It has been known, for decades, that the use of injectable medicines in European hospitals has been associated with frequent medication errors, some of which cause preventable severe harms and deaths. There have been national and European inquiries and reports concerning improving patient safety by recommending greater use of pharmacy aseptic preparation services and provision of ready-to administer injectables, which have not been widely implemented.
In England experience of treating patients with COVID-19 infections has brought into focus other benefits of significantly extending pharmacy aseptic preparation services. These benefits include saving nursing time, having systems in place which have resilience and capacity, reducing variation in practice, improving clinical staff and patient experience, and enabling more injectable medicines to be administered to patients at home. It has also been recognised that more action is required to standardise policies and procedures for injectable medicines and implement the use of smart infusion devices with dose error reduction software, to help minimise drug administration errors.
Hospital pharmacists have a key role in developing these services to bring European hospitals more in line with those provided by hospital pharmacies in North America.
Desde hace décadas se conoce que el uso de los medicamentos inyectables en los hospitales europeos se encuentra asociado a numerosos errores de medicación, algunos de los cuales provocan daños graves y muertes prevenibles. Se han publicado investigaciones e informes nacionales y europeos sobre la mejora de la seguridad del paciente que recomiendan una mayor utilización de las unidades de preparación aséptica de los servicios de farmacia y la provisión de los medicamentos inyectables listos para su administración, recomendaciones que apenas se han implementado.
En Inglaterra, la experiencia de tratar a los pacientes con infección por COVID-19 ha puesto de manifiesto otros beneficios que conlleva la ampliación de las unidades de preparación aséptica de los servicios de farmacia. Estos beneficios incluyen ahorrar tiempo de enfermería, disponer de sistemas con mayor resiliencia y capacidad, reducir la variabilidad en la práctica, mejorar la satisfacción del personal clínico y del paciente, y facilitar la administración de más medicamentos inyectables a los pacientes en sus domicilios. También se ha reconocido que se precisan actuaciones dirigidas a estandarizar las directrices y procedimientos de utilización de los medicamentos inyectables e implementar el uso de dispositivos de infusión inteligentes con software de reducción de errores de dosis, con el fin de minimizar los errores en la administración de estos medicamentos.
Los farmacéuticos de hospital tienen un papel clave en el desarrollo de estas actividades para que los servicios que prestan las farmacias hospitalarias europeas estén más en consonancia con los que se proporcionan en Norteamérica.
The significant risk for patient injury and death related to errors involving injectable medications is well known1,2. Errors with injectable medicines can be particularly dangerous because of the immediate onset of systemic effects, the narrow therapeutic index of many intravenous medications, as well as the limitations in reversing systemic effects after intravenous administration.
The use of injectable medicines in hospitals is a complex process and errors can occur at any step, but are most likely to happen during preparation and administration3,4. Studies carried out in Europe, where injectable medicines are commonly prepared on hospital wards, have shown that among the root causes and factors that contribute to these errors are inadequate training for preparation and administration of intravenous medications and complex design of equipment, including unsuitable working environment5,6. Error rates are lower when intravenous preparation takes place in pharmacy settings compared with hospital wards4, since hospital pharmacies have qualified personnel and a controlled environment to prepare medicines aseptically. It has been estimated that removing this step on the wards by providing aseptically prepared ready-to-use injections would reduce the overall error rate from 0.73 to 0.177.
The strategy in European hospital pharmacies in the past has been to propose a reduction in hospital medication errors by transferring the preparation of injectable medicines to the pharmacy8,9. In the United States, injectable preparation by hospital pharmacy is the standard of practice and required by the Joint Commission. However, this safety practice, except for the preparation of total parenteral nutrition and chemotherapy, has not been widely adopted by hospitals in Europe. In our opinion this is due to the lack of sufficient recognition of risks to patient arising from ward based preparation of injectable medicines and the resulting lack of resources by healthcare managers.
