To assess the long-term cost-effectiveness of 12 months treatment of prasugrel compared to clopidogrel in patients with acute coronary syndrome (ACS) undergoing percutaneous coronary intervention (PCI) in the Spanish health care system.
MethodsA Markov state transition model was developed to estimate health outcomes, quality adjusted life years (QALYs), life years (LY), and costs over patients’ lifetimes. Clinical inputs were based on an analysis of the TRITON-TIMI 38 clinical trial. Hospital readmissions captured during the trial in a sub-study of patients from eight countries (and subsequent re-hospitalisations modelled to accrue beyond the time horizon of the trial), were assigned to Spanish diagnosis-related group payment schedules to estimate hospitalisation costs.
ResultsMean total treatment costs were €11,427 and €10,910 for prasugrel and clopidogrel respectively. The mean cost of the study drug was €538 higher for prasugrel vs. clopidogrel, but rehospitalisation costs at 12 months were €79 lower for prasugrel due to reduced rates of revascularisation. Hospitalisation costs beyond 12 months were higher with prasugrel by €55, due to longer life expectancy (+0.071 LY and +0.054 QALYs) associated with the decreased nonfatal myocardial infarction rate in the prasugrel group. The incremental cost per life year and QALY gained with prasugrel was €7,198, and €9,489, respectively.
ConclusionsConsidering a willingness-to-pay threshold of €30,000/QALY gained in the Spanish setting, prasugrel represents a cost-effective option in comparison with clopidogrel among patients with ACS undergoing PCI.
Evaluar a largo plazo el coste-efectividad de 12 meses de tratamiento con prasugrel frente a clopidogrel en pacientes con síndrome coronario agudo (SCA) sometidos a intervención coronaria percutánea (ICP) desde la perspectiva del sistema nacional de salud español.
MétodosSe desarrolló un modelo de Markov de transición entre estados para estimar los resultados en salud, los años de vida ajustados por calidad (AVACs), los años de vida (AV) y los costes a lo largo de la vida de los pacientes. Los datos clínicos fueron obtenidos de un análisis del ensayo clínico TRITON-TIMI 38. Los reingresos hospitalarios registrados durante el ensayo en un subestudio de pacientes provenientes de ocho países, (y las subsiguientes rehospitalizaciones fueron modeladas para acumularse más alla del horizonte temporal del ensayo) fueron asignados a grupos relacionados con el diagnóstico españoles para estimar los costes de hospitalización.
ResultadosLos costes medios totales del tratamiento con prasugrel y clopidogrel fueron 11.427 € y 10.910 €, respectivamente. El coste medio del fármaco fue 538 € superior para prasugrel frente a clopidogrel, pero los costes de rehospitalización a los 12 meses fueron 79 € menores para prasugrel debido a la reducción en las tasas de revascularización. Los costes de hospitalización más allá de los 12 meses fueron 55 € superiores con prasugrel, debido a la mayor esperanza de vida (+0,071 AV y +0,054 AVACs) asociada a la reducción de la tasa de infartos de miocardio no mortales en el grupo de prasugrel. El coste-efectividad incremental por año de vida y AVAC ganado con prasugrel fue 7.198 € y 9.489 €, respectivamente. Conclusión: Considerando el umbral de disponibilidad a pagar de 30.000 €/AVAC para España, prasugrel representa una opción coste-efectiva en comparación con clopidogrel en pacientes con SCA sometidos a ICP.
