It is well-known that there is a lack of continuity in care received from the emergency department, as patients have to visit their physician in order to receive official prescriptions. A programme has been designed that aims to provide these patients with a therapeutic protocol to ensure that they are treated, thus improving coordination between the Hospital Emergency Department and Primary Care.
MethodsCreating a multidisciplinary team. Choosing the diagnoses that are most common in the emergency department and which are likely to be standardised. Developing treatment protocols, adapting them to the diagnoses selected. Creating a database, collecting, processing and analysing data. Designing satisfaction surveys, for patients given a therapeutic protocol, and for practitioners involved in the programme.
ResultsTreatment protocols were assigned to the nine most common diagnoses in the emergency department, with three-day treatment. The selected diagnoses covered 19.5% of the population attending the Emergency Department. A treatment protocol was dispensed to 17.3% of patients with the selected diagnoses. Patient satisfaction was excellent. Physicians approved of the programme, but the treatment protocol prescription did not agree with the degree of approval.
ConclusionsThe results show that the programme was excellently accepted by both patients and physicians, although the coverage given to the needs identified was lower than required.
Existe una situación de descubierto en la continuidad asistencial de los pacientes que acuden a los servicios de urgencias, al no poder disponer del tratamiento prescrito hasta que no pasan por su médico de atención primaria, donde obtienen las recetas oficiales. Se diseña un programa que pretende proporcionar a dichos pacientes un protocolo terapéutico, que garantice su tratamiento, mejorando la coordinación interniveles entre el servicio de urgencias del hospital y atención primaria.
MétodosCreación de un grupo multidisciplinario de trabajo. Selección de los diagnósticos más frecuentes en el servicio de urgencias susceptibles de protocolizar. Elaboración de protocolos terapéuticos adecuándose a los diagnósticos seleccionados. Creación de una base de datos, recogida, tratamiento y descripción de los mismos. Diseño de encuestas de satisfacción, para pacientes, a los que se les dispensó un protocolo terapéutico, y para facultativos involucrados en el programa.
ResultadosSe asignó protocolo terapéutico a los 9 diagnósticos más frecuentes en el servicio de urgencias, con tratamiento para 3 días. Los diagnósticos seleccionados cubrieron el 19,5% de la población atendida en el urgencias. Se dispensó un protocolo terapéutico al 17,3% de los pacientes con diagnóstico seleccionado. La satisfacción de los pacientes para con el programa fue excelente. Los médicos aprobaban el programa, pero la prescripción de protocolos terapéuticos no refleja concordancia con el grado de aprobación.
ConclusionesLos resultados muestran que el programa tiene una aceptación excelente tanto en los pacientes como en los facultativos involucrados, aunque la cobertura que se da a las necesidades detectadas fue menor que la requerida.
The perception of quality and the satisfaction level of patients regarding health services are becoming more relevant for the formulation and evaluation of social policies, in particular, of public health policies.1
The quality of care and the role of Critical Care and Emergency Department (CCED) depend on intrinsic factors of the medical emergency, and also on extrinsic factors. Currently, the demand in the CCED is high and in steady growth. The emergency assistance number is constantly growing, and it is estimated that over the course of one year more than half of the population visit the emergency department (ED).2
In the ED, the medical staff provide consultations for patients, conducting tests to make a final diagnosis, and prescribe medication, where necessary. The medical prescription is reflected in the reports of the ED, but it is not always accompanied by the official prescription from the health system, nor of the delivery of the medication prescribed. This will create an overdraft situation in the continuity of patients that come to the ED, because the patient has no access to the treatment that has been prescribed to them, until they see their primary care doctors. The family doctor makes the official prescription for a treatment that has not been prescribed by him, but that was prescribed by a doctor from the ED, sometimes the doctors may differ in the final diagnosis.
To improve the quality of care for patients who come to the ED, from the pharmacy service starts a programme for dispensing standardised medication, with which therapeutic protocols are established (TP) for most common diseases diagnosed in ED.