The COVID-19 pandemic has been a huge challenge for hospital pharmacy services10. The preparation of ready-to-administer injectable medications to support critical care areas and respond to nursing staff shortages has been one of the services provided by hospital pharmacies during the pandemic11,12. Currently, after the good feedback obtained, it is a practice that is being recommended for expansion13.
This article highlights the need to change systems for the preparation and administration of injectable medicines to meet changing priorities in European hospitals, and summarizes the evolution that the preparation of injectable drugs has had in England, where over the time it has been promoted the implementation of safe practices in this area and where the lessons learned in the COVID-19 pandemic have finally led to promoting the transformation of pharmacy aseptic services to accomplish injectable preparations and improve patient care.
Medication errors and hazards from injectable medicinesInjectable drugs are associated with higher medication error rates than oral medications14, because the process of use of injectable drugs involves several steps and presents multiple opportunities for errors. It is not the purpose of this article to conduct a review of the medication errors involving injectable drugs, but below we provide some data on the magnitude of the problem in Europe, as well as the main errors identified and their underlying causes, to understand the interventions proposed to avoid them.
Some early outstanding studies carried out in wards of European hospitals found errors rates in preparing and/or administering intravenous drugs were very high, of 22–49%5,6,14,15. The most frequent types of errors were wrong administration rate, omissions, co-administration of potentially incompatible medication as intermittent infusions, wrong dose, wrong preparation technique particularly when preparing drugs that required multiple steps, use of the wrong diluent, inaccuracies during calculation and poor aseptic technique5,6,14,15.
Common causes and/or contributory factors cited in these studies included lack of knowledge and competence of the staff on practical aspects of injectable medicine preparation and administration, training deficiencies in handling complex technology and equipment, lack or inadequate procedures, high workload, distractions and interruptions, deficiencies in the design of related equipment and unsuitable working environment6,14,15. Researchers concluded that there were uncontrolled risks in the intravenous processes and proposed several strategies to reduce these errors, such as: written procedures and standards, training in injectable drug preparation and administration, preparation of injectable drugs in pharmacy aseptic services, multidisciplinary teams involving clinical pharmacists, and changes in the design of equipment.
In a study reviewing 2,238 patient safety incidents involving predominantly injectable medicines, submitted from up to 29 critical care units each year in the North West of England between 2009 and 2012, 452 (20%) of these incidents led to actual harm to patients and 1,461 (65%) incidents were judged to have been preventable. Those most commonly reported involved the following injectable medicines: noradrenaline (161 incidents, 92 with harm), heparins (153 incidents, 29 with harm), morphine (131 incidents, 14 with harm) and insulin (111 incidents, 54 with harm). The administration of medicines was the stage in the process where incidents were most commonly reported. It was also the stage most likely to harm patients. Preparation of medicines was described as a factor in 266 incident reports (10% of total), the most common classifications being incorrect checking of the drug (109 incidents, 13 with patient harm), incorrect preparation (98 incidents, 12 with patient harm) and incorrect or no labelling of the drug (75 incidents, 3 with patient harm)16.
Medication administration errors persist in units with electronic prescribing and automated dispensing. In a disguised observational study in two clinical units using a computerized prescription order entry program with online pharmacy validation and decentralized profiled automated dispensing cabinets, where 402 intravenous administrations represented 17.4% of the number of opportunity of errors, the drug was not reconstituted/diluted according to the recommendations of the summary of product characteristics in 8.6% of intravenous administrations and wrong infusion rate were detected in 27 cases17.
A recent systematic review of the prevalence of intravenous medication errors in the United Kingdom18, which collected several of the previous studies14,15, found a weighted mean incidence of 101 intravenous medication errors per 1,000 administrations. Half were errors in medication administration, with the largest number of these errors involving the wrong rate of administration. The authors concluded that it was important to focus on interventions to mitigate these types of errors.
