This study is the first part of the MEDPAIN project “Update of analgesic parenteral admixtures: studies of use, compatibility and stability”, and its goal is to develop a national map about the use of analgesic parenteral admixtures in healthcare settings.
MethodsObservational study, based on a survey aimed at Spanish hospital pharmacists, during the period December 2020 – April 2021. The questionnaire was designed in the RedCap® platform and disseminated through the Spanish Society of Hospital Pharmacy distribution list. An analgesic parenteral admixture (AM) was defined as the combination of two or more drugs, with at least one of them being an analgesic. The same combination of active ingredients, at different concentration and/or administered by different routes, was considered as a unique AM in this study. Some registered endpoints were related to the characteristics of the healthcare settings participating in the study, and others were related to the AM, such as drugs, doses and concentration range, route of administration, frequency of use, indication and type of patient (adult/pediatric) and where they are prepared.
ResultsA total of 67 valid surveys from healthcare settings of 13 Spanish Autonomous Communities were received. They reported 462 AM. Every healthcare center informed an average of 6 AM (ICR p25-p75 = 4.0–9.0). Most of the reported mixtures were used in adults (93.9%) at hospital settings (91.8%), and they were mostly protocolized and frequently used. The 21.4% of them were compounded at the Pharmacy service. The AM included 26 different drugs, with opioid analgesics being present at the 87.4% of them. Midazolam was the most usual adjuvant drug. According to the definition of AM in this study, there were finally 137 different combinations mainly with two drugs (40.6%), but also with three (37.7%), four (15.2%) and five ingredients (6.5%).
ConclusionIn conclusion, this study reveals the wide variability in current clinical practice and shows which are the most used analgesic parenteral admixtures in our country.
Este estudio corresponde a la primera etapa del proyecto MEDPAIN “Actualización de mezclas analgésicas por vía parenteral: estudios de utilización, compatibilidad y estabilidad”, y tiene por objetivo la elaboración de un mapa a nivel nacional del empleo de mezclas analgésicas en hospitales y centros sociosanitarios.
Material y métodoEstudio transversal, basado en una encuesta dirigida a farmacéuticos hospitalarios, durante el período diciembre 2020-abril 2021. Se diseñó un cuestionario multirrespuesta en la plataforma RedCap® para su difusión a través de la lista de distribución de la Sociedad Española de Farmacia Hospitalaria. Se definió mezcla analgésica como la combinación de dos o más principios activos, de los cuales al menos uno es analgésico. Una misma combinación de fármacos a distintas concentraciones, o administrada por diferentes vías, se consideró una misma mezcla a efectos de este estudio. Se registraron variables relacionadas con el centro participante y otras relacionadas con las mezclas analgésicas: composición farmacológica de la mezcla, vía de administración, frecuencia de uso, indicación, tipo de paciente (adulto/pediátrico), ámbito en el que se utiliza (hospitalario/domicilio) y lugar de preparación.
ResultadosSe recibieron un total de 67 encuestas válidas (55,4%) procedentes de 13 Comunidades Autónomas. Los 67 centros sanitarios comunicaron un total de 462 mezclas analgésicas. La mediana de mezclas informadas por centro participante fue de 6 (RICp25-p75 = 4,0-9,0). La mayoría de las mezclas notificadas se utilizan en adultos(93,9%) y en el ámbito hospitalario(91,8%); mayoritariamente se trata de mezclas protocolizadas y de uso frecuente. El 21,4% se preparan en el servicio de Farmacia. En las mezclas descritas aparecen 26 fármacos distintos; predominan los analgésicos opioides, presentes en el 87,4% de las mezclas. El fármaco coadyuvante más frecuente es el midazolam. Teniendo en cuenta únicamente las combinaciones distintas, se encontraron finalmente 137 mezclas diferentes. Aunque la mayoría de las mezclas estaban compuestas por dos fármacos (40,6%), también se han registrado mezclas de tres (37,7%), cuatro (15,2%) y cinco componentes (6,5%).
ConclusiónEn conclusión, este estudio permite confirmar la variabilidad en la práctica clínica actual y mostrar cuáles son las combinaciones de fármacos más utilizadas en nuestro país.