Acute coronary syndrome (ACS) is a major cause of morbidity and mortality, and imposes significant costs on healthcare systems.1 ACS is a pathophysiologic continuum ranging from unstable angina (UA) to non-ST-segment elevation myocardial infarction (NSTEMI) to ST-segment elevation myocardial infarction (STEMI). Current guidelines recommend early diagnostic cardiac catheterisation and percutaneous coronary intervention (PCI) within 2 hours for STEMI patients2,3, and within 72 hours for moderate to high risk NSTEMI patients.4,5
Platelets play a key role in the pathogenesis of atherothrombotic complications that may occur due to plaque rupture in ACS and PCI. Therefore, dual antiplatelet therapy with aspirin and clopidogrel has been recommended in practice guidelines for ACS patients undergoing PCI to prevent ischemic events.3-6
The Trial to Assess Improvement in Therapeutic Outcomes by Optimizing Platelet Inhibition With Prasugrel-Thrombolysis in Myocardial Infarction 38 (TRITON-TIMI 38) demonstrated that prasugrel, significantly reduced, compared to standard-dose clopidogrel, the composite endpoint of cardiovascular death, non fatal myocardial infarction or non-fatal stroke in ACS patients undergoing PCI treated with aspirin for up to 15 months. Prasugrel was associated with a significant increase in the rate of bleeding.7 Analysis of net clinical benefit (defined as the rate of death from any cause, nonfatal myocardial infarction, non-fatal stroke, or non-CABG-related non-fatal TIMI major bleeding), however, favoured prasugrel over clopidogrel in the overall patient population.7 There were three subgroups of patients, however, among whom prasugrel did not have a favourable net clinical benefit: patients who had prior history of stroke or transient ischemic attack had net harm from prasugrel, while net clinical benefit among patients aged &75 years and patients weighing less than 60 kg was neutral.7 The European Medicines Agency (EMA) approved prasugrel to be given as a loading dose of 60 mg and followed with 12 months of treatment with a daily 10 mg dose in ACS patients undergoing PCI, with prasugrel contraindicated in patients with previous stroke or TIA. The label also reflects the higher rates of bleeding in patients a:75 years old and patients weighing < 60 kg in recommending a reduced maintenance dose (5 mg) for these patients.8 In patients a 75 years old, the use of prasugrel was generally not recommended and a careful benefit/risk evaluation needs to be performed and prasugrel used when the benefits of ischemic events prevention outweighs bleeding risks (Efient® SPC).8
Given the increasing pressures on health care budgets, it is necessary to assess health interventions not only in terms of their safety and efficacy but also in terms of their cost-effectiveness. Economic evaluation of competing healthcare interventions compares these in terms of their incremental costs and benefits, such as quality adjusted life years (QALYs), expressing cost-effectiveness in terms of incremental cost per QALY. Cost-effectiveness analyses have shown prasugrel to be cost-saving in a US setting, based on substantial reductions in re-hospitalisation costs.9 The present study evaluates the long-term cost-effectiveness, in terms of both cost per life year and cost per QALY gained, from the perspective of the Spanish health care system, of treating ACS patients undergoing PCI, with prasugrel compared to clopidogrel for a period of time of 12 months. The base case analysis considers the overall licensed population in TRITON-TIMI 38 (defined as all patients other than those with prior stroke or TIA and including patients who are now recommended to be treated with a 5 mg maintenance dose). The analysis is based on a model the main elements of which are briefly described below. Further details of the model, including the risk equations based on TRITON TIMI-38 that it employs, have been reported elsewhere.10
MethodsThis cost-effectiveness analysis compares 12 months treatment with prasugrel (60 mg loading dose and 10 mg daily maintenance dose) to 12 months treatment with clopidogrel (a 300 mg loading dose and a 75 mg daily maintenance dose) using a lifetime horizon. Detailed model methods have previously been described elsewhere.10
Briefly, a Markov state transition model was developed to estimate health outcomes, life years (LYs), quality adjusted life years (QALYs), and costs over the patients’ lifetimes. Life years and QALYs were modelled as a function of index ACS type and events occurring during 12 months of treatment. Individual patient data from TRITON-TIMI 38 were used to construct a series of risk equations to estimate the risks of clinical events. The equations predict the risk of the primary endpoint in the trial of cardiovascular death, non-fatal MI or stroke, and its key safety endpoint, TIMI major or minor bleeding (including CABG bleeds) over the 12 month period of treatment conditional on patients’ clinical characteristics at baseline and treatment allocation. Following the 12 month treatment period, risks for all-cause mortality are increased by non-fatal myocardial infarctions and strokes that are predicted to have occurred during the treatment period. The Markov state transition model approximated a lifetime horizon for the analysis (maximum survival of 40 years following the index ACS event).
Costs and outcomes were discounted at an annual rate of 3% according to current Spanish recommendations.11Table 1 presents a summary of the inputs used in the model.