TP and clinical practice guidelines emerged in the 1980s, with the aim of improving the performance of medical staff and health service administrators. They are considered as a tool for making patient care more efficient and consistent, with the main aim of decreasing the variability in treatment, thereby increasing quality and reducing associated costs.4
Protocols are part of the scientific review applied to patient care. Its development is based on the accumulation of scientific evidence, transparency and replicability of the method. Its main goal is to achieve quality improvement in health care.5 In the production and design of protocols for clinical practice the following should be considered: improving the quality of care, allowing the choice of alternative treatments, providing the necessary tools for decision making, promote medical knowledge and patient education, bearing in mind the needs of the population and considering the ethical aspects.3
The presentation of the protocol is of utmost importance to ensure follow-up. The description of the evidence and recommendations should be accessible and concise, so that the information is quickly assimilated by the user. In some cases, the use of algorithms can help the understanding and assimilation of the information provided.6
In recent years the opinion of users of health services has taken an increasing value as a measure of quality.
User satisfaction is the difference with a positive sign between the perceived quality and expectations on the service.7 Satisfaction is a complex, multidimensional, difficult to measure concept which changes according to different situations and people, as it relates to both the nature of the need that determines the demand for care and other factors that influence the perception of the service: style of life, past experiences, prior expectations and values of the individual and society.8
There are 3 reasons why you should consider satisfaction as an important measure of results of a health care process. First, it has been shown that satisfaction is a good indicator of treatment compliance by patients, and adherence to consultation and service provider. Secondly, satisfaction is a useful tool to assess the consultations and communication models, for example, success in informing and involving patients in decision making about the kind of attention that they need. And third, the opinion of the patient can be used systematically to improve the organization of the services that are going to be provided.9
The main objective of this work is to ensure continued care for patients who come to the ED. Therefore, the following actions have proposed from the hospital management: (1) develop a programme for dispensing standardised medication for patients attending the ED, (2) measure the impact of the programme, (3) measure the degree of satisfaction in both patients who are dispensed TP medications, such as doctors who prescribe TP medications from the ED.
MethodsTo achieve the proposed objectives a quasi-experimental study of medication dispensing protocol with additional information was conducted, which was called TP. Taking into account the importance of satisfaction as a measure of quality, satisfaction surveys were made by patients and doctors which allowed to record the opinion about this new service.
The hospital is a tertiary hospital divided into 3 distinct physical areas, General Medical Surgical Hospital (GH), Traumatology Hospital (TH) and Maternal and Child Hospital (MCH). The study took place in the ED of GH, from September 2005 through June 2006.
A multidisciplinary working group was established, driven by the hospital management and made up by emergency, primary care and hospital doctors. The working group chose 9 diagnoses to standardise their treatment. The selection was based on the frequency of the diagnoses, on the discharge reports of the patients in ED, and on their own experience.
The diagnoses selected were: muscle pains, cystitis, penicillin-allergic patients with cystitis, renal colic, odontogenic pain/pharyngotonsillitis, gastroprotection, injuries with infected soft tissues, immobilization, urticaria.
To assign treatment to each of these diagnoses, the group relied on clinical practice guidelines5,6,10–12 and their experience, always taking into account the drugs in the hospital pharmacotherapeutic guide.