Pain in its different forms continues to be a prevalent entity in hospitalized patients and its correct management remains a challenge for health staff.
The complex etiopathogenesis of pain, which involves large numbers of neurotransmitters, has led to the use of multimodal analgesia as a standard of clinical practice. This approach comprises the concomitant use of drugs with different mechanisms of action and/or different routes of administration, and can even be combined with nerve blocks with local anesthetics or other interventional techniques1. One of the main advantages of using multiple drugs in combination is to reduce the need for high doses of opioids.
On the other hand, pain in the pediatric population has often been underestimated and/or inadequately treated. In general, the same drugs can be used as in the adult patient with consequent dose adjustment and preferably administered in a fixed schedule. Multimodal analgesia is also indicated in children; patient-controlled analgesia (PCA) can be used in children of at least 6 years2.
Among the drugs used, classic opioid analgesics (e.g. morphine, fentanyl, methadone) and minor opioids (e.g. tramadol)—given by different routes of administration—continue to play a fundamental role in the control of moderate to severe pain3. Nonsteroidal antiinflammatory drugs (NSAIDs) and paracetamol are useful as single analgesics in minor surgical procedures and in combination to reduce the dose of opioids required after major surgery, as well as to treat mild to moderate pain of other origin4. In Spain, parenteral options available include dexketoprofen, diclofenac (intramuscular only), ibuprofen, ketorolac, metamizole, and paracetamol.
Local anesthetics, such as bupivacaine, levobupivacaine, or ropivacaine, are frequently used as adjuvant drugs in perfusions for epidural PCA, in perineural block mixtures for postoperative pain management, and in implantable intrathecal devices. Other drugs, such as ketamine or clonidine, also play an important role in multimodal analgesia5,6.
In addition, nausea and vomiting are frequent in patients with postoperative pain and in some cancer patients, so it is relatively common to include antiemetic drugs in the analgesic guidelines. Similarly, antispasmodic drugs are used when patients require them or benzodiazepines when a sedative effect is needed in addition to analgesia.
In short, many possible combinations of drugs can be found in the analgesic guidelines for parenteral pain treatment.
Although it is the case that there are clinical practice guidelines on different types of pain management, such recommendations are usually of a general nature. For example, although the American Postoperative Pain Management Guidelines recommend the use of multimodal analgesia, they also indicate that the drugs used will depend on the patient, the healthcare centre, and the type of surgery7.
Apart from the use of multiple drug combinations, clinical practice involves the added challenge of these drugs frequently being added to a diluent in the same container for their combined administration. There are no ready-to-administer analgesic combinations on the market, and so the preparation of these mixtures is the responsibility of healthcare staff. This can be conducted in nursing units just before administration or centralized in the pharmacy services as standardized mixtures with an adequate shelf life.
In any case, it should be noted that before mixing 2 or more drugs in solution, it should be known—in addition to the desired effect—whether they are compatible with each other and stable in the chosen diluent, at least during the time needed for their preparation and administration. The joint administration of physicochemically incompatible drugs can have negative effects on the patients' health due to a lack of therapeutic effect as well as toxicity8.
Thus, among other aspects, subjectivity in the assessment of pain, the various pathophysiological mechanisms involved, and the diverse clinical situations of the patients, make pain management an extremely complex task with great variability in clinical practice, all of which means that there is a lack of knowledge concerning the analgesic mixtures that are actually being used in Spanish healthcare centres. However, having information on the various drug combinations being used, their concentrations, doses, diluents, routes of administration, and containers would help to increase the available information on their compatibility, stability, and clinical efficacy, which would clearly contribute to improving pain management and patient safety.
This is the challenge raised by the Pain and Pharmacotechnical Groups of the Spanish Society of Hospital Pharmacy (SEFH) within the MEDPAIN project (Update of Parenteral Analgesic Mixtures: Studies on Use, Compatibility, and Stability). Its final objective is to prepare a guideline containing information on stability, compatibility, indications for use, and safety data on the most common parenteral analgesic mixtures in Spain. This document will serve as a support for hospital pharmacists in the validation and preparation of these mixtures, as well as for other healthcare staff who care for patients with pain.
