated Patient Programs have been implemented, in order to optimize and simplify the drug therapy for chronic patients, given that these are the most vulnerable during transitions of care9.
The creation of healthcare structures with integrated management and technological development (electronic prescription, electronic patient record, etc.) have laid the foundations for building a cross-sectional healthcare model focused on patients; this has been moving forward with tools for remote patient monitoring or teleconsultation between professionals.
Teleconsultation (or e-consultation) is an emergent Information and Telecommunications Technology (ITT) tool which allows synchronous electronic communication between professionals (typically from PC to HC) on general or patient-specific matters. E-mail is the most basic form of e-consultation, though web platforms or computer applications have been developed, which combine the shared electronic medical record and instant messaging. Different medical specialties (Dermatology, Rheumatology or Cardiology) have been pioneers in the use of the most advanced teleconsultation models, integrating them in their daily practice, and in the performance indicators for the healthcare managers in their centers. However, there are limited experiences showing a similar development between Hospital Pharmacy and Primary Care10.
The main objective of this study is to describe the stages for the implementation and escalation of a Hospital Pharmacy teleconsultation (or e-consultation) model between professionals, from its most basic form to its development integrated within the electronic clinical record of the patient.
MethodsThe teleconsultation project in Pharmacy was developed in a healthcare area managing > 500,000 inhabitants. This healthcare area is structured with integrated management, with a common management team for HC and PC. It includes 52 PC centers, a chronic psychiatric center, two hospitals (with 1,275 beds in total), and > 1,500 beds in social and health care centers with agreement with the hospital regarding pharmaceutical care. There are 23 Hospital Pharmacists and 13 Primary Care Pharmacists in charge of pharmaceutical management and care in all these centers.
The Health System has a single and joint electronic clinical record for HC-PC, electronic prescription and, since 2012, there is enough support for the development of teleconsultation (between professionals or with patients), and telemonitoring at patient homes.
The creation of Pharmacy Teleconsultation between professionals was initiated by mid-2014 and developed in three stages, differentiated by the level of development of the electronic tool used and the professionals involved.
Stage I: Creating the Pharmacy teleconsultation (e-consultation) modelThe first steps consisted in the formalization of the model, the analysis of the coordination process between PC and HC Pharmacists, as well as the study of the electronic media available for conducting it.
A board of experts was involved in this stage, and a work team was created with Pharmacists from both levels of care and the person responsible for quality, in order to standardize and reach a consensus about the reasons for consultation, patient coding, and the types of problems to be referred to either direction.
In this stage, an on-line bidirectional referral platform was developed (through e-mail) for communication between both levels. Activity record was also developed through a corporate program, accessible and common for both levels (but not integrated into the electronic clinical record). A 12-month pilot program was designed, coordinated by a Pharmacy Specialist working part-time3 (in order to prepare / validate the computer tool together with the Information Systems Unit, and to manage preliminary results). The 13 Primary Care Pharmacists from the healthcare area involved participated in this pilot program.
The target population for this pilot was:
- •
Patients with DRPs with medications subject to sanitary approval (“visado”) for treatments prescribed by specialists (referral from PC to HC), because in this healthcare area, PC Pharmacists are mostly in charge of the “visado” procedure.
- •
Patients with DRPs detected during drug reconciliation at admission or discharge from the Emergency Unit and the Short-Stay Unit, or those detected in the outpatient unit of the Hospital Pharmacy, for their inclusion in the PC Polymedicated Program (referral from HC to PC)9.
In this stage (12 months), patient referral was standardized and extended:
- •
From PC to HC: Patients with doubts or DRPs with medications for hospital use or prescribed by hospital specialists, and therefore the activity was extended with the involvement of all Hospital Pharmacists, represented in each specialization area from the Hospital Pharmacy Unit.
- •
From HC to PC: Patients with DRPs detected during drug reconciliation at admission or discharge from any unit or the outpatient unit.
The base operating program for consultations was automated and individualized by Pharmacist and area or health center. A code was assigned to each HC and PC Pharmacist; therefore, consultations were received only by those Pharmacists involved (according to the reason for consultation), instead of being a general message to the unit.