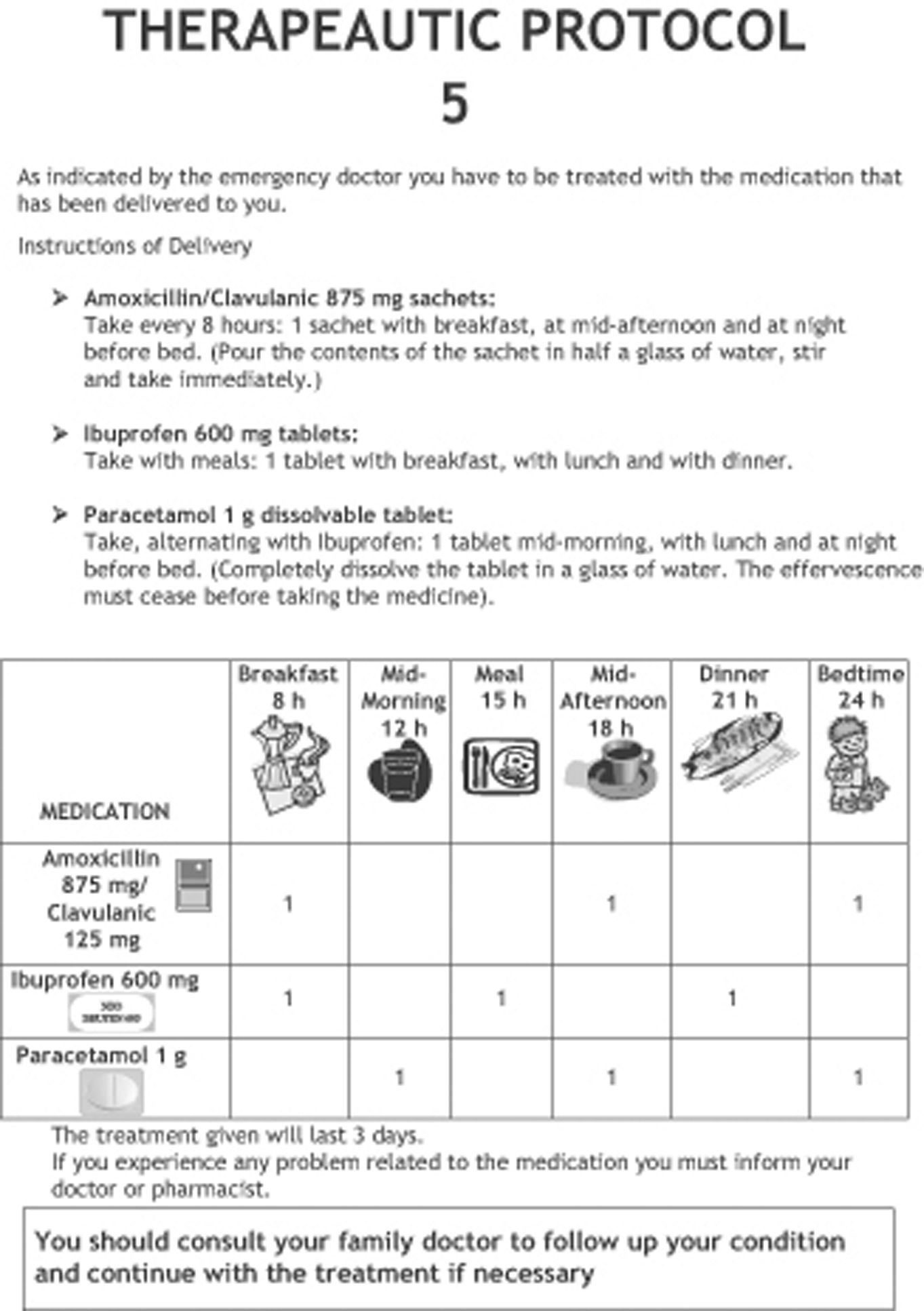
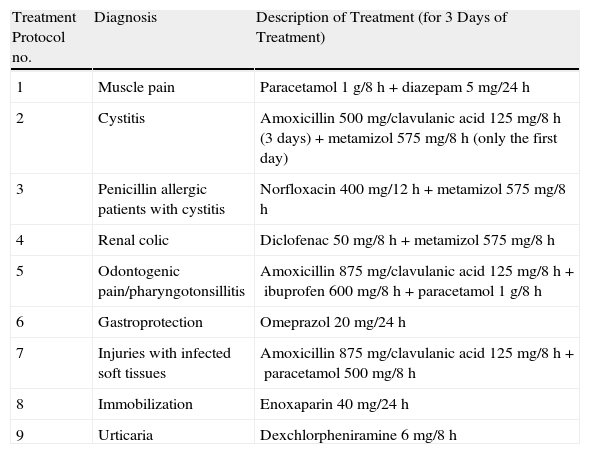
The result was the design of 9 TPs, for the 9 selected diagnoses. The description of the treatments that contained the TP, for each of the diagnoses, is shown in Table 1. Each TP was presented properly packaged and duly identified with the necessary medication for 3 days of treatment. It also included a printed explanation, detailing the appropriate advices for taking the drugs it contains (Fig. 1). The form informed the patients about the need to visit their family doctor, so that the continuity of treatment can be assessed.