This article presents the first stage of the MEDPAIN project and provides a Spanish national map of the use of analgesic mixtures in hospitals and social and healthcare centres.
MethodsThis article presents a cross-sectional multicentre study based on a survey addressed to hospital pharmacists (members of the SEFH) working in Spanish healthcare centres during the period December 21, 2020 to April 4, 2021. Participation was voluntary and only one response per centre was accepted.
A multi-response questionnaire was designed on the RedCap platform for dissemination through the SEFH distribution list. The project was also disseminated on social networks (Twitter) to increase participation, thus increasing to the greatest extent possible its representativeness by region and by the mixtures used.
Prior consent was obtained from respondents in the participating centres. Surveys were considered to be valid if they were received from Spanish centres and provided complete data on at least 1 analgesic mixture, although the participating centres were encouraged to provide information on 3 to 10 mixtures. The software allowed a maximum of 20 questionnaires to be completed, which had the advantage that they did not need to be completed at the same time; rather, the information could be saved and completed later.
An analgesic mixture was defined as the combination of 2 or more active ingredients (up to a maximum of 5), at least one of which was an analgesic. For the purposes of this study, mixtures were considered to be the same if they contained the same combination of drugs at different concentrations or were administered by different routes.
The surveys comprised 2 distinct parts. The first part provided instructions for completing the survey and reporting the demographic variables of the study: the name of the hospital or social and healthcare centre, the Autonomous Community to which it belongs, level of complexity, number of beds, and type of patients treated.
The first part had to be completed before the second part could be accessed. One questionnaire had to be completed for each analgesic mixture. The variables related to the analgesic mixtures were as follows: indication, type of patient (adult/pediatric), setting in which it is used (hospital/home), pharmacological composition of the mixture, diluent, route of administration, form of administration, frequency of use (daily, weekly, monthly, or when needed), final container, whether the mixture is protocolized, and whether it is prepared in the pharmacy service or in the nursing units.
The questionnaire allowed 2 to 5 components to be chosen via a drop-down list that included the main analgesic drugs (dexketoprofen, diclofenac, fentanyl, ketorolac, methadone, metamizole, morphine, oxycodone, paracetamol, sufentanil, and tramadol) and adjuvants, such as local anesthetics (bupivacaine, levobupivacaine, lidocaine, ropivacaine), benzodiazepines (midazolam), antiemetics (metoclopramide, ondansetron), antispasmodics (baclofen, butylscopolamine), corticosteroids (dexamethasone), clonidine, dexmedetomidine, and ketamine, plus an open option to indicate other drugs. The dose of each drug in the mixture could be filled in as total dose or concentration. Respondents could also indicate whether the mixture had fixed doses or concentrations of drugs or whether there was a range of doses or concentrations for the same analgesic mixture. In the latter case, the maximum and minimum dose or concentration of the 2 drugs considered to be the main drugs by the respondent was recorded.
A copy of the original questionnaire is included as supplementary information (Annex I).
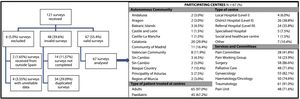
ResultsA total of 121 questionnaires were received, of which 67 (55.4%) were considered valid according to the criteria established in the study methodology. Fig. 1 shows the diagram of the surveys received and the reasons for rejecting those considered invalid.
Valid surveys were received from 13 of the 17 Autonomous Communities: Catalonia and the Community of Madrid provided the most surveys; none were received from the Canary Islands, Cantabria, Extremadura, and the Chartered Community of Navarre. Fig. 1 also shows the geographical distribution and characteristics of the participating centres. Only 1 survey was received from a social and healthcare centre. In total, 74.6% of the responding centres were Level II and III hospitals.
The 67 responding healthcare centres reported a total of 462 analgesic mixtures. A median of 6 mixtures was reported per participating centre (range 1–20; interquartile range p25–p75 = 4.0–9.0). Only 3 centres (4.5%) reported fewer than 3 mixtures, whereas 7 centres (10.4%) reported 15 or more analgesic mixtures.
