Medication reconciliation is an essential process in the care of critically ill patients, ensuring that patients' chronic medication is adapted to the patient's clinical situation and administered safely during hospitalisation. Given the profile of the patient admitted to a critical care unit (ICU), this becomes even more relevant. Reconciliation minimises possible medication errors and adverse effects, improving safety in the critically ill patient.
MethodsThe project, carried out between 2021 and 2024, was led by the FarMIC (Pharmacists in Intensive Care Medicine and Critical Care) and RedFaster (Pharmaceutical Care in Emergencies) groups of the Spanish Society of Hospital Pharmacy (SEFH), and included: selection of the drugs, review of the available literature and previous conciliation guidelines in similar areas of application, preparation of the drug information with the recommendations issued by the working group, the review of the same and the development of the mobile application.
ResultsIn October 2024, the app ‘Conciliation Guide for Critically Ill Patients®’ was published, available free of charge for iOS and Android. It provides a drug index with detailed information on medication reintroduction schedules, routes of administration, monitoring, and drug-specific considerations. In addition, the tool includes information on withdrawal syndromes, drug-drug interactions with the usual ICU drugs and hazardous drugs information according to the NIOSH list.
ConclusionsThis app facilitates pharmacotherapeutic reconciliation process in the ICU, supporting healthcare professionals in making personalised decisions. Its use can optimise patient safety, reduce adverse events and improve critical patient care. Finally, this tool reinforces the role of the clinical pharmacist in the ICU, who must lead this process in all care transitions and adapt it to the clinical situation of the patient.
la conciliación de la medicación es un proceso esencial en la atención de pacientes críticos, que garantiza que la medicación crónica de los pacientes sea adaptada a la situación clínica del paciente y administrada de forma segura durante su hospitalización. Dado el perfil del paciente ingresado en una unidad de críticos (UCI), adquiere una relevancia aún mayor. La conciliación minimiza posibles errores de medicación y efectos adversos, mejorando la seguridad en el paciente crítico. El objetivo es exponer el desarrollo de una app móvil de la Guía de conciliación farmacoterapéutica para su uso en la UCI, proporcionando a los profesionales sanitarios recomendaciones basadas en evidencia científica para la conciliación de la medicación en esta población.
Métodosel proyecto, realizado entre 2021 y 2024, fue liderado por los grupos FarMIC (Farmacéuticos de medicina intensiva y pacientes críticos) y RedFaster (Atención farmacéutica en urgencias) de la Sociedad Española de Farmacia Hospitalaria (SEFH), e incluyó: la selección de los fármacos a analizar, la revisión de la bibliografía disponible y las guías de conciliación previas en ámbitos similares de aplicación, la elaboración de las fichas de medicamentos con las recomendaciones emitidas por el grupo de trabajo, la revisión de las mismas y el desarrollo del aplicativo móvil.
Resultadosen octubre de 2024 se lanzó la app Guía de conciliación en pacientes críticos®, disponible gratuitamente para iOS y Android. Ofrece un índice de medicamentos con información detallada sobre cronogramas de reintroducción de la medicación, vías de administración, monitorización y consideraciones específicas de cada fármaco. Además, la herramienta incluye información sobre los síndromes de retirada, las interacciones medicamentosas y los medicamentos peligrosos según la lista NIOSH.
Conclusionesesta app facilita la conciliación farmacoterapéutica en la UCI, apoyando a los profesionales sanitarios en la toma de decisiones personalizadas. Su uso puede optimizar la seguridad del paciente, reducir los eventos adversos y mejorar la atención de los pacientes críticos. Finalmente, esta herramienta refuerza el papel del farmacéutico clínico en las UCI, que debe liderar este proceso en todas las transiciones asistenciales y adaptarlo a la situación clínica del paciente.
