Hospital Pharmacy Service (HPS) in Spain have been impacted by the health crisis caused by the COVID-19 pandemic. Thus, the outbreak has forced HPSs to adapt their outpatient consultation services to Telepharmacy to optimize clinical outcomes and reduce the contagion risk. The purpose of this article is to describe and analyze the experience of HPSs with hospital outpatient through Telepharmacy during the COVID-19 pandemic and expose the learned lessons. Measures have been adopted in on-site outpatient pharmacy clinics to prevent patients and professionals to virus exposure. These measures are based on national and international recommendations on social distancing and hygiene. With regard to remote outpatient pharmacy services, teleconsultation with drug dispensing has been promoted based on five basic procedures, each with its advantages and limitations: home drug delivery from HPSs, with the advantage of universal access and the limitation of entailing a substantial investment in resources; HPS coordination with primary care pharmacists, which requires no investments but with limited access to some geographic areas; HPS coordination with community pharmacists based on a large network of pharmacies, which requires the patient to go to the pharmacy, without confidentiality being guaranteed for any patient; geolocation and hospital-based medication dispensing, which provides universal access and direct traceability, but entails investment in human resources; and HPS coordination with associations of patients, which does not entail any additional cost but limits the information available on the diseases of society members. Three main lessons have been learned during the pandemic: the satisfactory capacity of HPSs to provide outpatient pharmacy consultation services in the setting of a public health crisis; the usefulness of Telepharmacy for the clinical follow-up, healthcare coordination, outpatient counseling, and informed dispensing and delivery of medication (with a high level of satisfaction among patients); and the need to foster Telepharmacy as a complementary tool through a mixed model of outpatient pharmacy consultation service that incorporates the advantages of each procedure and adapts to the individual needs of each patient in a context of humanized healthcare.
Los servicios de farmacia hospitalaria (SFH) en España se han visto afectados por la crisis sanitaria provocada por SARS-CoV-2 y han tenido que adoptar sus procedimientos de atención farmacéutica (AF) al paciente externo (PE) mediante estrategias de Telefarmacia, con los objetivos de maximizar los resultados en salud y reducir el riesgo de contagio. El objetivo de ese artículo es describir y analizar los procedimientos AFPE durante la pandemia SARS-CoV-2 y comunicar las lecciones aprendidas en los SFH. En relación con las consultas externas de AF presenciales, se han adoptado medidas para minimizar el contagio viral de pacientes y profesionales, siguiendo las recomendaciones nacionales e internacionales de referencia de distanciamiento temporal, espacial y recomendaciones higiénicas. En cuanto a las consultas externas de AF no presenciales, se han potenciado las teleconsultas con dispensación del tratamiento en base a cinco procedimientos básicos, cada uno de ellos con sus ventajas y limitaciones: dispensación domiciliaria desde SFH que presenta las ventajas de la universalidad de acceso, pero requiere una elevada inversión en recursos; coordinación del SHF con farmacéuticos de atención primaria, que conlleva una nula inversión en recursos, pero limita el acceso a determinadas zonas geográficas; coordinación del SFH con farmacéuticos comunitarios, que utiliza una amplia red de oficinas de farmacia, pero exige el desplazamiento del paciente sin garantías de confidencialidad para todos los casos; geolocalización y dispensación hospitalaria, que permite un acceso universal y trazabilidad directa, pero requiere un incremento en recursos humanos; y coordinación del SFH con asociaciones de pacientes, que no requiere inversión económica, pero limita el acceso a las patologías de los asociados. Destacamos finalmente tres lecciones aprendidas: la capacidad de AFPE de SFH españoles ante una crisis sanitaria; la utilidad de la Telefarmacia para el seguimiento clínico, la coordinación asistencial, información al PE, dispensación y entrega informada (con elevada satisfacción de los pacientes); y la necesidad de potenciar la Telefarmacia como herramienta complementaria, en un modelo mixto de AFPE que incorpore las ventajas de cada uno de los procedimientos adaptándose a las necesidades individuales de los pacientes en un entorno de humanización de la asistencia sanitaria.
Hospital pharmacy services (HPS) in Spain were affected by the health crisis caused by the SARS-CoV-21–7 and had to urgently adapt outpatient pharmaceutical care (PC) procedures to maximize health outcomes8,9 and reduce the contagion risk10. Although the population was allowed to visit the pharmacy to get their medicines, the new procedures developed based on Telepharmacy have made it possible to guarantee outpatient PC from HPS and avoid patient visits to the hospital.