Most of the mixtures were used in adults (93.9%) and in hospital settings (91.8%). Table 1 shows the results of the variables related to the 462 mixtures reported in this study. It should be noted that 73.6% of the mixtures (340/462) are protocolized in the healthcare centre and 57.8% are frequently used (177/462 are used daily and 90/462 weekly). On the other hand, 21.4% (99/462) are prepared in the pharmacy service.
Characteristics of the analgesic mixtures reported in the study. Frequency of occurrence of drugs in the mixtures by pharmacological group.
| Analgesic mixtures | Total = 462 (%) | Composition | Total = 462 (%) |
|---|---|---|---|
| Area of use | Drug (ATC Group) | ||
| Hospital | 424 (91.8%) | Opioids | 404 (87.4%) |
| Hospital and home | 81 (17.5%) | Morphine (N02A) | 206 (44.6%) |
| Indication | Tramadol (N02A) | 106 (22,9%) | |
| Acute pain | 226 (49.6%) | Fentanyl (N02A) | 69 (14.9%) |
| Palliative sedation | 132 (28.9%) | Methadone (N02A) | 12 (2.6%) |
| Chronic pain | 54 (11.8%) | Oxycodone (N02A) | 6 (1.3%) |
| Sedation-analgesia | 44 (9.6%) | Sufentanil (N01A) | 5 (1.1%) |
| Not answered | 6 (1%) | Benzodiazepines | 139 (30.1%) |
| Route of administration | Midazolam (N05C) | 139 (30.1%) | |
| Intravenous | 304 (65.8%) | Antiemetics | 135 (29.2%) |
| Subcutaneous | 116 (25.1%) | Metoclopramide (A03F) | 77 (16.7%) |
| Epidural | 69 (14.9%) | Ondansetron (A04A) | 58 (12.6%) |
| Intrathecal | 14 (3.0%) | Local anesthetics | 99 (21.4%) |
| Other | 11 (2.4%) | Levobupivacaine (N01B) | 35 (7.6%) |
| Type of patient | Ropivacaine (N01B) | 32 (6.9%) | |
| Adult | 434 (93.9%) | Bupivacaine (N01B) | 17 (3.7%) |
| Pediatric | 28 (6.1%) | Lidocaine (N01B) | 15 (3.2%) |
| Form of administration | Antipsychotics | 96 (20.8%) | |
| Continuous infusion | 365 (79.0%) | Haloperidol (N05A) | 72 (15.6%) |
| PCA | 66 (14.3%) | Levomepromazine (N05A) | 19 (4.1%) |
| Intermittent perfusion | 52 (11.3%) | Chlorpromazine (N05A) | 5 (1.1%) |
| Bolus | 22 (4.8%) | NSAIDS | 88 (19.0%) |
| Diluent | Dexketoprofen (M01A) | 73 (15.8%) | |
| Saline solution 0.9% | 402 (87.0%) | Ketorolac (M01A) | 15 (3.2%) |
| Other | 53 (11.5%) | Antispasmodics | 88 (19.0%) |
| Glucose serum 5% (5.0%) | 32 (6.9%) | Butylscopolamine (A03B) | 85 (18.4%) |
| None | 25 (5.4%) | Baclofen (M03B) | 3 (0.6%) |
| Ringer's lactate | 2 (0.4%) | Other analgesics | 86 (18.6%) |
| Final container | Metamizole (N02B) | 83 (18.0%) | |
| Bag | 285 (61.7%) | Paracetamol (N02B) | 3 (0.6%) |
| Elastomer | 162 (35.1%) | Others, unspecified | 57 (12.3%) |
| Cassette | 35 (7.6%) | Ketamine (N01A) | 15 (3.2%) |
| Syringe | 21 (4.5%) | Dexamethasone (H02A) | 9 (1.9%) |
| Others | 12 (2.6%) | Clonidine (C02A) | 3 (0.6%) |
| Implantable device | 5 (1.1%) | Dexmedetomidine (N05C) | 2 (0.4%) |
Abbreviation: ATC, Anatomical Therapeutic Chemical classification.