The quality of pharmacotherapy and patient safety form part of the overarching principles and quality standards of the Spanish Law on Cohesion and Quality of the National Health System (Ley De Cohesión Y Calidad Del Sistema Nacional De Salud).1 Preadmission medication reconciliation is a key strategy for enhancing the quality of pharmacotherapy. Other actions include medication reconciliation at transition of care (e.g. at admission), patient transfer, or hospital discharge.2 These strategies help ensure that patients continue receiving their outpatient medications at the correct dose, via the appropriate route, and with a frequency adjusted to their clinical condition.
Medication reconciliation is defined as the formal, standardized process of obtaining a complete list of the current medication a patient is taking to compare it to newly ordered medications, and analyze and solve any discrepancies. Reconciliation errors are any unintentional and clinically unjustified discrepancies, usually occurring as a result of a misunderstanding or a communication error.3 The reconciliation process involves three steps: gathering a complete list of the patient's chronic medication and verifying active medication orders; comparing and detecting apparently unjustified discrepancies that may require further clarification; receiving clarifications from the prescriber; documenting any changes, and recording a list of the reconciled medication.4
The Joint Commission (JC) acknowledges that reconciliation errors compromise the safe use of medications. Hence, the JC identifies the accurate and complete reconciliation of medication as a key safety approach to meeting medication use standards.5 One of the main duties of the clinical pharmacist includes performing medication reconciliation by carefully reviewing the list of patient's medications, evaluating their medical record, and through direct interviews with the patient. This activity has been proven to be effective in preventing and reducing medication errors and side effects in patients admitted to intensive care units (ICUs) or resuscitation units.6,7
Medication errors are especially relevant in the setting of critically ill patients, where medications are a major therapeutic resource. A study conducted in a Spanish clinical-surgical ICU revealed discrepancies between home medication and medication orders at ICU admission in 62% of cases, of which 48% stemmed from reconciliation errors. Of them, 58% were considered category D errors (errors that may cause potential harm to the patient and need monitoring or intervention to preclude harm); and up to 7% were considered F category errors (errors that cause harm and need hospitalization or prolongation of hospital stay).5 According to the Spanish Institute for the Safe Use of Medications (Instituto para el uso seguro de los medicamentos), ICU patients are at an increased risk of experiencing medication-related adverse events, as many of the medications used in the ICU are considered high-risk medications (drugs that, when used inappropriately, increase the risk of causing severe or life-threatening harm to patients) or medications with a narrow therapeutic range8. Other risk factors include the severity and complexity of the patients' conditions and the need for close communication between the different attending physicians.9 In this line, a study assessing discrepancies in medication orders during transition from the ICU to the general ward documented that 20% of reconciliation errors involved a high-risk medication.7 The alterations inherent to critically ill patients may impair oral drug absorption (shock or hypotension resulting in gastrointestinal tract hypoperfusion; use of vasopressor agents; sedoanalgesia; or delayed gastric emptying). Additionally, oral administration (orotracheal intubation, deep sedation, among others) is often not feasible in this setting, and the dose/pharmaceutical form of outpatient medication may need to be adjusted. These challenges lead to a major use of intravenous medications to ensure the bioavailability of the drug.9 The increased sensitivity, hemodynamic instability and varying condition of critical patients make this population more prone to experience medication errors with potentially more severe effects.10 It is worth noting that abrupt home treatment discontinuation may cause withdrawal syndrome, changes in clinical parameters, or even result in a relapse of the disease for which the drug therapy was prescribed.11 Therefore, it is crucial that these medications are identified during the reconciliation process and ordered on a priority basis. The factors described above underline the relevance of reconciling medication in ICUs.
On another note, the rapid development of healthcare technologies in recent years has not only contributed to optimizing healthcare standards but has also significantly improved patient outcomes worldwide. These innovations range from advances in medical devices and remote monitoring apps to the use of artificial intelligence for early diagnosis and the design of personalized therapies. An example is the algorithm designed for detecting patients at a higher risk of experiencing reconciliation errors after ICU discharge.12 In summary, the implementation of clinical data management applications has facilitated a more informed and accurate clinical decision-making. As a result, patients receive more effective treatment plans tailored to their specific needs. A wide array of mobile applications (apps), such as Concilamed or UrfRedFastER, is already available to assist clinicians during the reconciliation process. However, these apps do not always adjust to the clinical setting of critically ill patients.