Summary of key base-case model inputs
| Input | Value | Source |
|---|---|---|
| Discount rate | 3% per annum | Lopez Bastida et al.11 |
| RRs (95% confidence intervals) for post-trial | ||
| all-cause mortality† | ||
| UA/NSTEMI | 1.55 (1.31-1.84) | Allen et al.19 |
| STEMI | 1.84 (1.54-2.20) | Allen et al19 |
| Re-infarcted NSTEMI | 2.93 (2.34-3.66) | Mueller et al.12 |
| Re-infarcted STEMI | 3.48 (2.77-4.37) | Mueller et al.12 |
| Stroke | 2.39 (1.44-3.97) | Taneja et al.13 |
| HRQoL decrements: | ||
| ACS | 0.0409 (±0.0002) | Sullivan et al.21 |
| Stroke | 0.0524 (±0.0002) | Sullivan et al.21 |
| TIMI major bleed‡ | 25% decrement to population | Assumption based on |
| norm over 14 days | Wechowski et al.22 | |
| Estimated cost per hospitalisation (Euros, 2013) | ||
| Clopidogrel | 5.829 | Calculated from DRGs (see table 2) |
| Prasugrel | 5.535 | Calculated from DRGs (see table 2) |
| Drug acquisition costs | ||
| Clopidogrel | 0.60 | BOT23 |
| Prasugrel (branded) | 2.10 | BOT23 |
| Aspirin (low dose) | 0.05 | BOT23 |
RR: Relative risk; ACS: Acute coronary syndrome; UA/NSTEMI: Unstable angina/non-ST segment elevation myocardial infarction; STEMI: ST segment elevation myocardial infarction; HRQoL: Health related quality of life.
†In addition to cited source relative risk is derived using Rosengren et al.18
‡Population norms according to Kind et al.20
Figure 1 shows the model pathways (rectangles represent model states and arrows between ovals represent transitions between those states), for the Markov model. The model consists of two phases: one representing 12 months of treatment following PCI for ACS and the second representing remaining potential life expectancy. Patients enter the model and face risks for cardiovascular death, non-fatal MI, or non-fatal stroke, and bleeding (fatal, major or minor), during the 12 months antiplatelet treatment phase. Patients’ longer term mortality is then predicted based on the occurrence of events over the first 12 months. Though further events will occur over patients’ remaining lifetimes, an average effect of these further (unobserved) events on long term mortality is reflected in the relative risks for all-cause mortality employed in the model.12,13
Risk equationsSeparate risk equations were generated for the unstable angina/non-ST segment elevation myocardial infarction (UA/NSTEMI) and ST segment elevation myocardial infarction (STEMI) populations due to their different risk profiles. The equations adjusted for baseline characteristics and treatment interaction effects with prior stroke or TIA; a potential interaction with diabetic patients is also included. The model is designed to address the licensed population, and does not include separate interaction effects for age &75 years and weight < 60 kg. Due to a rapidly declining risk of events following the index procedure, logistic models were employed to model events within three days of randomization,14 and Weibull functions15 were applied over the remainder of the trial period.
Combined endpoint events are disaggregated using multinomial logistic regression functions that predict the probability of events being each of the components listed above.
Treatment effectsThe effectiveness of clopidogrel and prasugrel, in terms of the relative rate of clinical events over the 12 month treatment phase, was estimated within each of the risk functions. These effects are consistent with the overall published trial results.7
SurvivalDuring the trial phase, the risk of non-cardiovascular mortality, stratified by age and sex, is based on Spanish national life tables adjusted to exclude cardiovascular mortality.16,17 To estimate mortality beyond the trial period, the model accounted for the additional risk associated with revascularised ACS compared to the general population,18 and the further risk faced by patients who experienced non-fatal MI or non-fatal stroke during the trial period (Table 1).12,13,19
QALYsQuality-adjusted survival, in the form of QALYs, was derived by weighting patients’ survival time by estimates of health-related quality of life (HRQoL) that reflect the impact of clinical events. The model applies HRQoL weights to all patients based on age and sex specific EQ-5D population norms.20 Adjustment for non-fatal MI (including qualifying ACS event) and non-fatal stroke employed EQ-5D based decrements taken from the US Medical Expenditure Panel Survey (Table 1).21 A temporary decrement is applied for major bleeds,22 equivalent to 25% of patients’ quality of life at the time of the bleed event.
Medication costsFor the base case analysis, the daily cost of antiplatelets were €0.60 for clopidogrel (the cost for both generic and branded clopidogrel, i.e. Plavix® and Iscover®), and €2.10 for prasugrel.23 Costs for clopidogrel and prasugrel, in combination with aspirin, were applied over the duration of the 12 months maintenance treatment phase.