With the exception of diclofenac, all the drugs (analgesics and adjuvants) that could be chosen on the questionnaire to describe compositions appeared in some mixture. In total, the admixtures included 26 different drugs. Of these, there was a predominance of opioid analgesics, which were present in 87.4% of the admixtures; specifically, morphine appeared in 44.6% of them. The most frequently used adjuvant drug was midazolam (30.1%). By contrast, 19 combinations (30/462 mixtures) did not include an opioid analgesic, NSAID, metamizole, or paracetamol. Table 1 shows the frequency of occurrence in the mixtures by pharmacological group and drug.
Regarding indications, almost half of the mixtures were used in the treatment of acute pain (226/462; 49.6%) and mainly for postoperative pain (165/226; 73%). The second most frequent indication was palliative sedation (132/462; 28.9%). Table 1 shows that the reported mixtures were rarely used for chronic pain and sedoanalgesia. Regarding chronic pain, the main indication was oncologic pain (50%).
Although 462 mixtures were reported by the 67 participating centres, some combinations of active ingredients were identical. Thus, according to the definition of mixtures in this study, the analysis showed that there were 137 different mixtures (i.e. 137 different combinations of 2 or more drugs). Although most of the mixtures were composed of 2 drugs (40.6%), there were also mixtures with 3 (37.7%), 4 (15.2%), and 5 components (6.5%).
Table 2 shows the mixtures (35/137) that were described at least 4 times—ordered by frequency from the most to the least—with the indications for use reported by the respondents, whether the mixtures are used for adult and/or pediatric patients, and whether they are protocolized in any centre. This same table with the 137 different mixtures is provided as an appendix for online consultation as table 4. Most of these mixtures are mainly used for the treatment of adult patients; 18 combinations for pediatric use were recorded. Table 3 shows the 20 most commonly used mixtures (51.7% of the total), their main characteristics, the diluent used, the range of doses of the components, and the route of administration.
Analgesic mixtures described at least 4 times by respondents in the MEDPAIN study. Data are shown by indication, type of patient, and protocolization in at least one participating centre.
| Analgesic mixture | Sedation-analgesia | Acute pain | Chronic Pain (>3–6 mo) | Palliative sedation | Type of patient | Protocolized mixture | N (%) |
|---|---|---|---|---|---|---|---|
| Morphine + Midazolam + Butylscopolamine | X | X | X | A | X | 33 (7.14%) | |
| Fentanyl + Levobupivacaine | X | X | X | A | X | 28 (6.06%) | |
| Morphine + Midazolam | X | X | X | A/P | X | 24 (5.19%) | |
| Fentanyl + Ropivacaine | X | X | A/P | X | 22 (4.76%) | ||
| Morphine + Midazolam + Butylscopolamine + Haloperidol | X | X | A/P | X | 12 (2.59%) | ||
| Tramadol + Metamizole + Ondansetron | X | X | A | X | 12 (2.59%) | ||
| Morphine + Midazolam + Haloperidol | X | X | A/P | X | 11 (2.38%) | ||
| Tramadol + Dexketoprofen + Ondansetron | X | X | A | X | 11 (2.38%) | ||
| Tramadol + Dexketoprofen + Metoclopramide | X | A | X | 9 (1.94%) | |||
| Tramadol + Metamizole | X | X | A/P | X | 9 (1.94%) | ||
| Tramadol + Metamizole + Metoclopramide | X | A | X | 9 (1.94%) | |||
| Tramadol + Metoclopramide | X | X | A | X | 9 (1.94%) | ||
| Fentanyl + Bupivacaine | X | X | A/P | X | 8 (1.73%) | ||
| Morphine + Metoclopramide | X | X | X | A/P | X | 8 (1.73%) | |
| Dexketoprofen + Metamizole | X | A | X | 7 (1.51%) | |||
| Morphine + Haloperidol | X | X | X | A/P | X | 7 (1.51%) | |