Access to updated, evidence-based information is crucial for healthcare professionals to appropriately evaluate medication orders in critically ill patients. The display of this information on an easily accessible mobile app will help optimize pharmaceutical care in ICUs, thereby enabling rapid, effective medication reconciliation.
ObjectiveThe objective of this paper is to present the mobile app Guía De Conciliación Farmacoterapéutica Para Pacientes Ingresados En Las UCI (Guide To Medication Reconciliation In ICU Patients) aimed at healthcare professionals involved in the drug therapy process of critically ill patients. This Guide provides recommendations for assessing the risk–benefit of maintaining/discontinuing outpatient medication in routine practice.
MethodsA lead working group (WG) was commissioned to develop the scientific contents of the Reconciliation Guide. The group was composed of Emergency Department and ICU hospital pharmacists from the FarMIC (intensive medicine and critical care pharmacists) and RedFaster (ED pharmacy care) working groups of the Spanish Society of Hospital Pharmacy (SEFH).
The project was developed from January 2021 to October 2024 and involved several stages:
- –
Creation of the Working group: The project was led by the FarMIC Working Group (WG). All members of the FarMIC and RedFaster coordinating WGs were invited to voluntarily take part in the project. The lead WG was finally composed of eight specialist pharmacists and an assistant group of eight pharmacists.
- –
Definition of Guide structure and review criteria: The Guide was structured based on previous guides, including the RedFaster WG Guía De Conciliación Al Ingreso En Urgencias (Guide to Reconciliation at ED Admission)13 and other clinical practice guidelines for the perioperative management of chronic medication in surgery patients.14 Through consensus, the WG selected the variables to be considered for the management of critically ill patients during an acute process. For such an end, based on their individual clinical experience, the panel considered the particular characteristics of critically ill patients. Special attention was paid to the particularities of this population regarding medication reconciliation.
- –
Task assignment and active-substance selection: The WGs reviewed each pharmacotherapeutic group according to the ATC classification (4 digits if the active substance could be grouped into a single medication data sheet). Active substances that are clinically relevant to this population were selected through WG consensus. Infrequently prescribed active substances or those on which scientific evidence is limited were ruled out by simple majority, as they were not applicable to this population.
- –
Literature search: Different data sources including clinical and pharmacological information platforms were searched, namely: UpToDate, Drugdex-Micromedex®, and Lexicomp®. The search was extended to the summary of product characteristics (SmPC) of each drug, available at the Medicine Online Information Center (CIMA) of the Spanish Agency for Medicines and Medical Devices (AEMPS). An evaluation was performed of the alternative routes of administration of each medicinal product, as critically ill patients frequently exhibit poor oral intake tolerance or restricted availability of enteral or parenteral access, and an alternative route of administration of outpatient medication may be needed. For recommendations about alternative routes, drug bioavailability and biohazard were considered, with the latter being based on the NIOSH list. This way, information is provided on the hazards associated with the handling and administration of these medications according to the route of administration. Additionally, a review was performed of the scientific evidence available on the tolerability and dependence potential of ICU medications to determine the risk for developing a withdrawal or rebound syndrome after treatment discontinuance. Additional recommendations were included to support clinicians in making informed decisions about restarting a drug therapy based on the patient's clinical condition. Hence, information was included concerning the interactions, comorbidities or clinical and analytical abnormalities that should be taken into account when ordering a particular medication. Finally, information is also offered about the clinical and analytical monitoring criteria to be applied.
Considering the points discussed above, a recommendation was issued that reconciliation should be performed both at ICU admission once the patient is hemodynamically stable, and at ICU discharge.
- –
Drafting of a preliminary document: This task was performed by the principal investigator.
- –
Review and validation of medication data sheets: The rest of the members of the coordinating groups and the FarMIC working group were invited to take part in this step of the process. Each medication was subject to a peer-review conducted by a panel of 29 specialist pharmacists.