Telepharmacy11–14, understood as the practice of pharmacy at a distance through the use of information and communication technologies (ICT) was incorporated by the Spanish Society of Hospital Pharmacy (SEFH) as a strategic line of care15–18 (more specifically, outpatient PC in the MAPEX Project19). Moreover, it has already been successfully evaluated at national level in terms of pharmacotherapy follow-up, coordination with the care team and in the informed remote dispensing or delivery of medicines20–27. In this line, the aim of this paper is to describe and analyze the Telepharmacy procedures in outpatient PC during the SARS-CoV-2 pandemic.
Developed strategy: procedures of outpatient pharmaceutical careThis article cannot include every procedure carried out with considerable effort and professionalism by all the HPSs in Spain in such exceptionally difficult circumstances28, but it is intended to provide a representative sample of the strategies adopted. A recent national survey on Telepharmacy conducted by the SEFH during the pandemic, which definitive results will be published in a forthcoming issue of the journal Farmacia Hospitalaria, shows that almost 120,000 outpatients in Spain from 185 hospitals have received PC through Telepharmacy, with a clear focus on humanization of PC services. The hospitals consulted in different Autonomous Communities implemented a model that is included in the procedures shown below.
Face-to-face outpatient pharmaceutical care consultationsSome outpatient PC consultations continued to be conducted face-to-face. To this end, measures were implemented to minimize viral infection of patients and professionals, following national and international reference recommendations9,29–31: temporary and spatial distancing, disinfection of the waiting room and consultation room, information posters on personal hygiene, and prevention of infection in the consultation rooms (e.g. screens, masks, etc.). There were no relevant changes in relation to face-to-face outpatient PC procedures in the past.
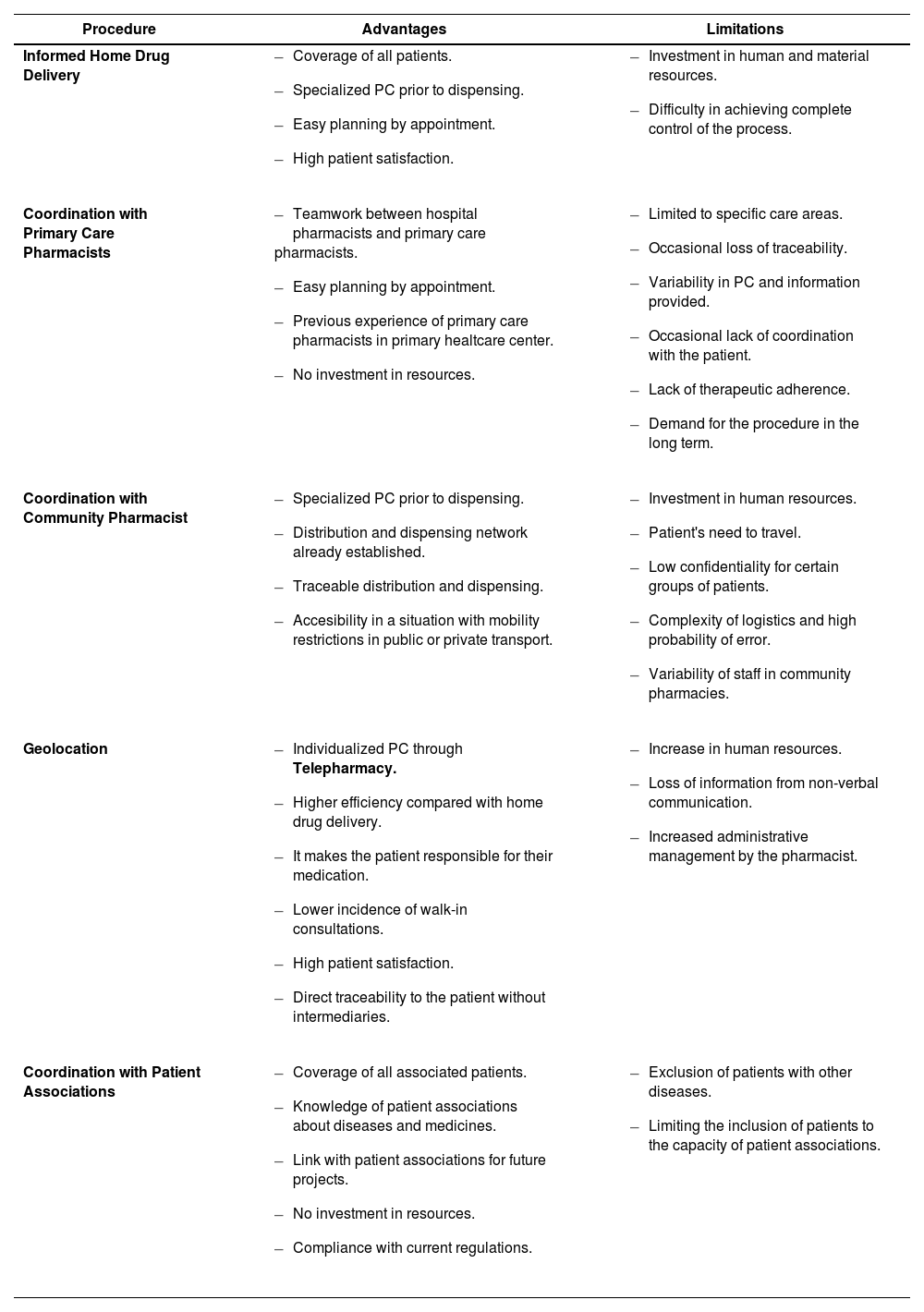
Off-site outpatient pharmaceutical care consultations. TelepharmacyHealth authorities issued exceptional instructions during the state of alert on the dispensing of medicines in HPSs32,33. As a result, and considering the previous legal framework, HPSs established outpatient PC procedures to guarantee therapeutic adherence and patient clincal monitoring. The main advantages and limitations of each procedure, according to their designers, are summarized in Table 1.
Advantages and limitations of Telepharmacy: dispensing and informed delivery procedures