A study comparing the rate of errors in intravenous medicine preparation at the bedside in neonatal intensive care units vs the preparation error rate in a hospital pharmacy service found that calculation errors can be eliminated using protocols based on standard drug concentrations, and that accuracy error rates affected both neonatal intensive care units (55%) and hospital pharmacy services (34%), depending on the syringes and preparation techniques used19.
Contaminated injectable medications can cause severe complications to patients and increase morbidity in hospitals. A systematic review and meta-analysis on the period 2000–2018 found significantly higher contamination rates for the preparation of parenteral medication in the clinical environment compared to pharmacy environment: the overall contamination rate of doses prepared by nursing/ medical staff was 7.8%, and 0.08% for doses prepared by pharmacy staff20.
Although there is increasing recognition of occupational exposure of hazardous medicines, such as chemotherapy during dose preparation21, there is now also evidence of occupational exposure of nurses when preparing antibiotics in clinical areas22. This may result in adverse health effects such as hypersensitivity, allergic reactions, resistance, and anaphylactic shock.
Council of Europe recommendationsSafer preparation of injectable medicines was one of the best practices proposed in the report Creation of a better medication safety culture in Europe: Building up safe medication practices, developed for the Committee of Ministers of the Council of Europe in 2006 by a committee of experts8. The report states that the use of injectable medicines is growing, doses are prepared on hospital wards due to insufficient resources and multiple problems have been identified during the preparation that compromise patient safety.
The report strongly recommends that injectable dose preparation on nursing units be minimized by centralising aseptic dose preparation within hospital pharmacies and that products are prepared in ready-to-administer form.
In January 2011, the Committee of Ministers of the Council of Europe adopted the Resolution CM/Res AP(2011)1 on quality and safety assurance requirements for medicinal products prepared in pharmacies for the special needs of patients23. Five years later published additional guidance in the Resolution CM/Res(2016)2 on good reconstitution practices in health care establishments for medicinal products for parenteral use24, and the parent Resolution CM/Res AP (2011)1 was updated and reissued25.
The report defines “reconstitution” as the manipulation to enable the use or application of a medicinal product in accordance with the instructions given in the summary of product characteristics, and states that the reconstitution of medicinal products in health care establishments is not harmonised throughout Europe.
The resolution highlights that medication errors, including those involving the reconstitution of a medicinal product into a dosage form that is ready to be used or administered to a patient, and quality defects associated with inappropriate reconstitution, have serious implications for patient safety. It states that the quality of reconstituted medicines in healthcare centers should ideally be the same, regardless of where reconstitution takes place, but in real practice risks are greater when reconstitution is carried out in clinical areas. Then, it encourages healthcare establishments to ensure that parenteral medications are properly reconstituted through the preparation in the hospital pharmacy or by purchasing ready-to-administer products. Nevertheless, as capacity is generally not available to allow this, the reconstitution considered to be low risk can be done on the wards. The use of a risk assessment approach is recommended to identify high-risk products that should be reconstituted in the pharmacy and which could be safely reconstituted in clinical areas with appropriate risk-reduction measures26.
Several European countries have developed practical guidelines and assessment tools to improve the reconstitution process in accordance with the recommendations of these reports, with the aim of improving patient safety in hospitals; these include the United Kingdom, the Netherlands and Spain27–30. However, these efforts have been focused primarily on ensuring the implementation of best practices for injectable preparation in clinical areas instead of promoting the preparation of injectable medications in the pharmacy. For this reason, although the publication of these resolutions was an opportunity to promote aseptic preparing units in hospital pharmacies in Europe, these units have been developed to a very limited extent. Challenges of implementing CM/Res(2016) in European hospitals include additional costs for clean rooms, clean room technology and monitoring, qualified staff recruitment, changes on medicines legislation and complexity of the process and control related risks31.