| Morphine + Midazolam + Levomepromazine | X | A | X | 7 (1.51%) | |||
| Tramadol + Dexketoprofen | X | A | X | 7 (1.51%) | |||
| Morphine + Bupivacaine | X | X | A | X | 6 (1.29%) | ||
| Morphine + Midazolam + Butilescopolamine + Metoclopramide | X | X | A | X | 6 (1.29%) | ||
| Morphine + Metamizole | X | A | X | 6 (1.29%) | |||
| Tramadol + Dexketoprofen + Haloperidol | X | A | X | 6 (1.29%) | |||
| Metamizole + Other | X | X | A | X | 5 (1.08%) | ||
| Morphine + Midazolam + Butilescopolamine + Levomepromazine | X | X | A | X | 5 (1.08%) | ||
| Morphine + Levobupivacaine | X | X | A | X | 5 (1.08%) | ||
| Tramadol + Haloperidol | X | A | X | 5 (1.08%) | |||
| Tramadol + Ondansetron | X | A | X | 5 (1.08%) | |||
| Lidocaine + Ketamine | X | X | A | 4 (0.86%) | |||
| Lidocaine + Other | X | X | X | A | X | 4 (0.86%) | |
| Morphine + Butylscopolamine | X | X | A | X | 4 (0.86%) | ||
| Morphine + Butylscopolamine + Haloperidol | X | X | A/P | X | 4 (0.86%) | ||
| Morphine + Midazolam + Metoclopramide | X | X | A | X | 4 (0.86%) | ||
| Morphine + Ondansetron | X | X | X | A/P | X | 4 (0.86%) | |
| Morphine + Other | X | X | A | X | 4 (0.86%) | ||
| Oxycodone + Midazolam + Haloperidol | X | X | A | X | 4 (0.86%) |
Abbreviations: A, adult; P, pediatric.
Characteristics of the 20 most frequently used analgesic mixtures.
| Analgesic mixture/dose range (mg) | N = 462 | Main indication | Route of administration | Type of patient | Range volume/diluent | |||
|---|---|---|---|---|---|---|---|---|
| Morphine10–100 | Butylscopolamine 15–150 | Midazolam 6–160 | 33 | Palliative sedation | Subcutaneous/intravenous | A | 24–1000 mL PS/GS 5% | |
| Fentanyl0,1–1,5 | Levobupivacaine300–625 | 28 | Acute pain/sedoanalgesia | Epidural | A | 50–425 mLUndiluted/PS | ||
| Morphine10–250 | Midazolam10–250 | 24 | Palliative sedation/chronic pain | Subcutaneous/intravenous | A/P | 50–500 mLPS | ||
| Fentanyla | Ropivacaine100–400 | 22 | Acute pain/sedoanalgesia | Epidural | A/P | 50–500 mLUndiluted/PS | ||
| Tramadol200–600 | Metamizole6.000–12.000 | Ondansetron8–16 | 12 | Acute pain | Intravenous | A | 50–275 mLPS | |
| Morphine10–200 | Butylscopolamine5–60 | Midazolam5–100 | Haloperidol5–60 | 12 | Palliative sedation | Subcutaneous/intravenous | A/P | 50–500 mLPS/GS 5% |
| Tramadol100–400 | Dexketoprofen50–250 | Ondansetron4–16 | 11 | Acute pain | Intravenous | A | 50–250 mLPS | |
| Morphine20–40 | Midazolam5–45 | Haloperidol5–20 | 11 | Palliative sedation | Subcutaneous/intravenous | A/P | 24–500 mLPS/GS 5% | |
| Tramadol100–300 | Metoclopramide10–30 | 9 | Acute pain | Intravenous | A | 50–500 mLPS | ||
| Tramadol5–300 | Metamizole200–6000 | 9 | Acute pain | Intravenous | A/P | 50–500 mLPS/GS 5% | ||
| Tramadol100–600 | Dexketoprofen50–300 | Metoclopramide10–40 | 9 | Acute pain | Intravenous | A | 50–500 mLPS | |
| Tramadol200–400 | Metamizole2000–12,000 | Metoclopramide10–40 | 9 | Acute pain | Intravenous | A | 50–1000 mLPS | |
| Fentanyla | Bupivacaine50–250 | 8 | Acute pain/sedoanalgesia | Epidural | A/P | 5–300 mLUndiluted/PS | ||
| Morphine15–350 | Metoclopramide10–210 | 8 | Chronic pain/sedoanalgesia | Intravenous/subcutaneous | A/P | 50–500 mLPS/GS 5% | ||
| Morphine20–140 | Haloperidol5–56 | 7 | Acute pain/chronic pain/palliative sedation | Intravenous/subcutaneous | A/P | 50–250 mLPS/GS 5% | ||
| Dexketoprofene25–150 | Metamizole2000–8000 | 7 | Acute pain | Intravenous | A | 50–500 mLPS/GS 5% | ||
| Tramadol200–600 | Dexketoprofen150–300 | 7 | Acute pain | Intravenous | A | 96–500 mLPS/GS 5% | ||
| Morphine10–50 | Midazolam15–50 | Levomepromazine25–600 | 7 | Palliative sedation | Subcutaneous/intravenous | A | 50–500 mLPS | |