Stage III: Escalation and integration of the Pharmacy teleconsultation within the electronic clinical record
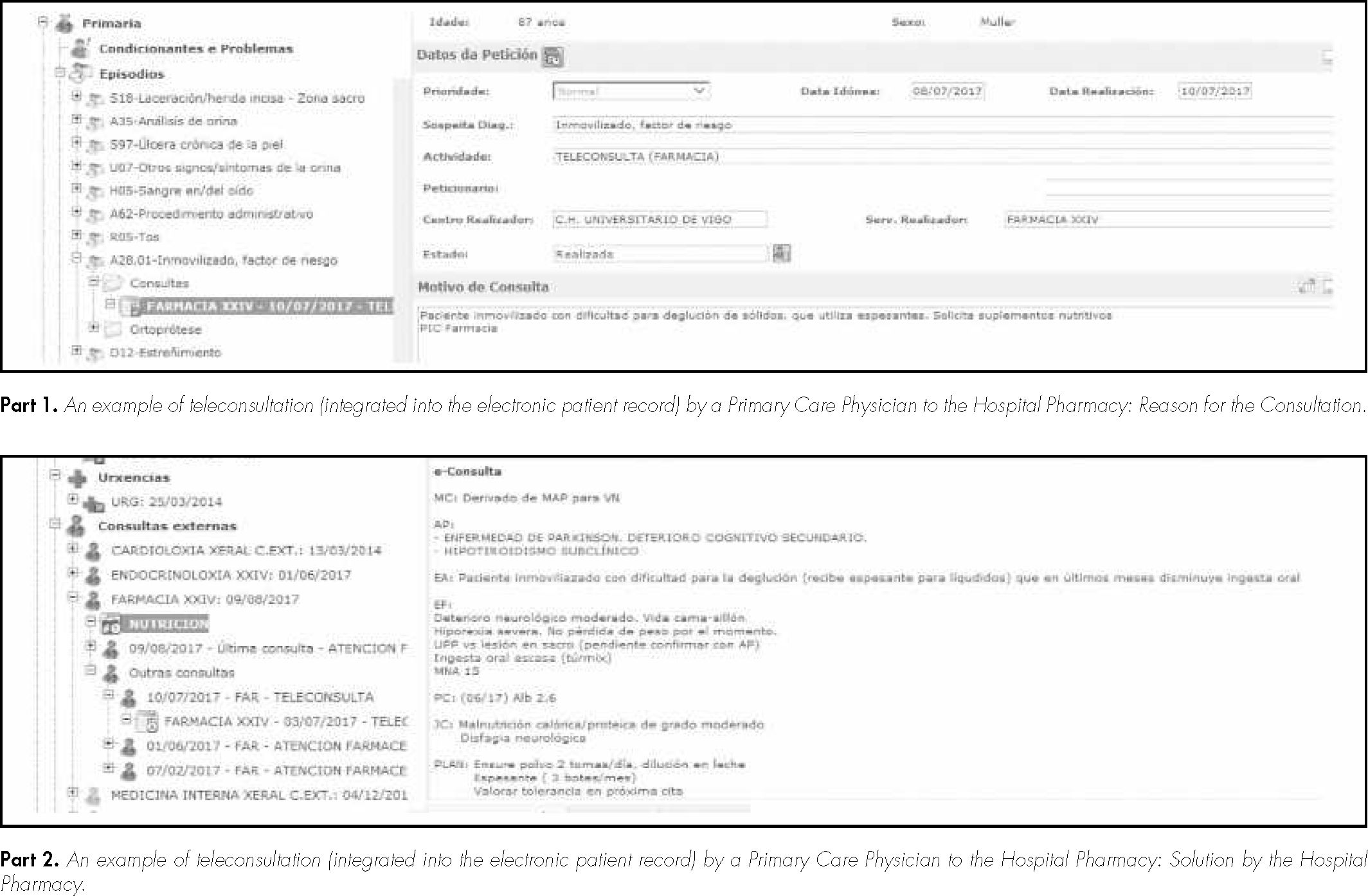
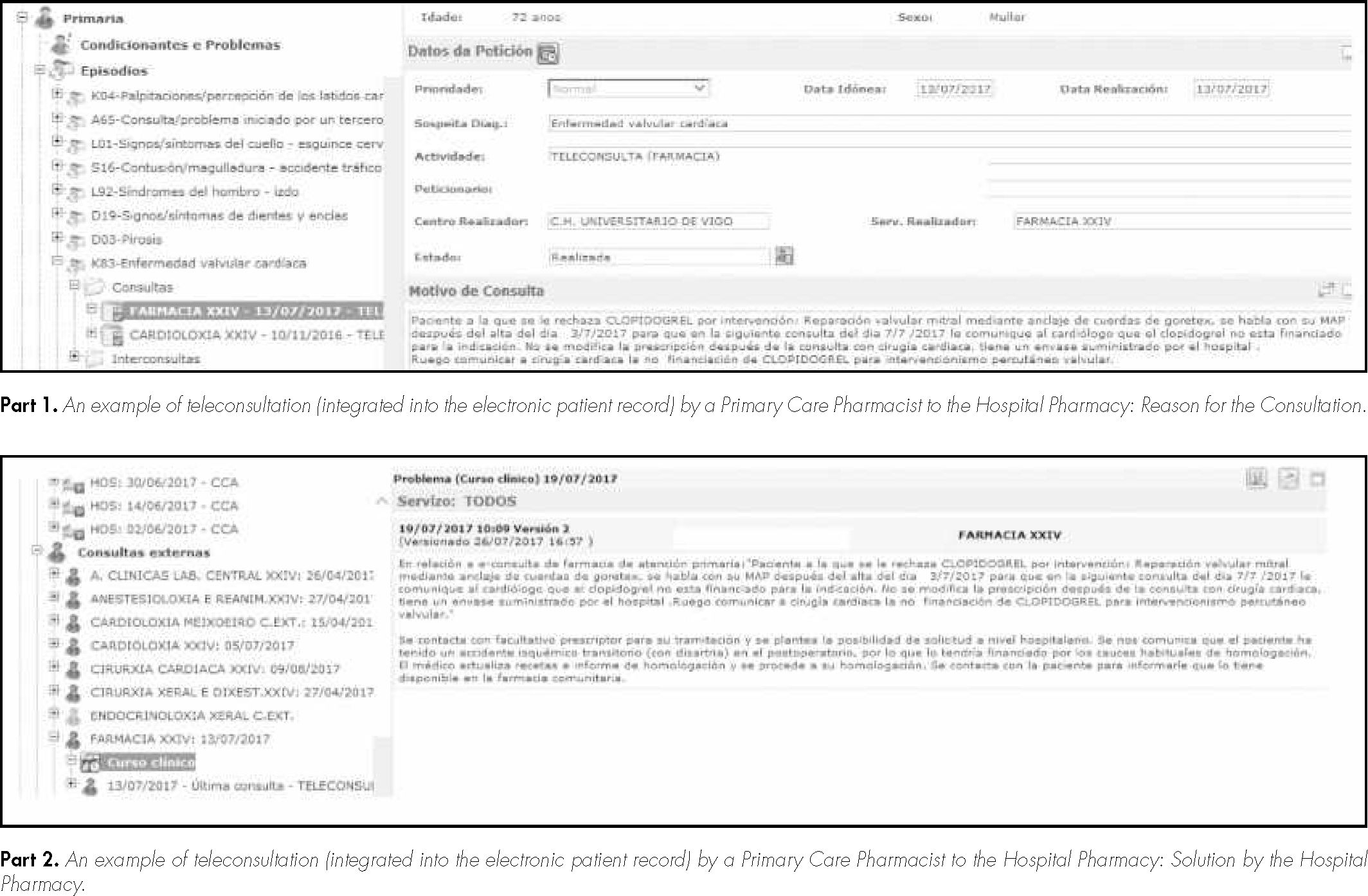
The e-consultation was escalated and integrated into the electronic record for referrals from PC to HC. For this, the Health Service was requested authorization by mid-2016, in order to have access to the technological infrastructure required. Following this, a team work was created with members of the management, admissions, and PC-HC Pharmacists, in order to implement the work system of the program using ICTs, the Electronic Clinical Record (IANUS) and the System for Managing Appointments in Primary Care (SIGAP).
