Digital transformation impacts health care through technology. Telepharmacy is set to become one of the most important aspects of Telemedicine in the years to come with its ability to provide patients with increased and more timely access to pharmaceutical care, reduced costs for individuals and health systems, improved patient satisfaction, experience and convenience, and better health outcomes. Telepharmacy has gained increasing importance in the delivery of pharmaceutical care, largely due to the COVID-19 pandemic which has placed enormous pressures on healthcare systems globally. There is a significant amount of published literature from different countries around the world that provide examples of Telepharmacy. There are some innovative models of Telepharmacy services aimed at optimizing and improving access to pharmaceutical care, resulting in improved patient safety and outcomes. The benefits of Telepharmacy include increased value for pharmacies and pharmacists and adapting to patients’ needs, enhanced interprofessional care and increased efficiency of health systems and increased provision of patient-centred services, among others. However, despite these benefits, major barriers for implementation of Telepharmacy remain such as patient confidentiality and privacy of health information. These barriers to the implementation of Telepharmacy have been identified and can be divided into four different environments: technological, organizational, human and economic. Delivering pharmaceutical care and services through digital media is identified as a key priority for the International Pharmaceutical Federation. Digital health is one of the 21 Development Goals launched by International Pharmaceutical Federation in 2020. The International Pharmaceutical Federation Digital Health in Pharmacy Education report in 2021, describes the readiness, adaptability and responsiveness of pharmacy education and knowledge and skill needs of pharmaceutical workforce on digital health. Amongst other digital health tools, telehealth/Telepharmacy has been reported as one of the most preferred tools to teach and learn about by respondents.
La tecnología surgida de la transformación digital ha traído consigo cambios en la asistencia sanitaria. En los próximos años, la Telefarmacia previsiblemente se convertirá en uno de los aspectos más importantes de la Telemedicina, ya que ofrece a los pacientes un acceso más inmediato a la atención farmacéutica, supone una reducción de costes tanto para los pacientes como para los sistemas sanitarios, y deriva en una mayor satisfacción, experiencia y comodidad de los pacientes, mejorando así los resultados clínicos. Debido en gran medida a la pandemia de COVID-19, la Telefarmacia ha adquirido gran importancia en el ámbito de la atención farmacéutica, ya que esta crisis ha provocado una enorme presión sobre los sistemas sanitarios de todo el mundo. Se pueden encontrar multitud de experiencias publicadas en la literatura científica sobre modelos de Telefarmacia en diferentes países del mundo. Existen algunos modelos innovadores de servicios de Telefarmacia orientados a optimizar y mejorar el acceso a la atención farmacéutica, lo que se traduce en una mejora de la seguridad y los resultados de los pacientes. Entre las ventajas de la Telefarmacia se incluye el aumento del valor para las farmacias y los farmacéuticos y la adaptación a las necesidades de los pacientes, la mejora de la atención interprofesional, el aumento de la eficiencia de los sistemas sanitarios y la mayor prestación de servicios centrados en el paciente, entre otras. Sin embargo, a pesar de presentar múltiples ventajas, siguen existiendo importantes barreras para la implantación de la Telefarmacia, como la confidencialidad del paciente y la privacidad de la información clínica. Estas barreras para la implantación de la Telefarmacia pueden dividirse en cuatro ámbitos: tecnológico, organizativo, humano y económico. La prestación de atención y servicios farmacéuticos a través de medios digitales es una prioridad clave de la Federación Internacional Farmacéutica. La salud digital es uno de los 21 Objetivos de Desarrollo lanzados por la Federación Internacional Farmacéutica en 2020. El informe de la Federación Internacional Farmacéutica sobre salud digital en la formación farmacéutica en 2021 describe la preparación, adaptabilidad y capacidad de respuesta de la formación farmacéutica y las necesidades de conocimientos y habilidades de los farmacéuticos sobre la salud digital. Entre otras herramientas de salud digital, la Telemedicina/Telefarmacia ha sido señalada como una de las herramientas preferidas por los encuestados para formar y aprender.
Digital transformation positively impacts healthcare through technology. Digital technologies provide healthcare organizations with the tools to support greater standardization of work, which can improve efficiency. At the same time, 'big data’ also holds the promise of personalized medicine. Factors that drive this development include budgetary pressures and changes in both demographics and consumer behaviour. The technological revolution impacts healthcare by reducing healthcare costs, avoiding preventable deaths, improving health outcomes and quality of life, improving efficiency and quality of care and developing new drugs and treatments1.
Telemedicine, Telepharmacy, artificial intelligence (AI), enabled medical devices and electronic health records, examples of digital transformation in healthcare, are reshaping how health professionals and patients interact. Technology will continue to change and develop healthcare. Smart systems capable of understanding health issues and complicated new diseases will lead to innovations that will impact pharmacy. It will provide increased options and new ways for treating diseases, optimize diagnoses and improve shared decision-making processes as patients become more proactive in their care. While the promise of digital healthcare could lead to inclusive and equitable digital transformation in health, as a means for universal health coverage, it also brings challenges. Digital technologies have become a determinant of health, while ethics, data privacy, an evidence-based approach and equity should be ensured by design.
Health care systems and pharmacy are facing this technological revolution. There is increasing need to reduce the cost of care for individuals and health systems, meet consumers/patients expectations, and predict diseases faster and more accurately2. Consumers have access to a significant amount of health information and are becoming accustomed to the use and benefits of technology. Consumers and patients will expect changes in how they experience and receive health care.