| Morphine10 | Bupivacaine5–18 | 6 | Chronic pain/sedoanalgesia | Intrathecal/epidural | A | 15–40 mLUndiluted/PS | ||
| Morphine5–30 | Metamizole2000–6000 | 6 | Acute pain | Intravenous | A | 100–500 mLPS/GS 5%. | ||
Abbreviations: A, adult; P, pediatric; PS, physiological saline; GS, glucose solution.
This study is the first to report the parenteral analgesic mixtures of 2 or more components that are being used in Spanish healthcare centres. However, similar studies have been conducted by other authors in other countries. For example, Zachrisson et al. evaluated the real-life use of analgesic combinations in palliative care in Sweden9. Observational studies of this type have also been conducted in the United Kingdom in the settings of palliative pain10,11 and acute pain12. The results of these studies are similar in that they highlight the lack of consensus in analgesic therapy, the great variability of drug combinations used, and the lack of evidence on the physical–chemical compatibility of many of the drugs.
Hospital pharmacists were chosen to be in charge of data collection on the basis of their involvement in pain management. This aspect could be seen as a limitation, given that other staff are involved in pain treatment and that their participation in this study would have been of great value. However, it proved more difficult to access such staff at the national level. Nevertheless, other authors have also chosen pharmacists as the providers of information on the use of analgesics,11 probably because of their strategic position in the pharmacotherapeutic process.
The percentage of rejected surveys was quite high (44.6%), which was probably due to the complexity of completing the survey over several working sessions. Nevertheless, 67 health centres from 13 Autonomous Communities participated, reporting a total of 462 mixtures: the median of 6 mixtures per participating centre was higher than 3 mixtures per centre, which was the original target of the study.
The main limitation of this study is that it was a qualitative voluntary study, which contributes to its lack of completeness and the possibility of errors being made when recording the data.
Many centres with pediatric care and 2 dedicated pediatric hospitals participated in the study, thus adding value to the data collected on mixtures for pediatric use. However, among the 462 mixtures reported, only 28 (6.1%) are for pediatric use: this aspect may indicate their underrepresentation in the overall results, or it may simply reflect the fact that mixtures are less often used for pain treatment in children2. Williams et al. conducted a survey on the practice of epidural analgesia in children in the United Kingdom, highlighting the problems of the lack of evidence to guide clinical decisions in some cases and the lack of specialists in the treatment of acute pain in pediatric patients12.
It is noteworthy that most of the participating centres have a pain unit (71.6%) and a working group or clinical committee dedicated to pain care (65.7%). A multidisciplinary approach, based on a patient-centred model, is key to effective pain management13.
The analysis of frequency of use by drug confirmed the wide use of opioids in analgesic mixtures. Among the nonopioid analgesics, metamizole is widely used, whereas paracetamol is little used. Among the adjuvant drugs, midazolam, antiemetics, and a variety of local anesthetics are frequently used. It is not known to which drugs the respondents were referring when they chose option “other” on the drop-down lists to describe the compositions: due to the complexity involved in adding this information, this aspect was accepted as a limitation at the time of designing the survey.