Other costsCosts relating to re-hospitalisations beyond the index admission were based on hospitalisation data collected in an economic sub-study of TRITON-TIMI 38 involving all study patients (n = 6,705) enrolled in eight pre-specified countries (USA, Australia, Canada, Spain, Italy, UK, Germany, France).9 The economic sub-study identified re-hospitalisations that were considered by a clinician blinded to treatment arm to potentially relate to the ACS condition or the PCI intervention, and that were separate hospitalisations to the index episode, these included both planned and unplanned PCI. Spanish diagnosis related groups (DRGs) were inflated to 2013 costs and mapped to the clinically assigned United States DRGs for each hospitalisation in the TRITON economic sub-study24. Weighted average costs per hospitalisation were then calculated (based on the distribution of DRGs in each trial arm) (Table 2). Poisson regression, using panel data methods,25 was used to estimate the rate of re-hospitalisation associated with clinical events over the trial period. Costs are modelled over the trial period by assigning the average re-hospitalisation costs for each arm (Table 2). After the 12 month treatment horizon, a common cost per year was applied to the modelled re-hospitalisations.
DRGs and unit costs assigned to re-hospitalisations9,24
| DRG description | Incidence of rehospitalization | ||
|---|---|---|---|
| 2013 cost (€) | Clopidogrel | Prasugrel | |
| Intracranial Hemorrhage or Cerebral Infarction | € 5,669 | 31 | 28 |
| Transient Ischemic Attack & Precerebral Occlusions | € 5,877 | 15 | 18 |
| Nonspecific Cerebrovascular Disorders w CC | € 3,107 | 1 | 0 |
| Hyphema | € 1,750 | 0 | 1 |
| Other Disorders of the Eye Age >17 w CC | € 2,988 | 1 | 1 |
| Epistaxis | € 2,213 | 3 | 5 |
| Other Ear, Nose, Mouth & Throat Diagnoses Age > 17 | € 1,505 | 1 | 1 |
| Pulmonary Embolism | € 4,576 | 1 | 7 |
| Pulmonary Edema & Respiratory Failure | € 3,978 | 1 | 4 |
| Chronic Obstructive Pulmonary Disease | € 2,826 | 0 | 1 |
| Respiratory Signs & Symptoms w CC | € 2,806 | 2 | 4 |
| Cardiac Valve & Oth Major Cardiothoracic Proc w Card Cath | € 25,955 | 1 | 2 |
| Coronary Bypass w Ptca | € 30,938 | 1 | 3 |
| Coronary Bypass w Card Cath | € 23,327 | 69 | 63 |
| Prm Card Pacem Impl w AMI, hrt Fail or Shk,or AICD Lead or Gnrtr | € 9,242 | 2 | 3 |
| Cardiac Pacemaker Revision except Device Replacement | € 3,912 | 1 | 0 |
| Circulatory Disorders w AMI & Major Comp, Discharged Alive | € 6,392 | 60 | 43 |
| Circulatory Disorders w AMI w/o Major Comp, Discharged Alive | € 4,840 | 1 | 0 |
| Circulatory Disorders w AMI, Expired | € 4,673 | 5 | 4 |
| Circulatory Disorders except AMI, w Card Cath & Complex Diag | € 4,977 | 67 | 66 |
| Circulatory Disorders except AMI, w Card Cath w/o Complex Diag | € 3,199 | 2 | 2 |
| Heart Failure & Shock | € 3,560 | 50 | 53 |
| Deep Vein Thrombophlebitis | € 2,302 | 5 | 8 |
| Cardiac Arrest, Unexplained | € 3,353 | 4 | 1 |
| Peripheral Vascular Disorders w CC | € 3,386 | 42 | 38 |
| Atherosclerosis w CC | € 2,946 | 25 | 23 |
| Cardiac Congenital & Valvular Disorders Age > 17 w CC | € 3,670 | 1 | 4 |
| Cardiac Arrhythmia & Conduction Disorders w CC | € 2,808 | 1 | 2 |
| Cardiac Arrhythmia & Conduction Disorders w/o CC | € 1,817 | 53 | 71 |
| Angina Pectoris | € 2,307 | 49 | 59 |
| Syncope & Collapse w CC | € 2,716 | 20 | 27 |
| Chest Pain | € 1,835 | 45 | 52 |
| Other Circulatory System Diagnoses w CC | € 3,959 | 22 | 36 |
| G.I. Hemorrhage w CC | € 4,005 | 59 | 81 |
| Dental & Oral Dis except Extractions & Restorations, Age > 17 | € 2,472 | 0 | 1 |
| Other Digestive System Diagnoses Age >17 w CC | € 3,458 | 3 | 1 |
| Kidney & Urinary Tract Infections Age >17 w CC | € 3,026 | 0 | 1 |
| Kidney & Urinary Tract Signs & Symptoms Age >17 w CC | € 2,543 | 7 | 12 |
| Menstrual & Other Female Reproductive System Disorders | € 1,317 | 1 | 1 |