Experience in England and recent proposals to improve preparation and administration of injectable medicinesA death from a potassium chloride concentrate injection error in England was published by Whitelaw in 197432. This death and others from potassium and other injectable medicines prompted the publication of the Breckenridge report providing guidance on addition of drugs to intravenous infusion fluids in 197633. The report included the following recommendation: “The addition of drugs to intravenous infusion fluids is an aseptic pharmaceutical procedure which should ideally be carried out in appropriate environmental conditions under the direct control of a pharmacist. However, because this procedure must sometimes be undertaken immediately prior to administration, it is often carried out on the wards by medical or nursing staff. The pharmacist should therefore carefully examine the possibilities of providing a dispensing service for the necessary drug-infusion mixtures which would enable these to be aseptically prepared in the pharmacy. This is particularly important if the contents of more than one vial or ampoule are to be added to the infusion fluid”. Sadly, the guidance was not fully implemented in hospitals in England and more incidents of deaths and serious harms from potassium chloride and other injectable medicines continued to be reported34–37.
In 2007 reviewing data from the new National Health Service (NHS) National Reporting and Learning System (NRLS) and published research, Safety Alert 20 on Safer Use of Injectable Medicines was issued27. In this publication it was noted that the incidence of errors in prescribing, preparing and administering injectable medicines is higher than for other forms of medicine. This was evidenced by incident reports to the NRLS and research studies. It was again recommended that ready-to-administer or ready-to-use injectable products of standard strength should be provided, that will minimise risks when preparing and administering injectable medicines.
Since 2007, the National Patient Safety Agency and successor organizations responsible for issuing patient safety alerts to the NHS in England have issued many alerts associated with the unsafe use of injectable medicines, in situations where the risks could be reduced by the provision of ready-to-administer or ready-to-use injectable medicines and the prospective review by a pharmacist of the prescription before preparation and use38–40.
In 2019, Lord Carter of Coles was commissioned by the Department of Health to review the quality, safety and resilience of the NHS hospital pharmacy aseptic services in England. In the introduction to his report, entitled Transforming NHS Pharmacy Aseptic Services in England, Lord Carter observed that these services are “an unsung hero“ and that by transforming these services, the NHS has the chance to deliver better clinical outcomes, an improved patient experience and deliver considerable productivity gains. It presents one of the best opportunities to improve patient care and deliver significant savings13.
In March 2020, the draft report was largely complete and focused on nursing staff savings through the use of ready-to-administer injectable medicines. However, afterwards, in light of the experience during the COVID-19 first wave pandemic, the report was reframed in order to reflect lessons learned and how they effects aseptic medicines, specifically to:
- •
Recognise the positive impact of ready-to-administer injectable medicines on critically ill patients.
- •
Recognise the need to embed these changes in NHS clinical practice.
- •
Explore the opportunities to employ ready- to-administer medication in the home or in non-acute settings to relieve pressure on hospital beds.
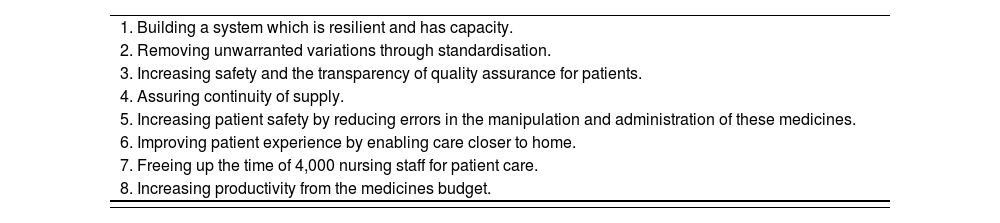
The report states that during the pandemic clinicians prescribed standardised concentrations and volumes of injectable medicines. Aseptic units have been able to deliver these ready-to-administer standardised injectables to treat critically ill COVID-19 patients in hospitals, and nursing staff expressed their preference for these ready-to-administer medicines and their desire to continue to use them going forward. Consequently, in the pandemic recovery period it had become clear that the NHS must make additional efforts to increase the number of ready-to-administer medicines. The identified benefits from implementing the report proposals are summarised in table 1.