| Procedure | Advantages | Limitations |
|---|---|---|
| Informed Home Drug Delivery |
|
|
| Coordination with Primary Care Pharmacists |
|
|
| Coordination with Community Pharmacist |
|
|
| Geolocation |
|
|
| Coordination with Patient Associations |
|
|
PC: pharmaceutical care.
The HPS of the Complejo Hospitalario Universitario A Coruña (1,456 beds) has six outpatient PC consultations by appointment, where 20 pharmacists attend 18 external consultations schedules (13,000 patients and 50,000 consultations in 2019, approximately). During the pandemic, teleconsultation with home drug delivery (enteral nutrition and clinical trials included) was extended to 100% of patients with a new standard operating procedure. Teleconsultation was performed (with prior notice by SMS message), with the same activities as in face-to-face consultation (i.e. review of clinical and analytical records, assessment of adherence, comprehensive review of treatment, detection of interactions and adverse events, documentation of ongoing clinical PC, scheduling of new appointments) and requesting the patient's verbal consent for home drug delivery. The treatment was delivered on the day of the patient's appointment by an external company bound by a privacy and confidentiality contract, and in guaranteed storage conditions. Two pharmacy technicians and an administrative assistant were hired, and a part-time pharmacist coordinated all the logistics. Over the first eight weeks, 3,954 patients were seen and 5,975 teleconsultations were made (5,446 on medicines, 479 on enteral nutrition, and 50 on clinical trials), with 0.8% of delivery incidents. The overall satisfaction of outpatients (satisfaction survey; 95% confidence; accuracy ± 0.2 points) was 9.7 ± 0.7 on a 10-point scale, with similar results in aspects such as messaging, privacy, confidentiality, and PC.
The aim is to promote Telepharmacy in outpatient PC after the end of the pandemic as a complementary service to face-to-face consultations in the HPS.
Coordination with Primary Care Pharmacists. Seville-South Primary Healthcare Area (Hospital Universitario Virgen de Valme)The HPS of the Hospital Virgen de Valme in Seville (617 beds) has three outpatient PC consultations that provide their services by appointment with pharmacists (19,000 consultations and 4,500 patients in 2019, approximately). It has a standardized Telepharmacy operating procedure, which is the basis for the development of outpatient PC procedure during the pandemic.
Initially, the procedure established the informed delivery of medicines through the Primary Health Care Center network in the healthcare area (CCSS).