Description of Treatment of the 9 Therapeutic Protocols Designed for the 9 Selected Diagnoses.
| Treatment Protocol no. | Diagnosis | Description of Treatment (for 3 Days of Treatment) |
| 1 | Muscle pain | Paracetamol 1g/8h+diazepam 5mg/24h |
| 2 | Cystitis | Amoxicillin 500mg/clavulanic acid 125mg/8h (3 days)+metamizol 575mg/8h (only the first day) |
| 3 | Penicillin allergic patients with cystitis | Norfloxacin 400mg/12h+metamizol 575mg/8h |
| 4 | Renal colic | Diclofenac 50mg/8h+metamizol 575mg/8h |
| 5 | Odontogenic pain/pharyngotonsillitis | Amoxicillin 875mg/clavulanic acid 125mg/8h+ibuprofen 600mg/8h+paracetamol 1g/8h |
| 6 | Gastroprotection | Omeprazol 20mg/24h |
| 7 | Injuries with infected soft tissues | Amoxicillin 875mg/clavulanic acid 125mg/8h+paracetamol 500mg/8h |
| 8 | Immobilization | Enoxaparin 40mg/24h |
| 9 | Urticaria | Dexchlorpheniramine 6mg/8h |
For the dissemination of the programme, e-mails were sent, briefings were organised and methacrylate fact sheets were placed in each of the consultation rooms, from which the TPs were prescribed. These fact sheets described the contents of each of the 9 TPs designed.
During the 6-month pilot phase, ED doctors prescribed the TP which was to be dispensed to patients by nursing staff in the discharge report. The pharmacy department was responsible for preparing and ensure the supply of TP.
Three data collection periods were established, each of 15 days approximately, to see the evolution of the programme over time: the first period of data collection, January 31–February 13, 2006; the second period, March 1–March 15, 2006, and the third period, May 15–May 31, 2006.
The study population consisted of patients who attended the GH's ED during the data collection periods established.
To measure the impact of the programme, a database was created where information recorded in the emergency department reports was collected, which were then reviewed during the data collection periods and then proceeded to treat them.
The following variables were collected: sex, diagnosis in the emergency department, diagnostic protocol (yes/no), referral to primary care (yes/no), referral to specialist (yes/no), patient satisfaction, doctor satisfaction.
We made a satisfaction survey for patients who were dispensed TP and one for the doctors who worked in the ED that were responsible for prescribing TP.
The patient survey mostly consisted of dichotomous closed-ended questions and a score from to 10 had to be assigned to the programme. We conducted a telephone survey of patients who received TP during the third period of data collection.
The doctor's survey was structured in 2 parts, one with dichotomous closed-ended questions, and another with open questions regarding possible modifications to the TP dispensed.
We carried out a descriptive analysis of the data, calculating absolute and relative frequencies (n and percentage) for all qualitative variables collected in the study (percentage of diagnostic protocol, percentage of patients with TP over the total patients), and also calculating the frequency distribution of the most common diagnoses.
We calculated the average daily number of emergencies attended; dispensing rates of TP were also calculated. These rates were defined as the number of patients who were dispensed the TP, divided by the total number of patients able to receive it for being diagnosed with one of the 9 diagnoses chosen for the study. These rates were calculated for different periods of data collection.
For the analysis of the satisfaction surveys, percentages were calculated for each of the possible answers (yes, no, sometimes). For the overall assessment of the level of patient satisfaction (measured with a scale of 1–10) the mean, standard deviation and median were calculated.
ResultsDuring 2005, emergency assistance was provided to 261 799 patients, of which 93,578 were dealt with in the GH, resulting in an average of 256 emergencies attended daily.
A total of 6428 reports were reviewed during the 3 data collection periods, with 1502, 1551 and 3375 reports corresponding to the first, second and third periods, respectively.
We analysed the relationship between the number of patients who have been dispensed TP (208) and the number of patients with one of the diagnostic protocols recorded the discharge report (1172), showing that 17.75% were dispensed TP.
Using an analysis by period, we obtained a dispensing rate of 12.5, 20.57 and 19.02% for the first, second and third data collection period, respectively.
Likewise, we analysed the number of patients dispensed with TP (230) compared to the total number of patients treated (6428). 3.58% of patients in the ED were discharged with a TP prescribed.