Expected benefits by transforming NHS pharmacy aseptic services in England13.
| 1. Building a system which is resilient and has capacity. |
| 2. Removing unwarranted variations through standardisation. |
| 3. Increasing safety and the transparency of quality assurance for patients. |
| 4. Assuring continuity of supply. |
| 5. Increasing patient safety by reducing errors in the manipulation and administration of these medicines. |
| 6. Improving patient experience by enabling care closer to home. |
| 7. Freeing up the time of 4,000 nursing staff for patient care. |
| 8. Increasing productivity from the medicines budget. |
The report proposes a fundamental change in the operating model, to enable the NHS to move from small over-stretched pharmacy aseptic units to a national network of regional hubs with the capacity to produce high volume products on an industrialised scale using automated systems in offhospital sites. Achieving this will require an industrial step change in production, using advances in technology including automation, which will need considerable investment, but will yield significant returns in quality and cost. It is estimated that this model can increase the current provision of 3.4 million doses in English hospitals to over 40 million doses and this can release the time of over 4,000 whole time equivalent nurses each year who would be making up these doses on wards.
In England it has also been recognised that drug administration errors are the most common type of intravenous error and that more action is required to standardise policies and procedures between NHS hospitals to improve intravenous infusion safety18,41. Smart infusion devices with dose error reduction software (DERS) when implemented effectively would minimise wrong infusion rate errors42,43. However, although the aim of smart infusion pumps is to improve patient safety, there are barriers and challenges to do this leading sometimes to infusion errors due to workarounds, poor workflow, and technology limitations44,45.
The Healthcare Safety Investigation Branch (HSIB) funded by the Department of Health in England, recently conducted an Investigation into the procurement, usability and adoption of 'smart’ infusion pumps46. This investigation focused on understanding the challenges involved in introducing smart infusion pump technology within NHS hospitals and reviewed the safety risks associated with implementing this technology, leading to safety recommendations about how these risks need to be managed.
The investigation identified that in England there is currently no agreed national drug library for use in NHS hospitals. Additionally, there are no national guidelines or standards on how to implement drug libraries. Using smart pumps requires staff to be trained in the use of a drug library and DERS. This is a complex and often unfamiliar task for many staff. Besides, the infrastructure needed to implement smart pump technology requires the use of software to upload the drug library to the smart pumps, download data logs associated with usage (including alerts where DERS has prevented an “error”), and monitor the status of each smart pump in the system. Smart pumps need to be connected to a hospital's IT network and require specialist staff.
Recommendations for action included that the NHS develops an agreed specification that defines an open standard format for the sharing of event log data, thus allowing DERS to be evaluated to establish patient safety benefits. In addition, that validated national drug libraries for smart infusion pumps are developed and that training (possibly mandatory) is required for clinicians and pharmacists on the use of safety critical devices within a hospital.
Many of the findings and recommendations of HSIB report have also be found in other European publications. A European expert panel in 2013 concluded that the use of DERS is mainstream in the United States but in Europe it is with enthusiasts only, and that the first step in the implementation of smart pumps and drug libraries is the introduction of standardised drug concentration and volumes. Ideally, pump manufactures should produce template drug libraries, and if possible provide technical support to help users to customise them. Networked connectivity for smart pumps is essential47.
In a recent literature review of the role of the pharmacist in smart infusion pumps, the authors found two predominant themes for the creation of a drug library: using a multidisciplinary team, consisting of a pharmacist, nurses and physicians, and standardisation of infusions48. The pharmacist had the main role of creating a drug library. The presumed reason for this is that, as drug experts, pharmacists had a critical role in ensuring that an accurate and safe drug library was built, which would be of the utmost importance when it comes to patient safety.
DiscussionAs healthcare continues to develop to meet the needs of patients, the use of injectable medicines increases, with more doses prescribed, prepared, administered and monitored. Two important practices to support the safe use of injectable medicines, namely pharmacy aseptic preparation services to provide ready-to-administer injectable medicines and the use of smart pumps with DERS have generally had limited implementation in European hospitals compared to those in North America.