- –
Review and drafting of the final document: This task was performed by the principal investigator.
- –
Development and implementation of the mobile app: An external company was commissioned to develop the app software for smartphones and tablets.
- –
Validation: The content of the app was validated by all WG members.
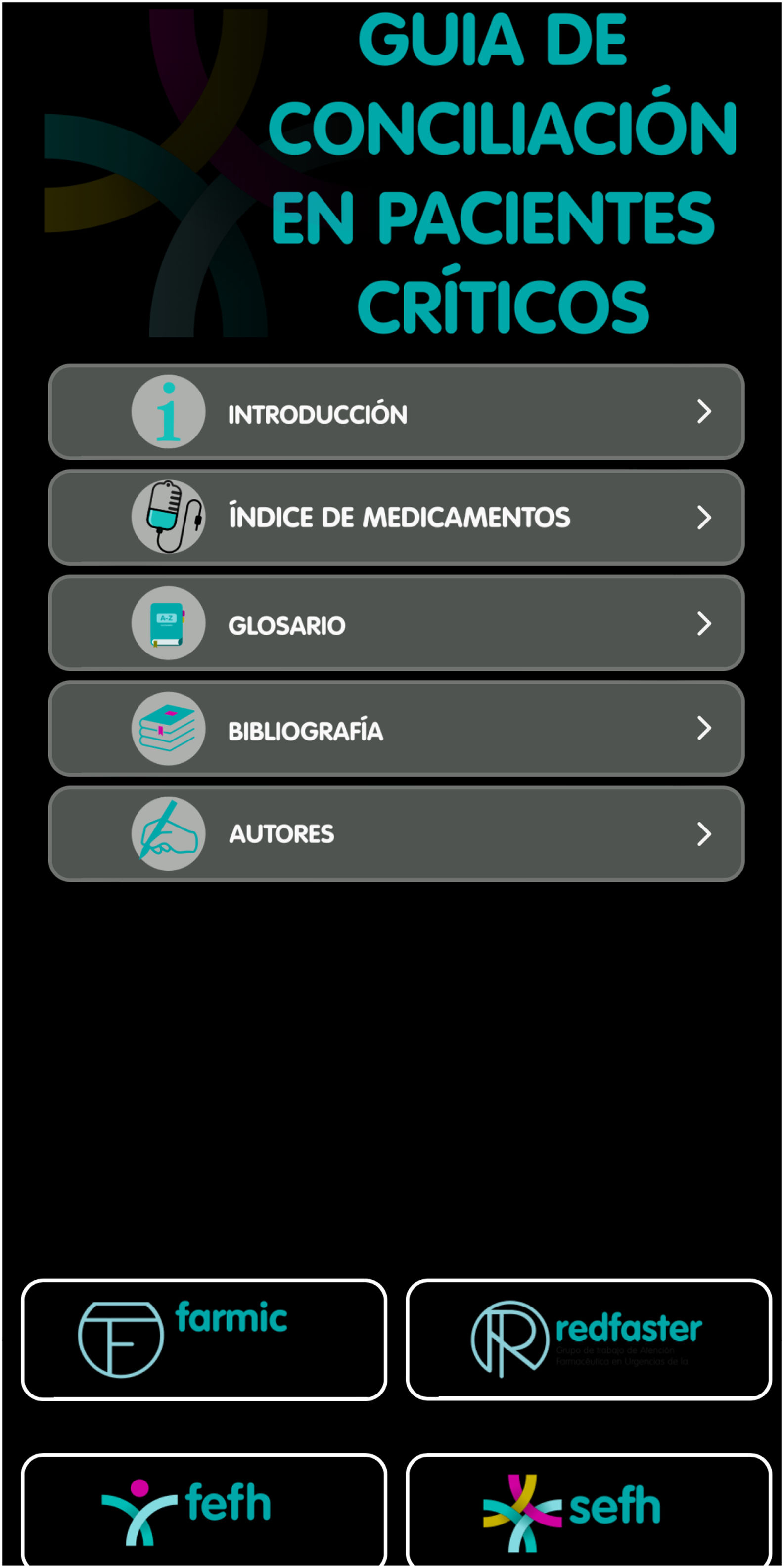
The app was released in October 2024 after the name “Guía De Conciliación En Pacientes Críticos®” (Guide to Reconciliation in Critically Ill Patients) and is currently available for iOS and Android systems. This app can be downloaded free of charge as a mobile app from App Store and Google Play and is accessible to all users. No login is required.