When analysing these results broke down as per the 3 data collection periods, we observe that in the first period, TP was dispensed to 41 of 1502; in the second period TP was dispensed to 70 of 1551; and in the third, to 110 of 3375 patients treated in emergency department, corresponding to 2.73, 5.09 and 3.26%, respectively.
The evaluation of the diagnoses of patients attended in the ED showed that of 6428 patients seen during periods of data collection, 1172 had one of the 9 diagnoses that had been selected to be standardised, which represented a 18.23%.
The evaluation of the diagnoses of patients in the ER showed that of 6428 patients seen during periods of data collection, 1172 had a diagnosis that fell within the 9 diagnoses chosen for being included in a treatment protocol, which was a 18.23%.
Having revised the reports, in the first period, 312 of the 1502 patients (20.77%) received the diagnostic protocol, while in the second period it was 350 out of 1551 (20.57%), and 510 out of 3375 (15.11%) in the third period.
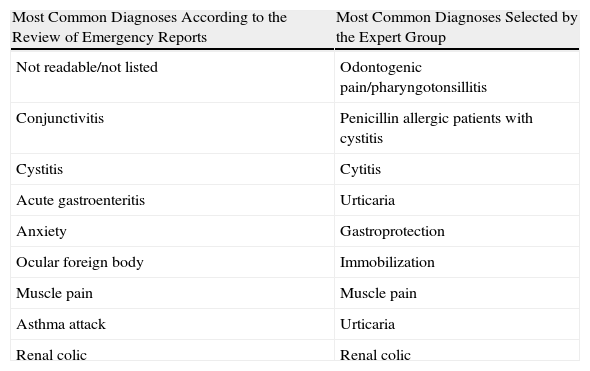
Table 2 shows the selected diagnoses to apply TP against the most common diagnoses after reviewing discharge reports.
Correspondence of the Most Common Diagnoses According to the Experience of the Expert Group With the Most Common Diagnoses According to the Review of Emergency Reports.
| Most Common Diagnoses According to the Review of Emergency Reports | Most Common Diagnoses Selected by the Expert Group |
| Not readable/not listed | Odontogenic pain/pharyngotonsillitis |
| Conjunctivitis | Penicillin allergic patients with cystitis |
| Cystitis | Cytitis |
| Acute gastroenteritis | Urticaria |
| Anxiety | Gastroprotection |
| Ocular foreign body | Immobilization |
| Muscle pain | Muscle pain |
| Asthma attack | Urticaria |
| Renal colic | Renal colic |
Two types of satisfaction surveys were drafted, one for patients who had been prescribed TP and another for emergency doctors who were responsible for prescribing TP.
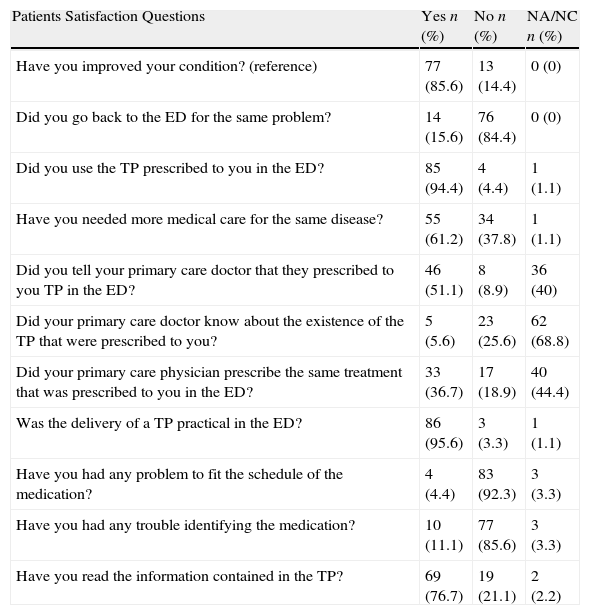
Of the 110 patients who received TP, only 90 (81.8%) were surveyed. The average score obtained for the programme was 8.7±0.5 and a median of 9. The survey results are shown in Table 3.