| Traumatic Injury Age >17 w CC | € 3,331 | 1 | 4 |
| Complications of Treatment w CC | € 3,395 | 0 | 3 |
| Other Vascular Procedures w CC | € 8,011 | 12 | 12 |
| Cardiac Defibrillator Implant w/o CardCath | € 9,092 | 1 | 0 |
| Percutaneous Cardiovasc Proc w AMI | € 7,483 | 0 | 2 |
| Perc Cardio Proc w Coronary Artery Stent w/o AMI | € 4,795 | 2 | 2 |
| Perc Cardio Proc w/o Coronary Artery Stent or AMI | € 4,978 | 7 | 3 |
| Percutaneous Cardiovascular Proc w Drug Eluting Stent w AMI | € 7,940 | 109 | 68 |
| Percutaneous Cardiovascular Proc w Drug Eluting Stent w/o AMI | € 5,105 | 471 | 403 |
| Extracranial Procedures w CC | € 9,941 | 0 | 1 |
| Cardiac Defib Implant w Cardiac Cath w AMI/HF/Shock | € 18,311 | 0 | 1 |
| Cardiac Defib Implant w Cardiac Cath w/o AMI/HF/Shock | € 14,803 | 4 | 2 |
| Weighted average cost per re-hospitalization | €5,829 | €5,535 | |
AICD: Automated implantable cardioverter-defibrillator; AMI: Acute myocardial infarction; Card Cath: Cardiac catheterization; Cardio: Cardiovascular; CC: Complication or comorbidity; Comp: Complications; Dis: Disorder; GI: Gastrointestinal; Gnrtr: Generator; hrt Fail: Heart failure; HF: Heart failure; oth: Other; Perc: Percutaneous; Prm Card Pacem Impl: Permanent Cardiac Pacemaker implant; proc: Procedure; PTCA: Percutaneous transluminal coronary angioplasty; Shk: Shock; w: With; w/o: Without.
Analyses were performed by running the model sequentially for all 13,090 patient profiles in TRITON that satisfy prasugrel’s licenced population (defined as all patients other than those with prior stroke or TIA, including patients who are now recommended to be treated with a 5 mg maintenance dose). Cost-effectiveness analyses are presented with mean costs, life years gained, and QALYs, along with incremental cost-effectiveness ratios (ICERs), for the licensed population and subgroups of UA/NSTEMI, STEMI, and diabetic patients, and those aged less than 75 with weight of 60 kg or above (TRITON-TIMI 38’s ‘core’ clinical cohort 10 mg treatment population26).
Model parameters were entered in the model as probability distributions where appropriate to facilitate probabilistic analysis.27 Deterministic sensitivity analyses were also performed to examine the impact of specific alternative assumptions regarding discount rates; utility decrements for haemorrhage, MI and stroke; relative risks for all-cause mortality for the extrapolation phase and DRG costs. Deterministic sensitivity analyses were performed by re-running the model for each of the patient profiles in the licensed population under each scenario examined. Probabilistic analysis was based on the profile with median cost-effectiveness (defined as the profile with median net benefit, calculated as the value of prasugrel’s incremental QALYs using a threshold value of €30,000 per QALY, less incremental costs), when the model was run deterministically for all 13,090 profiles in the overall licensed population.
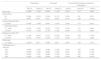
ResultsEffectivenessThe primary endpoint occurred in the model in 11.28% of Clopidogrel patients in the overall licensed population compared with 8.87% of prasugrel patients, with the reduction driven primarily by myocardial infarction (8.49% for clopidogrel vs. 6.43% for prasugrel). The model predicted a numerical reduction in cardiovascular death (2.05% for clopidogrel vs. 1.76% for prasugrel) and little difference in the incidence of stroke (0.74% and 0.69% for clopidogrel and prasugrel respectively) (Table 3). Total bleeding events (TIMI major or minor, CABG and non-CABG) for the overall licensed population were higher at 12 months in the prasugrel group (4.81% with prasugrel vs. 3.64% with clopidogrel). These event rates were modelled over a lifetime to yield 0.071 additional life-years and 0.054 additional QALYs per patient with prasugrel compared to clopidogrel.