Currently, its objective is to maintain continuity in PC, prolonging the persistence of treatments. The material and human resources involved were those already available plus the primary care pharmacists, who verified the correct distribution of medicines to primary health centers, based on the information sent from the HPS before distribution. The previously established circuits for delivery of other types of material were used to speed up response to urgent demand. In addition, a circuit was created in coordination with the specialist pharmacists of the Empresa Pública del Bajo Guadalquivir to deliver the medicines through their health centers, thus expanding the delivery area. By appointment, medications were dispensed to all outpatients in to primary health centers, except for patients diagnosed with severe asthma who required in-hospital drug administration. The method was as follows: prioritization of management based on prior appointment, patient's place of residence and pre-established dispensing pathways; teleconsultation where the service was offered, confirmation from the health center; establishment and communication of next appointment; dispensing; preparation and identification of shipment; advance communication to primary care pharmacists, collation, distribution, and informed delivery. Approximately 1,000 deliveries to primary health centers were made in eight weeks. The perspective is to continue with Telepharmacy, in accordance with the regulations in force, established guidelines and available resources, but with the approach and orientation established within the positioning published by the SEFH.
Coordination with Community Pharmacies. Hospital Universitario Marqués de Valdecilla de SantanderThe HPS of Hospital Universitario Marqués de Valdecilla (907 beds) has five pharmacy consultations that work by appointment, both in the Outpatient Unit and in the Oncology Pharmacy Unit (45,603 consultations made to 8,309 outpatients in 2019). A procedure for distributing medicines to spare patients from having to travel to the hospital was designed, and PC was encouraged through Telepharmacy by appointment.
Initially, the HPS requested home drug delivery associated with Telepharmacy. However, the model chosen by Regional Health Authorities was through coordination with community pharmacies and distribution warehouses. To this end, the parties executed an agreement and a temporary delivery procedure was established through community pharmacies. The General Directorate of Planning, Pharmacy and Inspection of the Regional Department of Health coordinated the agents involved and ensured compliance with the regulations in obtaining the patient's verbal consent and on the confidentiality of the treatments delivered to the community pharmacies. A joint protocol was developed to ensure correct pharmaceutical care, and the safe and traceable distribution and dispensing of medication.
At first, the service was offered to the most vulnerable patients (transplant recipients, respiratory diseases, etc.) and without other face-to-face consultations in the hospital. As the pandemic worsened, the HPS extended the scope to all patients. In the first phase, 110 of the 273 existing community pharmacies were selected, but at the third week, the protocol was modified to improve the safety of the consignments and the staff involved, so the offer was extended to all community pharmacies in the region of Cantabria. The procedure did not entail any additional costs at the level of distribution warehouses and community pharmacies, but required five additional pharmacists at the HPS (due to the cessation of other care activities) and the establishment of an afternoon shift (due to staff security and complexity of the procedure), which complicated its maintenance once regular hospital activities had been resumed.
In eight weeks, 2,008 deliveries were made to community pharmacies for the 4,805 patients seen in both units (42%), 46% of patients in the Outpatient Unit and 27% in the Oncology Pharmacy Unit. Only 57 deliveries were made to the 1,055 HIV-dependent patients in the outpatient unit due to lack of confidentiality. Although we do not have specific data, and even though the patients who accepted deliveries to community pharmacies were grateful, it is not representative because they represent only 40% of the population attended on these dates, and there were several patients from the outpatient unit who rejected this procedure.
Considering the limitations of this procedure (Table 1), the HPS is not committed to continuing with this model, which it considers inefficient. Instead, it opts for Telepharmacy with home drug delivery, which was previously included among our objectives.
Dispensing and informed delivery through geolocation (Complejo Hospitalario Universitario de Vigo)Outpatient PC in the HPS of the Complejo Hospitalario Universitario de Vigo (CHUVI, 1,325 beds) is provided by six pharmacists by appointment in six consultations (13,356 patients and 51,143 consultations in 2019).