Of the 137 analgesic combinations, 18 accounted for 50% of the total number of mixtures and 58 combinations accounted for 80%. The information on the 20 most commonly used mixtures (see Table 3) shows great variability of drug concentrations used, and wide ranges in the volume used and their diluents. Such variability is biased due to how the term “analgesic mixture” was defined in this study: the same mixture was defined as “the combination of 2 or more drugs, whether at different concentrations or in different diluents or containers”. Variability would have been even greater if, for each combination, different mixtures had been considered according to concentration, target population, or routes of administration. In any case, the variability of the combinations used was very high: this result is in line with the results of similar surveys conducted in other European countries9–12.
This lack of standardization poses a risk to patient safety because it increases the risk of errors at all stages of the process. In this regard, we highlight the Standardize 4 Safety initiative in the USA, which focused on standardizing drug concentrations to reduce medication errors and to specifically standardize the concentrations to be used in patient-controlled analgesia (PCA) and epidural analgesia in both adult and pediatric patients14.
It should be emphasized that the composition of the analgesic mixtures collected in this survey was that reported by the participating centres and does not imply that the research team—at the date of publication of this article—investigated whether they had all undergone stability and compatibility studies in support of them. Some recently marketed drugs, such as levobupivacaine in infusion bags, include information on physicochemical compatibility with certain opioids or NSAIDs in their datasheets15; however, it is still very rare for pharmaceutical companies to share this information in the datasheets. In any case, validated stability studies should be encouraged in order to offer adequate levels of quality and safety.
On the other hand, the number of drugs (21.7% of the mixtures have 4 or 5 components), the presence of high-risk drugs (87.4% contain opioids), the form of administration (79% continuous perfusion), and the handling required to prepare many of the mixtures indicate that a high proportion of these will be of medium risk according to the Spanish Guide to Good Medication Preparation Practices in Hospital Centres. Therefore, it is recommended that their preparation should be centralized in clean rooms of hospital pharmacy services16. However, only 21% of the reported mixtures are prepared in pharmacy departments.
This study had the simple aim of presenting the daily reality of clinical practice in Spanish hospitals. It will be continued with the creation of a practical guide for users that also incorporates information on stability, compatibility, and compounding risk levels. This initiative could help to identify, for different reasons, more optimal and less optimal combinations and contribute to more effective and safer analgesic therapy. This is the main challenge that will be addressed in the second stage of the MEDPAIN project.
Similarly, future studies should investigate the usefulness of mixtures that do not contain any analgesics in their composition or those that contain similar types of drug in the same mixture, such as the combination of 2 antipsychotics, 2 local anesthetics, or 2 drugs from the same analgesic step17. The contribution of pharmacists as drug experts can provide great added value, as has been suggested by previous authors18–20.
In conclusion, this is the first study to date that—counting with the participation of 13 autonomous communities and including a considerable number of analgesic mixtures—confirms the great variability of drug concentrations used in current clinical practice and shows which drug combinations are most commonly used in Spain. A future literature review will allow us to complete the clinical and stability data on these mixtures and to make evidence-based recommendations for their use.
Contribution to the scientific literatureThis study is the first to report the most commonly used parenteral analgesic mixtures of 2 or more components used in Spanish health centres.
The results will make it possible to conduct a detailed review of the mixtures and to obtain data on indications, compatibility, and physicochemical stability, which will help provide better and safer use of these drugs.
FundingThis project was funded through a grant under a call for workgroup-developed proposals launched by the Spanish Society of Hospital Pharmacists in 2019.
Author contributionsCatalina Lara-Cátedra and Carmen López-Cabezas contributed equally to this study.
Conflict de interestThe authors declare no conflict of interest.
AcknowledgementsA special thank you to all pharmacists who participated in the survey included in the MEDPAIN study. Their contribution was instrumental in advancing our understanding of the routine use of analgesic admixtures in Spanish hospitals.
Technical support and statistical guidanceEmilio García Cabrera, Delos Clinical Contract Research Orgnization (C.R.O).