Cost-effectiveness results for overall licensed population and specific sub-groups (event rates at 12 months)
| Overall licensed population n = 13,090 | UA-NSTEMI n = 9,669 | STEMI n = 3,421 | ACS diabetes n = 2,947 | Core Cohort* n = 10,804 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Clopidogrel | Prasugrel | Clopidogrel | Prasugrel | Clopidogrel | Prasugrel | Clopidogrel | Prasugrel | Clopidogrel | Prasugrel | |
| Modelled event probabilities: | ||||||||||
| Cardiovascular death | 2.05% | 1.76% | 1.81% | 1.66% | 2.76% | 2.05% | 3.59% | 2.73% | 1.57% | 1.36% |
| Myocardial infarction | 8.49% | 6.43% | 8.60% | 6.61% | 8.17% | 5.91% | 10.64% | 6.72% | 8.15% | 6.21% |
| Stroke | 0.74% | 0.69% | 0.72% | 0.54% | 0.79% | 1.12% | 1.23% | 1.01% | 0.64% | 0.58% |
| Total combined endpoint | 11.28% | 8.87% | 11.13% | 8.80% | 11.71% | 9.08% | 15.46% | 10.47% | 10.36% | 8.14% |
| Fatal bleed | 0.00% | 0.11% | 0.00% | 0.11% | 0.00% | 0.12% | 0.00% | 0.15% | 0.00% | 0.05% |
| Major bleed | 1.71% | 2.19% | 1.49% | 2.07% | 2.32% | 2.52% | 2.21% | 2.35% | 1.50% | 1.94% |
| Minor bleed | 1.93% | 2.51% | 1.69% | 2.40% | 2.61% | 2.82% | 2.70% | 2.93% | 1.47% | 1.96% |
| Total bleed (major or minor) | 3.64% | 4.81% | 3.18% | 4.58% | 4.93% | 5.46% | 4.91% | 5.43% | 2.97% | 3.95% |
| Mean cost per patient (€) | ||||||||||
| Drugs | 213 | 751 | 214 | 752 | 214 | 752 | 211 | 746 | 214 | 755 |
| Hospitalisations < 12 months | 988 | 910 | 996 | 917 | 996 | 917 | 1,099 | 964 | 969 | 892 |
| Hospitalisations > 12 months | 10,207 | 10,262 | 10,225 | 10,267 | 10,225 | 10,267 | 9,588 | 9,724 | 11,052 | 11,107 |
| Total costs | 11,409 | 11,923 | 11,435 | 11,936 | 11,435 | 11,936 | 10,898 | 11,434 | 12,235 | 12,754 |
| Mean outcomes per patient | ||||||||||
| Life years | 14.017 | 14.089 | 14.04 | 14.10 | 13.95 | 14.07 | 13.21 | 13.39 | 15.10 | 15.17 |
| QALYs | 10.828 | 10.883 | 10.83 | 10.87 | 10.82 | 10.91 | 10.16 | 10.29 | 11.70 | 11.76 |
| ICER (€) vs. clopidogrel | ||||||||||
| Cost per LY gained | 7,198 | 9,367 | 4,514 | 2,987 | 7,291 | |||||
| Cost per QALY gained | 9,489 | 12,414 | 5,913 | 3,935 | 9,582 | |||||
ACS: Acute coronary syndrome; UA/NSTEMI: Unstable angina/non-ST segment elevation myocardial infarction; STEMI: ST Segment elevation myocardial infarction; LY: Life year; QALYs: Quality adjusted life years; ICER: Incremental cost-effectiveness ratio.
+Core cohort: those aged less than 75 and weighing 60 kg or above.
The mean total treatment costs were € 11,923 and € 11,409 for prasugrel and clopidogrel respectively (Table 3). The mean cost of study drug was €538 higher for prasugrel compared to clopidogrel, but rehospitalisation costs at 12 months were €79 lower for prasugrel due to reduced rates of revascularisation. Hospitalisation costs beyond 12 months were higher with prasugrel by €55, due to the longer life expectancy. Life expectancy modelled on the basis of the 12 month event rates was 14.09 and 14.02 years for prasugrel and clopidogrel respectively, a gain of 0.071 life years with prasugrel. Clopidogrel’s average quality adjusted survival was 10.83 QALYs compared to 10.88 for prasugrel, an advantage of 0.054 QALYs. The incremental cost per life year and QALY gained with prasugrel was €7,198 and €9,489, respectively (Table 3).