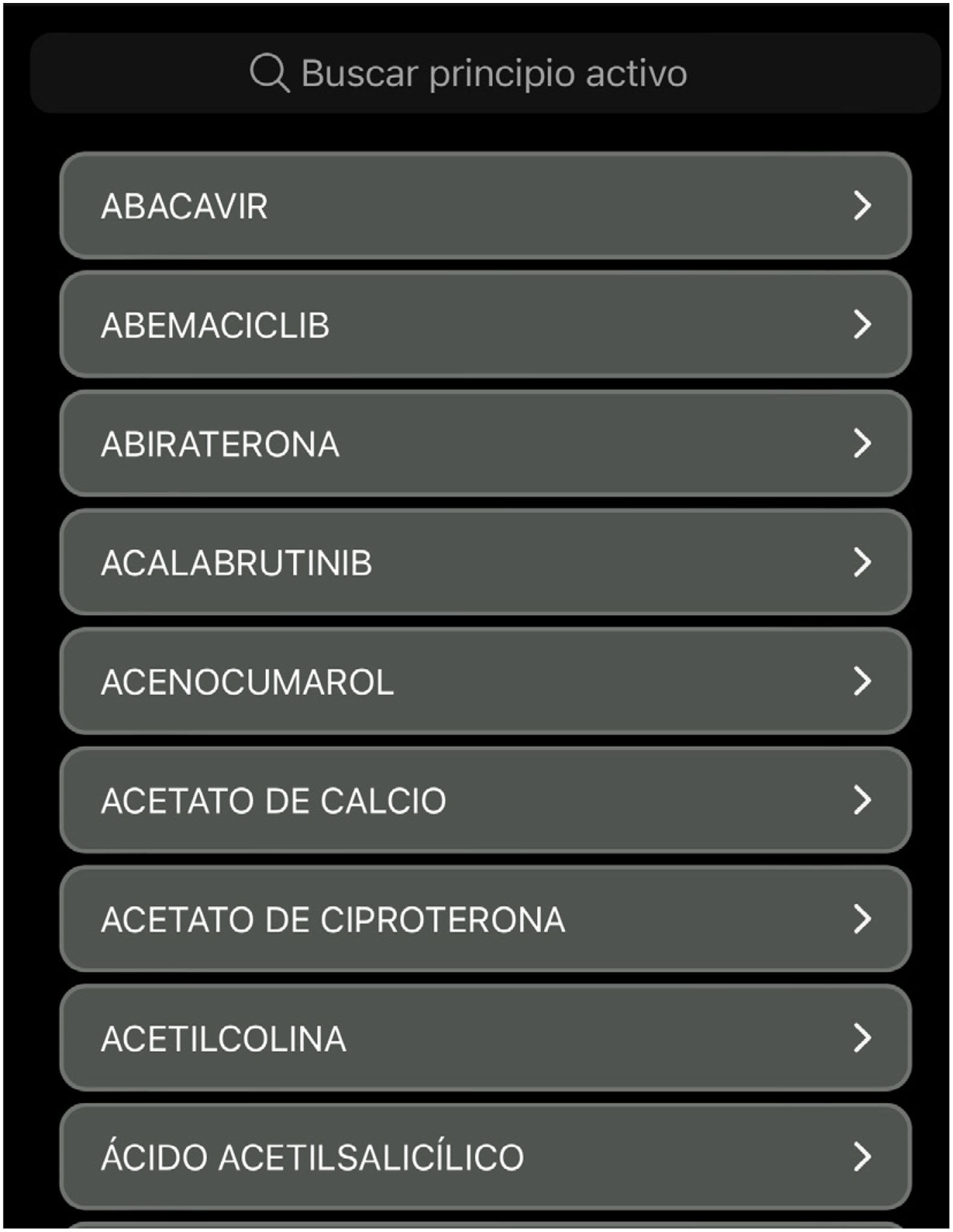
This app features a homepage that provides access to a brief introduction, a glossary, a list of references, and author names. It also displays an index and a tool for searching medications by the active substance that provides direct access to individual data sheets.