Results of the Patient Satisfaction Survey.
| Patients Satisfaction Questions | Yes n (%) | No n (%) | NA/NC n (%) |
| Have you improved your condition? (reference) | 77 (85.6) | 13 (14.4) | 0 (0) |
| Did you go back to the ED for the same problem? | 14 (15.6) | 76 (84.4) | 0 (0) |
| Did you use the TP prescribed to you in the ED? | 85 (94.4) | 4 (4.4) | 1 (1.1) |
| Have you needed more medical care for the same disease? | 55 (61.2) | 34 (37.8) | 1 (1.1) |
| Did you tell your primary care doctor that they prescribed to you TP in the ED? | 46 (51.1) | 8 (8.9) | 36 (40) |
| Did your primary care doctor know about the existence of the TP that were prescribed to you? | 5 (5.6) | 23 (25.6) | 62 (68.8) |
| Did your primary care physician prescribe the same treatment that was prescribed to you in the ED? | 33 (36.7) | 17 (18.9) | 40 (44.4) |
| Was the delivery of a TP practical in the ED? | 86 (95.6) | 3 (3.3) | 1 (1.1) |
| Have you had any problem to fit the schedule of the medication? | 4 (4.4) | 83 (92.3) | 3 (3.3) |
| Have you had any trouble identifying the medication? | 10 (11.1) | 77 (85.6) | 3 (3.3) |
| Have you read the information contained in the TP? | 69 (76.7) | 19 (21.1) | 2 (2.2) |
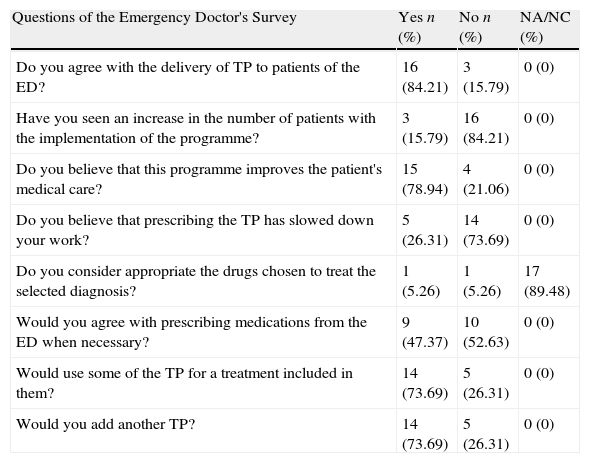
The survey was sent to 19 of 20 ED doctors and the results were anonymous.
The results of the closed questions of the doctor's survey are shown in Table 4. As for the changes proposed in the section reserved for the open-ended questions were as follows: concerning TP 1, add ibuprofen or metamizol; for TP 2, add fosfomycin and/or NSAID; for TP 3, add fosfomycin; in TP 4, add dexketoprofen and rescue tramadol; for the TP 5, add dexketoprofen; add corticosteroid in TP 9.
Results From Closed Questions Included in the Emergency Doctor's Satisfaction Survey.
| Questions of the Emergency Doctor's Survey | Yes n (%) | No n (%) | NA/NC (%) |
| Do you agree with the delivery of TP to patients of the ED? | 16 (84.21) | 3 (15.79) | 0 (0) |
| Have you seen an increase in the number of patients with the implementation of the programme? | 3 (15.79) | 16 (84.21) | 0 (0) |
| Do you believe that this programme improves the patient's medical care? | 15 (78.94) | 4 (21.06) | 0 (0) |
| Do you believe that prescribing the TP has slowed down your work? | 5 (26.31) | 14 (73.69) | 0 (0) |
| Do you consider appropriate the drugs chosen to treat the selected diagnosis? | 1 (5.26) | 1 (5.26) | 17 (89.48) |
| Would you agree with prescribing medications from the ED when necessary? | 9 (47.37) | 10 (52.63) | 0 (0) |
| Would use some of the TP for a treatment included in them? | 14 (73.69) | 5 (26.31) | 0 (0) |
| Would you add another TP? | 14 (73.69) | 5 (26.31) | 0 (0) |
Furthermore, doctors suggested the drafting of TP for diseases such as anxiety, asthma, corneal erosion, heart diseases, otitis and gastroenteritis.