Sub-group analysisConstant treatment effects were applied across all patients in the UA/NSTEMI and STEMI risk functions with the exception of diabetes. Sub-group analyses are presented that reflect heterogeneity in risks of events by baseline characteristics. Although prasugrel was highly cost-effective in the STEMI and diabetes groups, subpopulations with a higher risk of ischaemia, (€ 5,913 and €3,935 per QALY respectively), prasugrel was also cost-effective in the UA-NSTEMI group, for which the cost per QALY was €12,414.
Sensitivity analysisIn the deterministic sensitivity analysis changes to model assumptions, including a 5% discount rate, doubling the cost of re-hospitalisations and increasing the disutility associated with a bleed, reducing the quality of life and long term mortality impact of non-fatal events, had little impact on the cost-effectiveness of prasugrel, with the ratio remaining below €13,000 per QALY gained, or under (Table 4). Reducing the price of clopidogrel to 80% of the current price (to €0.12 per day) resulted in the ICER increasing only to €12,636. Each deterministic sensitivity analysis reflects diversity in patients’ baseline characteristics by re-running the model for all patient profiles in TRITON, and aggregating these individual results. The cost-effectiveness acceptability curve in figure 2 is based on the patient profile with median cost-effectiveness.
Sensitivity analyses based on the licensed population
| Clopidogrel | Prasugrel | Incremental (Prasugrel compared to Clopidogrel) | |||||
|---|---|---|---|---|---|---|---|
| QALYs | Costs (€) | QALYs | Costs (€) | QALYs | Costs (€) | €/QALY | |
| Base case | 10,828 | 11,409 | 10,883 | 11,923 | 0.054 | 514 | 9,489 |
| Discounting | |||||||
| 0% | 15,464 | 16,159 | 15.553 | 16,715 | 0.089 | 557 | 6,257 |
| 5% | 8,900 | 9,437 | 8.941 | 9,933 | 0.041 | 496 | 12,134 |
| Haemorrhage disutility | |||||||
| 8 x base | 10,828 | 11,409 | 10.881 | 11,923 | 0.054 | 514 | 9,534 |
| Ml/stroke disutility | |||||||
| 1/2 * base | 10,870 | 11,409 | 10.925 | 11,923 | 0.054 | 514 | 9,464 |
| 2 x base | 10,744 | 11,409 | 10.798 | 11,923 | 0.054 | 514 | 9,539 |
| Ml/stroke mortality RR | |||||||
| 1/2 * base | 11,430 | 12,033 | 11.473 | 12,536 | 0.043 | 503 | 11,655 |
| 2 x base | 10,347 | 10,910 | 10.405 | 11,427 | 0.058 | 517 | 8,994 |
| DRG costs | |||||||
| 1/2 * base | 10,828 | 5,811 | 10.883 | 6,337 | 0.054 | 526 | 9,710 |
| Clopidogrel price reduction | |||||||
| -20% | 10,828 | 11,336 | 10,883 | 11,923 | 0.054 | 557 | 10,276 |
| -40% | 10,828 | 11,323 | 10,883 | 11,923 | 0.054 | 599 | 11,063 |
| -60% | 10,828 | 11,281 | 10,883 | 11,923 | 0.054 | 642 | 11,850 |
| -80% | 10,828 | 11,238 | 10,883 | 11,923 | 0.054 | 685 | 12,636 |
Ml: Myocardial infarction; DRG: Diagnostic reimbursement group; RR: Relative risk; QALYs: Quality adjusted life years.