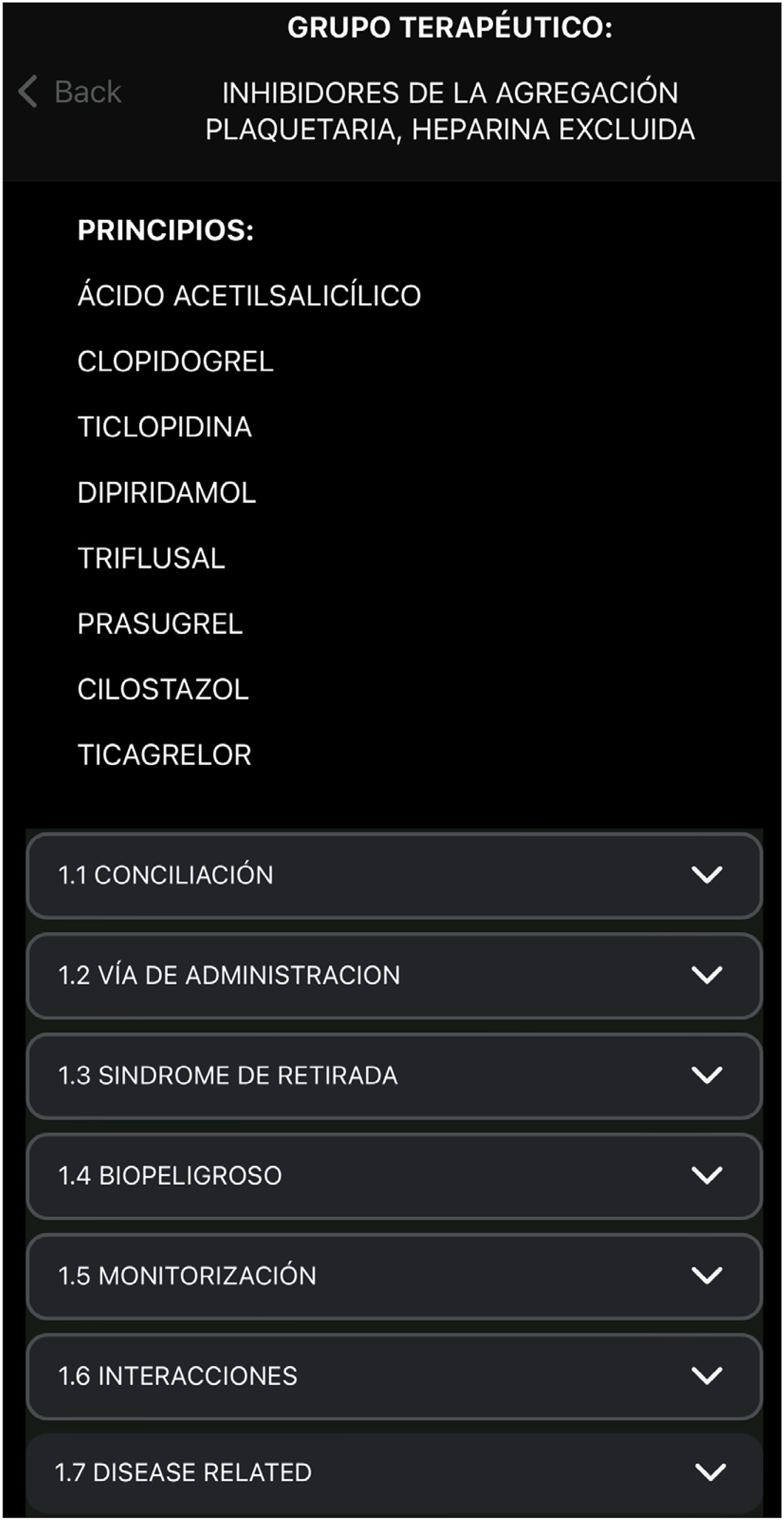
The items considered were described according to the following structure:
- –
Pharmacotherapeutic group.