In the past, hospital pharmacists in Europe have presented information about the high rate of medication errors and the absence of good manufacturing practices on wards as reasons why the preparation of injectable medicines should be transferred to hospital pharmacy services. Although this safer practice has been supported by national and European reports, this transfer has not occurred to any great extent. Barriers include the additional cost of the aseptic environment, equipment, quality assurance, additional logistics required to supply and store aseptically prepared products, and the cost and difficulty of recruiting additional aseptic services staff.
The full implementation of smart infusion pumps and syringe drivers has been hindered by difficulties in agreeing standard concentrations of infusions, insufficient pharmacy resources to build drug libraries and difficulties in uploading and downloading data to and from smart pumps via hospital WIFI systems.
The COVID-19 pandemic is prompting a re-evaluation of the work of all clinical staff, and the need to reduce unnecessary variation in clinical practices and to have systems in place which have resilience and capacity. It has highlighted the significant time that nurses spend preparing injectable medicines. This work takes them away from direct patient care at a time when many European countries have insufficient nursing staff to meet demand. These concerns have risen to the top of hospital and national agenda's for action.
Expansion of hospital pharmacy aseptic preparation services from only focusing on injectable medicines that cannot be prepared in clinical areas (e.g. total parenteral nutrition, cancer chemotherapy and small number of specialist products), to a wider range of products requiring a much larger number of doses (e.g. antibiotics and error prone products) would save significant amounts of nursing time, as well as allow standardisation of product ranges and provide more resilient systems with capacity. These new services would improve product quality and help minimise preparation errors. Other important benefits include enabling more injectable medicines to be administered to patients at home.
Proposals from the Carter report in England recommend moving from small overloaded aseptic pharmacy units to a national network of regional centers with the capacity to produce high-volume products on an industrial scale using automated systems. This additional step has been taken to our knowledge, at least in the Netherlands where a center of this type has already been created and owned by several hospitals as shareholders49.
If the expansion of aseptic services was also linked to standardizing injectable medicines procedures, drug libraries and drug administration using smart infusion devices this would also help minimise drug administration errors.
When change is proposed, there are always concerns that the staff group previously undertaking the role is at risk of losing their skills. To avoid this, nurses’ knowledge and ability to prepare injectable medicines should be maintained. This could be achieved by identifying small numbers of injectable medicines, e.g. some first doses, that could continue to be prepared by nursing staff and providing standardised training for qualified nursing staff and students on safe preparation and administration of injectable medicines. Pharmacy services should play a larger role in developing, delivering and assessing the effectiveness of this training.
The introduction of larger numbers of aseptically prepared injectable medicines may introduce new types of errors. For example doses could be omitted or delayed if there are delays in delivering enough ready-to-administer products to clinical areas in a timely manner. Most ready-to-administer products require refrigerated storage in clinical areas, and these products could be wasted if they are not stored correctly or they pass their shorter expiry dates. There is also increased risk of mis-selection errors of different ready-to-administer products if the labelling and packaging of these products look very similar. Aseptic units should make judicious use of colour and design to help differentiate injectable products. Plans for expanded aseptic services should include thorough risk assessment to identify risks and mitigating actions to minimise these risks. These expanded aseptic services should be piloted to identify and manage additional risks before they are offered to all clinical areas.
In conclusion, there are new opportunities to expand the role of hospital pharmacy departments in Europe to deliver more extensive services for injectable medicines. The COVID pandemic has stimulated hospitals to place greater value on nurses time and on resilient systems to assure capacity, continuity and quality. These factors are in addition to the need to further improve patient safety by reducing medication errors. A re-examination of how injectable medicines are prepared and administered in European hospitals would be very timely.
FundingNo funding.
Conflict of interestsNo conflict of interest.