Treatment with prasugrel was cost effective compared with clopidogrel among patients with an ACS undergoing PCI from the perspective of the Spanish healthcare system. Drug costs for prasugrel were higher than clopidogrel by €538 but this higher cost was partially offset by savings from reduced re-hospitalisations over one year. Prasugrel was associated with a non-significant reduction in the rate of cardiovascular death in TRITON-TIMI 38, however, life year gains will also accrue over the longer term principally due to the significantly lower rate of non-fatal MI. The model recognises, through the long term application of the rehospitalisation equation’s baseline admission rate, that surviving patients will continue to require a certain level of health care due to their underlying coronary disease irrespective of potential further events. Though the admission rates associated with modelled events could also have been applied over the long term, this would clearly have favoured prasugrel without evidence to support this. The approach taken may to this extent, therefore, be conservative with respect to prasugrel’s expected cost-effectiveness; although greater numbers of prasugrel patients remain alive and therefore at risk of further events, a greater proportion of surviving clopidogrel patients carry the added risk due to re-infarctions seen in the trial. Additional life-years and QALYs over the longer term result in incremental cost-effectiveness ratios below the Spanish threshold considered for cost-effectiveness (€30,000 per QALY).28 Sensitivity analysis showed prasugrel’s cost-effectiveness was robust to different assumptions within the model.
Though prasugrel is cost-effective in all sub-groups, it’s ICER is lower in those groups at higher risk of ischemic events - the STEMI and diabetic populations. The model reported here, however, is designed to assess prasugrel’s cost-effectiveness based on the licensed population in the trial, and accounts for prasugrel’s greater effectiveness in patients without prior TIA/stroke. Wiviott et al. have emphasised the greater effectiveness of prasugrel seen in patients with what they term a ‘core clinical cohort’, which includes not only those patients within TRITON TIMI-38 without prior TIA/stroke, but also those patients aged under 75 years with body weight a 60 kg. The model does not account for differences in treatment effects by age and weight, and the results reported for the core clinical cohort may therefore reflect conservative estimates of prasugrel’s likely QALY gains in these patients.
The results and sensitivity analyses presented in tables 3 (main results) and 4 (deterministic sensitivity analysis), are based on aggregating analyses for individual patient profiles, reflecting diversity in patients’ baseline characteristics in TRITON. To conduct probabilistic analyses on this basis, however, would be impractical as this would require several million iterations of the model. We therefore report a limited probabilistic analysis in Figure 2 that shows the probabilities of prasugrel being cost-effective at given thresholds for cost per QALY based on the patient profile in the overall licensed population with median cost-effectiveness.
Fatal bleeding is accounted for in the model, and the higher bleeding risk associated with prasugrel treatment can be expected to cease once patients stop treatment, in this case at a maximum of 12 months following PCI. This assumption is consistent with prior cost-effectiveness analyses of anti-thrombotic agents known to be associated with differences in bleeding rates.29 While bleeding has been associated with increased mortality over a long time period,30 Hochholzer et al., estimated the impact of serious bleeding on mortality in TRITON-TIMI 38.31 A declining HR over time following a non-fatal serious bleed stabilised after 40 days at approximately 1.38 (0.72-2.66).31 We explored our assumptions around bleeding in our analyses, and an eight-fold increase in the disutility associated with bleeds had little on the cost-effectiveness.
A potential limitation of the analysis concerns the utility estimates which are drawn from the US Medical Expenditure Panel Survey.21 Though these were based on the EQ-5D, the tariff used was that of the USA and so may not be representative of the Spanish population. However, the impact of the utility data assumptions were tested in the sensitivity analysis by varying the weights (utilities) attached to modelled events; reducing the impact of these events’ utility decrements by 50%, and increasing them by 100%, varied prasugrel’s cost per QALY by only ± €50.
In Spain, clopidogrel’s cost-effectiveness has been demonstrated by Badia et al.32 in a short-term trial based, and longer-term modelled analysis. The short-term incremental cost per event avoided of adding clopidogrel to standard therapy was €17,190; long-term incremental cost per life-year gained was €8,132.32 In an analysis by Latour-Perez et al.33 clopidogrel cost-effectiveness in NSTEMI patients, was shown to vary between €5,000 per QALY for high risk 40 year old patients and €30,000 for low risk 80 year olds.
ConclusionIn conclusion this analysis shows that treatment with prasugrel compared to clopidogrel in patients with ACS undergoing PCI in Spain represents a cost-effective use of health care resources.
Funding/disclosuresTRITON-TIMI 38 was funded by Daiichi Sankyo Company, Limited and Eli Lilly and Company. Economic analyses were funded by Eli Lilly and Company and undertaken by Oxford Outcomes. A. Barrett, JA Sacristán, T Huete and T Dilla are employees of Eli Lilly and Company.
Prasugrel frente a clopidogrel en pacientes con síndrome coronario agudo sometidos a intervención coronaria percutánea: análisis de coste-efectividad basado en un modelo español