- –
Active substance.
- –
Timing of Reconciliation: The timing for restarting a medication was determined on the basis of its urgency, based on the risk–benefit of discontinuing the medication. Groups were defined as follows:
- •
“At admission”: Medications that should be prescribed at ICU admission.
- •
“Upon recovery of hemodynamic stability”: Medications that do not need to be restarted at the acute phase but should be restarted at some point during the ICU stay, once hemodynamic stability has been restored.
- •
“At discharge”: Medications that do not need to be restarted at the acute phase during the ICU stay but upon patient discharge to the general ward.
- •
- –
Route of administration: Routes of administration were recorded according to the pharmaceutical forms available for each medication. Recommendations for adapting the route to the patient's clinical status were established, including recommendations for administration via a nasogastric/nasojejunal tube. The app also addresses compatibility with concurrent enteral nutrition and specifies the availability of intravenous, intramuscular, or subcutaneous formulations. It also provides information about bioavailability and dose equivalence across the different pharmaceutical forms. Guidance is provided on whether special delivery systems are required for administration, such as light-protective opaque devices or compatibility with specific materials (e.g., PVC). Finally, the section covers considerations for restarting medication when oral tolerance is adequate.
- –
Withdrawal syndrome: yes/no. Special considerations were reviewed according to whether abrupt discontinuance of a medication could result in a rebound effect or cause undesired adverse events.
- –
Hazardous drugs: classification based on the NIOSH list.15 Special recommendations for medication handling were included.
- –
Monitoring: potential adverse events requiring special monitoring, or abnormalities that should be considered during use in the ICU.
- –
Clinically relevant drug-to-drug interactions with common or ICU-specific drugs: amiodarone, cisatracurium, clevidipine, dexmedetomidine, dobutamine, dopamine, fentanyl, furosemide, insulin, isoprenaline, ketamine, labetalol, levosimendan, lidocaine, midazolam, morphine, nitroglycerin, norepinephrine, propofol, remifentanil, rocuronium, terlipressin, and urapidil.
- –
Associated-disease considerations: specific medical or clinical considerations to be taken into account in relation to a disease when starting a treatment or administering a drug.
Recommendations were reviewed and included for 568 drugs from 192 pharmacotherapeutic groups.
Subsequently, Syscel Solutions S.L. developed the software and app interface (Figs. 1–3). The principal investigator verified the preliminary app version to validate its format, visual design, and final content.
Finally, it was decided that the scientific content would undergo monitoring, maintenance and updating on an annual basis.
DiscussionWe developed an easy-access mobile app containing reliable information about medication reconciliation in critically ill patients. This invaluable tool will assist ICU healthcare professionals in decision-making.
One of the goals of the 2020 SEFH working group was achieving that 80% of Hospital Pharmacy Departments got involved in the development of a standardized outpatient medication reconciliation process both at admission and at discharge.16 This project forms part of the SEFH strategic lines, as it helps healthcare professionals to correctly perform medication reconciliation on an individualized basis. Additionally, this app contributes to improving patient safety in the ICU.