DiscussionThe Department of Health is promoting the development of process management model, with the aim of reanalysing the health care work, taking into account the multiplicity of scenarios, participation of different professional groups and the sequential nature of the interventions, to address care processes comprehensively. This perspective, continued care, proper coordination between care levels, as well as a result-oriented approach are key points of the concept of quality to be achieved.13
The provision of instructions upon discharge is made in an unstructured way in most of the ED and assessment on the quality perceived by the user has not been tested.14
The TP dispensation programme is a pioneering experience and, therefore, typical problems have arisen. This is a dynamic programme and with a duration of 6 months. In the 3 data collection periods established by the working group, they reviewed 6428 reports: in the first and second data collection periods only 1502 and 1551 reports were reviewed, 3375 and in the third. This is because reports that contained X-rays were excluded in the first and second periods.
In the third period of data collection, patient satisfaction surveys are designed for people who were prescribed a TP and another survey for emergency department doctors. This gives us two key perspectives: that of patients receiving TP and of doctors who prescribe TP.
For the preparation of TPs, most frequent diagnoses which cover the largest possible number of patients coming to the ED are selected. This selection is also based on the experience of the working group that was created. These TPs were designed to be dispensed in both the ED of GH, as in the ED of TH, and for this reason, an immobilization TP appropriate to the needs of emergencies treated in the TH was created. The lack of staff in general was the reason why TP was not delivered in the ED of TH in this study period, so actually 8 different TPs were actually dispensed in the ED of GH.
With the review of the diagnoses in the discharge reports, it was found that the more frequent ones did not coincide with those selected to assign a TP. To give a greater coverage to patients who come to the ED, it should introduce TP for diagnostics such as anxiety, acute gastroenteritis, conjunctivitis, ocular foreign body and asthma attack.
When reviewing the reports and collecting the information we find that the applicability of TP was reduced for several reasons, one of which is the different ways in which doctors express a given diagnosis, and another is the failure to collect the diagnosis in the emergency report, because the diagnosis record was “not readable/does not appear”.
In addition, we found great diversity in establishing pharmacological treatment for the same diagnosis, which reduces the applicability of TP.
We also found that prescribing TP involved a change in the emergency doctors’ routine, which initially caused them to reject the programme. This could be observed during the programme introduction (doctors’ attitude towards programme) and the data analysis, which showed that only 19.62% of the total applicable cases were prescribed.
The information obtained by telephone survey is not exempted from criticism, usually by the overestimation of the quality,15,16 although they have been accepted and used for the evaluation of satisfaction in the emergency environment.17
When satisfaction surveys were analysed, we observed that the programme was very much welcomed by patients, since most of them used the TP dispensed in the ED and found it practical. They also read the leaflet which contained the TP designed by the pharmacy service. As for the doctors, they expressed their agreement with the programme, but medication was only sometimes considered to be appropriate for the treatment of selected diagnoses, and they proposed changes in the open questions included in the satisfaction survey. They even expressed their agreement with increasing the number of TP designed incorporating new diagnoses likely to be standardised.
Being a pioneering programme tailored specifically to a problem that occurs in our national health system we cannot compare the results with similar programmes and any other previous programme, but we can improve future actions in this aspect, based on the inconsistencies found in the proposed methodology and strengthening weaknesses found, taking into account the areas for improvement proposed by the doctors and staff involved in the programme.
With the dispensation of TP, this has ensured a continued care for patients who come to the ED, in a number of patients less than required; however, the degree of acceptance for the programme has been excellent both by patients, as the with the doctors involved.
Conflict of InterestThe authors declare that they have no conflict of interest.
We thank all health professionals who were part of multidisciplinary working group, both Primary Care, Emergency Department, Pharmacy Service and other areas of the Hospital Universitario Virgen de las Nieves. Thanks for your interest in improving continued care for patients and the quality offered in their services. Also we would like to give thanks the group FASTER (Pharmacy Care in Emergencies), always actively involved in the emergency area.
Please cite this article as: Chinchilla Fernández MI, et al. Dispensación de medicación protocolizada en un servicio de urgencias de un hospital de tercer nivel. Farm Hosp. 2011;35(3):106–113.
This project has been presented partially as a poster at the 54.° Congreso Nacional de la Sociedad Española de Farmacia Hospitalaria held in Zaragoza from 22 to 25 September, 2009.