Moreover, there was an increase in the number of professionals involved in the circuit: PC physicians in order to refer or consult doubts or problems with patients on artificial home nutrition.
In this new channel, e-consultation is conducted by the PC professional through the clinical patient record (which is shared by both settings of care), associated to an episode “A-47: Remote telemedicine consultation (FAR-FARMACIA)”. And an outpatient consultation agenda was created in HC: Telefarmacia G00 (remote appointment).
A Hospital Pharmacist is responsible each day for examining the teleconsultation patients in a specific work agenda, in order to evaluate and solve the problems put forward, or refer them to the Pharmacist of Reference according to the specialization area (Oncohematology, Nutrition, Cardiovascular, Infectious Diseases, Drug Monitoring, Psychiatry, Information on Medication, Pediatrics, and others). Once solved, the answer to the teleconsultation is entered in the electronic record, creating a specific clinical course. This evaluation is then reviewed by the PC professional, four days after the automatic generation of the consultation, because at the time of its creation, a remote appointment is also generated in PC for the subsequent examination of the patient.
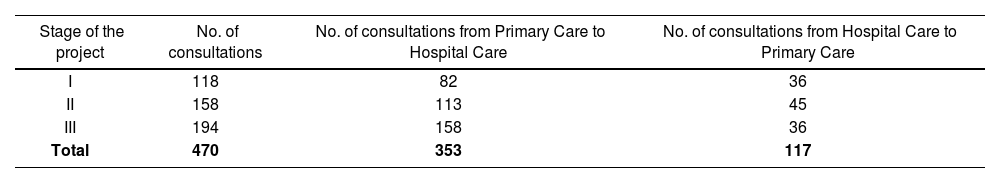
ResultsIn total, 470 consultations were registered in the three stages of the study; 353 of them were conducted from PC to HC (see Table 1).
Number of consultations conducted in the healthcare coordination model for the Pharmacy Unit at each stage of the Project
| Stage of the project | No. of consultations | No. of consultations from Primary Care to Hospital Care | No. of consultations from Hospital Care to Primary Care |
|---|---|---|---|
| I | 118 | 82 | 36 |
| II | 158 | 113 | 45 |
| III | 194 | 158 | 36 |
| Total | 470 | 353 | 117 |
The reasons for consultation were: to solve problems associated with medications with sanitary approval (32.8%), evaluations of artificial home nutrition (20.6%), patient inclusion in the Primary Care Polymedicated Program (18.2%), information about medications (off-label use, depot antipsychotics, cytostatic agents, etc.) (10%), inadequate dosing (9.8%), drug duplications (6.4%), and others (2.2%).
Consultations were solved in > 90% of cases. With teleconsultation, the average time to response was < 48 hours (with 4 hours as minimum and 144 hours as maximum); and approximately 40% of patients were referred for a second personal consultation in the Hospital Pharmacy in order to obtain home nutritional support or medications used off-label.
The visualization of teleconsultation is shown in figures 1 and 2.
DiscussionThe benefits of e-consultation have been widely described, both for patients and professionals. For patients, it represents an improvement in access in terms of time and space, as well as regarding the communication and information received. In terms of professionals, it improves the communication between levels, and this translates into a higher quality of care and patient safety11.
The innovation of this article lies in the description of how to start a Pharmacy Continuity Program, and how to create and implement a Pharmacy Teleconsultation at the same level than the other medical specialties. This leads to positioning this activity (internally for the Pharmacy Unit and externally for managers and patients) as a highly problem-solving process that can provide visibility, safety, and savings in costs and time.
Regarding the results achieved, we can observe that the number of consultations has increased since the start of the program, and mostly with the incorporation of Primary Care Physicians to the circuit. However, we consider that these data will increase as the new communication tool gets established, and higher electronic involvement of professionals is encouraged.
Publications about care coordination experiences are frequent among medical specialties. Thus, in 1996 Friedman et al. had already published a study on telemedicine to monitor blood pressure and treatment adherence among patients with hypertension12. Another example is the publication in 2010 by Eron et al. for the follow-up of infections at hospital discharge13. And there is a more recent telemedicine experience published, targeted to improving treatment adherence in schizophrenic patients14.