In this line, the pharmacists involved in multidisciplinary teams managing critically ill patients should lead the reconciliation schedule and prepare the pharmacotherapeutic history of each patient.17 The involvement of hospital pharmacists in the management of ICU patients has demonstrated to significantly optimize drug therapies and reduce medication errors, adverse events, and mortality in these patients.18–20 However, despite the evidence available on the major role of pharmacists in the ICUs, experience in this field is still limited in Spain, with a median of five years of experience in 2019. Pharmacy staffing is both limited and variable (30.8 beds per pharmacist) with one pharmacist covering an average of 30.8 beds. In up to 93.3% of cases, the pharmacist is assigned to the ICU on a part-time basis, with a mean of 2.7 ± 1.7 h a day devoted to the ICU.21 Hence, this tool contributes to optimizing pharmacist activity in the ICU.
Timely medication reconciliation should be considered a priority objective and a shared responsibility of all healthcare professionals. Reconciliation should be integrated into all routine clinical activities, including initial patient assessment at admission; ward rounds; new medicine orders; nursing shift changes; pharmaceutical validation; patient education; transfers of care; and preparation of the discharge summary.17 Hence, this app not only emerges as a valuable tool for clinical pharmacists but it will also facilitate decision-making among healthcare professionals involved in the management of critically ill patients.
Some apps are already available to facilitate medication reconciliation and perioperative management of outpatient medication in patients undergoing elective surgery (Conciliamed®) or in Emergency Departments (UrgRedFastER®). However, this is the first mobile app to provide recommendations for adjusting outpatient medication in critically ill patients. This app also offers distinctive information such as when to restart outpatient medication with respect to ICU admission. Other recommendations are provided about routes, clinically relevant interactions with perfusion drugs frequently used in the ICU, clinical parameters, and adverse events. Finally, the app details the considerations to be taken into account when starting or discontinuing a drug therapy, which is an innovative feature not available in previous apps.
A limitation of this project is that app contents were not validated by ICU physicians, nurses, ICU patients, or caregivers, but only by hospital pharmacists. In addition, the information provided is only available in Spanish. Moreover, future efforts should be focused on integrating all this information into hospital information systems.
Future updates will involve an annual review and maintenance of the scientific content of the app. Additionally, the impact of the app on users and its usability in routine clinical practice will be assessed.
In conclusion, this mobile app provides recommendations for 568 drugs regarding the benefits and risks of maintaining or discontinuing outpatient medication. This tool is intended for healthcare professionals involved in the management of ICU patient pharmacotherapy and is aimed at streamlining the review of chronic medications during ICU stay. Designed for clinical pharmacists and other healthcare professionals, this accessible tool offers decision support for individualized medication reconciliation in critically ill patients.
CRediT authorship contribution statementMaría Martín Cerezuela: Conceptualization. Fernando Becerril Moreno: Conceptualization. Jesús Ruiz Ramos: Data curation, Conceptualization. Ana de Lorenzo Pinto: Formal analysis, Data curation. Esther Domingo Chiva: Conceptualization. Marta Valera Rubio: Investigation. Irene Aquerreta González: Validation, Conceptualization. Carla Bastida Fernández: Conceptualization. Tatiana Betancor García: Conceptualization. Sara Cobo Sacristán: Conceptualization. Sara Ortiz Pérez: Conceptualization.
AuthorshipAll authors are members of the SEFH FarMIC and RedFaster Working Group. All authors contributed to study conception and design, devised the main conceptual ideas and reviewed the project. María Martín Cerezuela, Fernando Becerril Moreno, Luis Pérez de Amezaga Tomás, Jesús Ruiz Ramos, Ana de Lorenzo Pinto, Laura Doménech Moral, Amaia Egüés Lugea and Marta Albanell Fernández performed the literature search and prepared the scientific content. María Martín Cerezuela and Luis Pérez de Amezaga Tomás took the lead in writing the manuscript. All authors provided critical feedback and approved the final version of the mobile app and the manuscript for publication.
FundingThis project was financed by the Grants for Research Projects and Professional Development promoted by the Working Groups of the Spanish Society of Hospital Pharmacy called by the Spanish Foundation of Hospital Pharmacy in the 2022–2023 call.
The authors declare no conflicts of interest associated with this publication.