During the pandemic, Telepharmacy was strengthened in coordination with healthcare services. The procedure enabled two dispensing points for medicines and enteral nutrition in each of the CHUVI hospitals, where patients can enter on their private car without entering the hospital, and organized home dispensing for patients with mobility problems. This model involves pharmacists, nurses, pharmacy technicians, and orderlies. On a technological level, the procedure integrates a corporate geolocation system that indicates to the patient by SMS message the location and route to the delivery points by means of real-time coordinates. Clinical services (rheumatology) and patient associations (psoriatic arthritis [ASEARPO], multiple sclerosis [AVEMPO], hemophilia, cystic fibrosis) have collaborated. PC procedure includes the following: (i) review of the patient's clinical history by appointment and assessment of their suitability for inclusion in this program; (ii) PC teleconsultation (i.e. therapeutic validation, clinical follow-up, assessment of adherence, training, and information); (iii) documentation of PC in the clinical history; (iv) assignment of date, time slot and sending of SMS message; (v) preparation and shipping of the treatment to the pick-up point; (vi) assignment of next appointment; and (vii) dispensing of medication. All patients cited in the HPS were included, except if they had another face-to-face appointment or treatment initiation/change. During eight weeks, 3,095 patients were treated with this procedure (55% of the total), and 195 received their medication at home. The extraordinary perception of quality of the new model was received through multiple signs of appreciation from patients. Nevertheless, a survey on the quality of outpatient PC is planned within the framework of the SATISFAR 2.0 project.
Based on our assessment of advantages and limitations (Table 1), we consider that Telepharmacy was a useful tool during the health alarm period. Moreover, it made it possible to maintain the quality of PC, involving the patient in the dispensing process as the person ultimately responsible for their treatment. Therefore, our plan is to promote Telepharmacy in the consultations of the pharmacy service.
Coordination with Patient Associations (Hospital Universitari i Politècnic La Fe, Valencia)The Outpatient PC Unit of the HPS of the Hospital Universitari i Politècnic La Fe attended 12,237 patients and had 60,349 visits in 2019. As a result of the COVID-19 pandemic, and with the support of the General Directorate of Pharmacy and Health Products of the Regional Department of Health of the Generalitat Valenciana, a system of telematic PC and informed home delivery through a courier company was implemented. In addition, a home dispensing procedure was maintained for hemophilic patients, coordinated with a patient association (ASHECOVA, Hemophilia Association of the Community of Valencia), to carry out home dispensing of the coagulation factor and any prescribed hospital treatment. The procedure involves that patients delegate in writing the pick-up of their treatment at the outpatient PC unit to a person linked to ASHECOVA. Through a specific software package validated by the Hospital Systems Unit, the outpatient PC unit and ASHECOVA coordinate to establish a schedule for the delivery of medication, always after the clinical history has been reviewed, contacting, and solving any incident related to the treatment. Deliveries are made twice a week for a period of four weeks. The PC services provided are the same as in a face-to-face consultation (i.e. validation of the prescription and possible changes, review of clinical history, evaluation of possible adverse effects, adherence to treatment, need for supplementary doses of coagulation factor, etc.). Additionally, emphasis is placed on the correct storage of the medicines during transport and storage at home, and on the traceability of the entire process. Table 1 lists the main advantages and limitations identified in this procedure.
Over the first eight weeks of confinement, 63 patients were attended, 139 consultations were carried out, and 258 dispensations were made. In the last satisfaction survey, conducted in 2017, the overall score of the program by patients was 9.7 on a 10-point scale, with no communication of confidentiality problems.
Learned lessons. Future applicability in Hospital Pharmacy Services
Based on the procedures described and the assessments made, the following lessons were learned in relation to outpatient pharmaceutical care in hospital pharmacy services during the state of alarm:
- –
Hospital pharmacy services have demonstrated their ability to react to a health crisis by urgently adapting their procedures and maintaining their responsibility for hospital outpatient pharmaceutical care.
- –
Telepharmacy has demonstrated its usefulness in all applications that shows the Spanish Society of Hospital Pharmacy Statement on Telepharmacy and MAPEX (clinical monitoring, care coordination, patient information, dispensing, and informed home drug delivery), with high patient satisfaction.
- –
Hospital pharmacy services must promote Telepharmacy as a complementary tool in a mixed model of hospital outpatient pharmaceutical care that incorporates the advantages of each procedure, adapting to the individual needs of patients in an environment of humanization of healthcare.
Our thanks to patient associations, the Spanish Society of Hospital Pharmacy, primary care pharmacists, pharmaceutical distribution companies, the State Security Forces and Corps, local authorities and police, and the pharmaceutical industry.