There are limited experiences described in Pharmacy, and the majority present descriptive results which are difficult to compare from a quantitative point of view; however, there are comparable data regarding the main reasons for consultation (the need for follow-up and healthcare approval)10.
The incorporation of teleconsultation between PC and medical specialties is a healthcare activity conducted habitually in the corporative information systems of many Regional Health Ministries for different autonomous communities, such as Galicia, Andalucía, etc.11. However, this is an unresolved matter for Pharmacy Units; so far we have presented the first coordination program to achieve an e-consultation with the same visibility than any other specialty. But this has some limitations, because so far computer tools have allowed to develop and integrate into the electronic record the referral of patients in one direction (from PC to HC), and it has been necessary to use other communication platforms (collaborative websites, etc.) in order to do it in the other direction10. It is also necessary to extend the period of analysis in order to achieve a higher volume of results that show that this activity offers health outcomes that can be measured, which will allow to strengthen and encourage the use of this type of strategies. In this sense, we intend to extend the study and go deeper into the objectives of efficiency and patient satisfaction.
However, the study presented here represents a chance for improvement in coordination of care in any healthcare area with electronic record and prescription, thus giving an answer to the suggestions published in other studies associated with the follow-up of chronic patients with multiple conditions15.
As a conclusion, teleconsultation allows to coordinate pharmaceutical care between levels, in a fast and simple manner, it increases the visibility and access for professionals, and any discrepancies can be solved without travels or time delays for patients; therefore, it would be expected to have a reduction in expenses and an improvement in the perception of healthcare quality by the users.
FundingNo funding.
AcknowledgementsTo all professionals from Primary Care, Pharmacy, Admissions, Quality and Management of the EOXI Vigo who are actively involved in the Pharmacy Teleconsultation program.
Conflict of interestsNo conflict of interests.
Presentation in CongressesThis study has been presented at the 61st National Congress of the Spanish Society of Hospital Pharmacy, within the round table “Humanizing Pharmacy Services”, on October 20th, 2017.
Contribution to scientific literature.
Coordination between levels of care is a priority activity that must be improved in different healthcare systems. The Hospital Pharmacy Unit staff has understood that we play an essential role in terms of ensuring the continuity of care for our chronic patients; for this aim, we can use different tools based on telemedicine. This article shows how any Hospital Pharmacy Unit can develop a teleconsultation system that will allow the coordination of care for pharmacotherapy, from a basic form to that integrated within the electronic record of the patient, at the same level as any medical specialty.
Marisol Samartín-Ucha1, Isabel Rey-Goméz-Serranillos2, Alicia Martín-Vila3, Susana San-Martín-Álvarez1, Yaiza Romero-Ventosa1, Noemí Martínez-López-de-Castro4, Nuria Iglesias-Álvarez5, Carmen Gallastegui-Otero1, Cristina Vázquez-López1, Natividad Lago-Rivero1, David Rodríguez-Lorenzo6, Elena Lorenzo-Llauger7, Julio García-Comesaña8, Guadalupe Piñeiro-Corrales9
1Area Specialist. Pharmacy Unit. Xerencia de Xestión Integrada of Vigo (SERGAS), Vigo. Spain. 2Primary Care Pharmacy Coordinator. Xerencia de Xestión Integrada of Vigo (SERGAS), Vigo. Spain. 3Pharmacy Unit Research Technician. Xerencia de Xestión Integrada of Vigo (SERGAS), Vigo. Spain. 4Head of Department and Coordinator of the Hospital Pharmacy Outpatient Consultations. Pharmacy Unit. Xerencia de Xestión Integrada of Vigo (SERGAS), Vigo. Spain. 5Primary Care Pharmacist. Xerencia de Xestión Integrada of Vigo (SERGAS), Vigo. Spain. 6Innovation and Quality Coordinator. Xerencia de Xestión Integrada of Vigo (SERGAS), Vigo. Spain. 7Head of Procedures without Admission and Emergencies. Xerencia de Xestión Integrada of Vigo (SERGAS), Vigo. Spain. 8Manager of Care Procedures. Xerencia de Xestión Integrada of Vigo (SERGAS), Vigo. Spain. 9Head of Department. Pharmacy Unit. Xerencia de Xestión Integrada of Vigo (SERGAS), Vigo. Spain.