The technological revolution brings with it the ability to deliver true 'beyond-the-pill’ value, with new services being provided by pharmacists. For community pharmacy to remain competitive and be best positioned for true integration in our health systems, investing in the emerging digital technologies, such as Telepharmacy, will be a prerequisite. Pharmacists can utilize technology to create links with patients through a common platform to access data and information which has not been possible in the past. Technology enables the storage of patient records, facilitates electronic prescriptions, the dispensing and administration of medicines, automates the handling of medicines in the supply chain, provides tools for monitoring the efficacy and safety of medicines; better equipment of pharmacists will contribute to the provision of high-quality pharmaceutical care and patient services. Opportunities for pharmacists in the digital landscape include optimizing medication adherence and medicines safety through increased identification of medicines-related problems, the delivery of more personalized care, and automation providing more time for pharmacists to consult with and manage patients, in collaboration with other health providers.
Electronic devices, such as electronic blood pressure and glucose monitoring devices, and smartphone healthcare apps for personal use, are increasingly becoming available. Pharmacists have an important role in facilitating the use of these technologies in addition to providing individuals with advice on the appropriateness of these technologies with respect to their own health care. With the increasing use of digital health tools in practice that change the way pharmacists deliver care, university curriculum should better integrate education on digital health to ensure students are prepared for rapid advances in technology when entering the workforce.
Telepharmacy is set to become one of the most important aspects of telehealth in the years to come with its ability to provide increased access to pharmacists, expanded quality of services, more timely access to services, reduced costs, improved patient satisfaction, experience and convenience, and better health outcomes3. In day-to-day practice, pharmacists answer questions regarding medicines interactions, vaccines and testing. With Telepharmacy, these dialogues can be performed with patients at home. It is encouraging to see that Telepharmacy is becoming more widely understood, used and appreciated. And there is a good explanation why: quite simply, Telepharmacy strongly enhances patient care.
A global overview of TelepharmacyTelemedicine has been defined as “the use of electronic information and communications technologies to provide and support health care when distance separates the participants”4. Telepharmacy, a more recent concept5,6, has been defined as “the remote provision of pharmaceutical care through telecommunication technologies”5,7. Evidence suggests that a wide range of clinical services and operational pharmacist activities can be conducted via Telepharmacy such as patient assessment, medication review, patient education, prescription verification, disease prevention and assessment of clinical outcomes6,8. Telepharmacy is a resource-effective way to deliver pharmaceutical services to individuals in rural areas, to individuals with mobility challenges or inflexible work schedules, without the physical presence of a pharmacist9.
Telepharmacy has gained increasing importance in the delivery of pharmaceutical care, largely due to the COVID-19 pandemic which has placed enormous pressures on healthcare systems globally10. In addition to the economic challenges, social distancing has limited the ability of patients to physically visit health care settings, such as pharmacies11. Telepharmacy has the ability to overcome many of the challenges presented by the pandemic while still providing quality pharmaceutical care. For example, hospital pharmacy services in Spain have adapted their outpatient services to be delivered by Telepharmacy, to optimise clinical outcomes and reduce the risk of viral transmission12. In the United States, changes in regulations have allowed pharmacies to utilize teleconferencing platforms, such as Zoom, which would have otherwise been non-compliant with privacy standards13. In Australia, changes were made to program rules in 2020 allowing pharmacists to undertake medication reviews via videoconference or teleconference14.
Telepharmacy models have been implemented for decades, especially where access to pharmacy is geographically challenging. For example, in Australia (1942), the United States (2000), Canada (2003), the United Kingdom and Hong Kong (2010), and others8. Early adopters of Telepharmacy have traditionally been rural and remote communities with insufficient access to traditional care providers. There is a significant amount of published literature on Telepharmacy. Not surprisingly, the majority is published between 2019 and 2022, during the time of the COVID-19 pandemic, highlighting the importance of pharmacists to continue to deliver pharmaceutical care, despite face-to-face delivery not being possible9. Articles related to Telepharmacy were identified from the Australia15,16, Bangladesh17, Brazil18, Canada19,20, China21, Germany22, Iran23, Italy24, Japan25, Jordan26, The Netherlands27, Pakistan28,29, Philippines30, Sub-Saharan Africa8, Saudi Arabia31,32, Spain33,34, Sri Lanka35 United Arab Emirates36, and the United States37,38.
There are some innovative models of pharmacists providing Telepharmacy services to optimise and improve access to pharmaceutical care. For example, a remote pharmacy service “Cloud Pharmacy Care”, a medication consultation service system and Telepharmacy service model based on the social software WeChat app, was developed in China21. The authors concluded that the consultation model assisted in providing medication management for chronically ill patients. Similarly in Denmark, a nationwide online Telepharmacy chat-service was developed for all individuals to receive counselling, irrespective of where a medicine was purchased, as part of the strategy for Danish pharmacies39. A 2017 study highlighted the feasibility of video-linkage technology integrated within a medicine supply robot (the Telepharmacy Robotic Supply Service) to provide community pharmacy services to a rural area in north-east Scotland40. The netCare programme in Switzerland is a pioneer initiative of Telemedicine and collaborative practice, by which the patient and pharmacist can consult with a general practitioner while the patient is at the pharmacy and presents symptoms. If the doctor confirms the diagnosis, they can issue a prescription that is dispensed immediately by the pharmacist41.
Telepharmacy can have a positive effect on patient safety and outcomes. A systematic review in 2017 concluded that clinical Telepharmacy interventions in the outpatient or ambulatory setting had an overall positive impact on outcomes related to disease management, patient self-management and adherence in the management of chronic diseases42. The effectiveness of Telepharmacy has also been demonstrated as a tool to reduce adverse drug events in hospitals43. Lastly, it has been shown that the remote review of medication orders by pharmacists decreased the number of potential adverse drug events and improved job satisfaction in the United States43. While it's important to consider the effect on clinical outcomes, improvements might follow from improved processes that deliver more cost-effective health care.
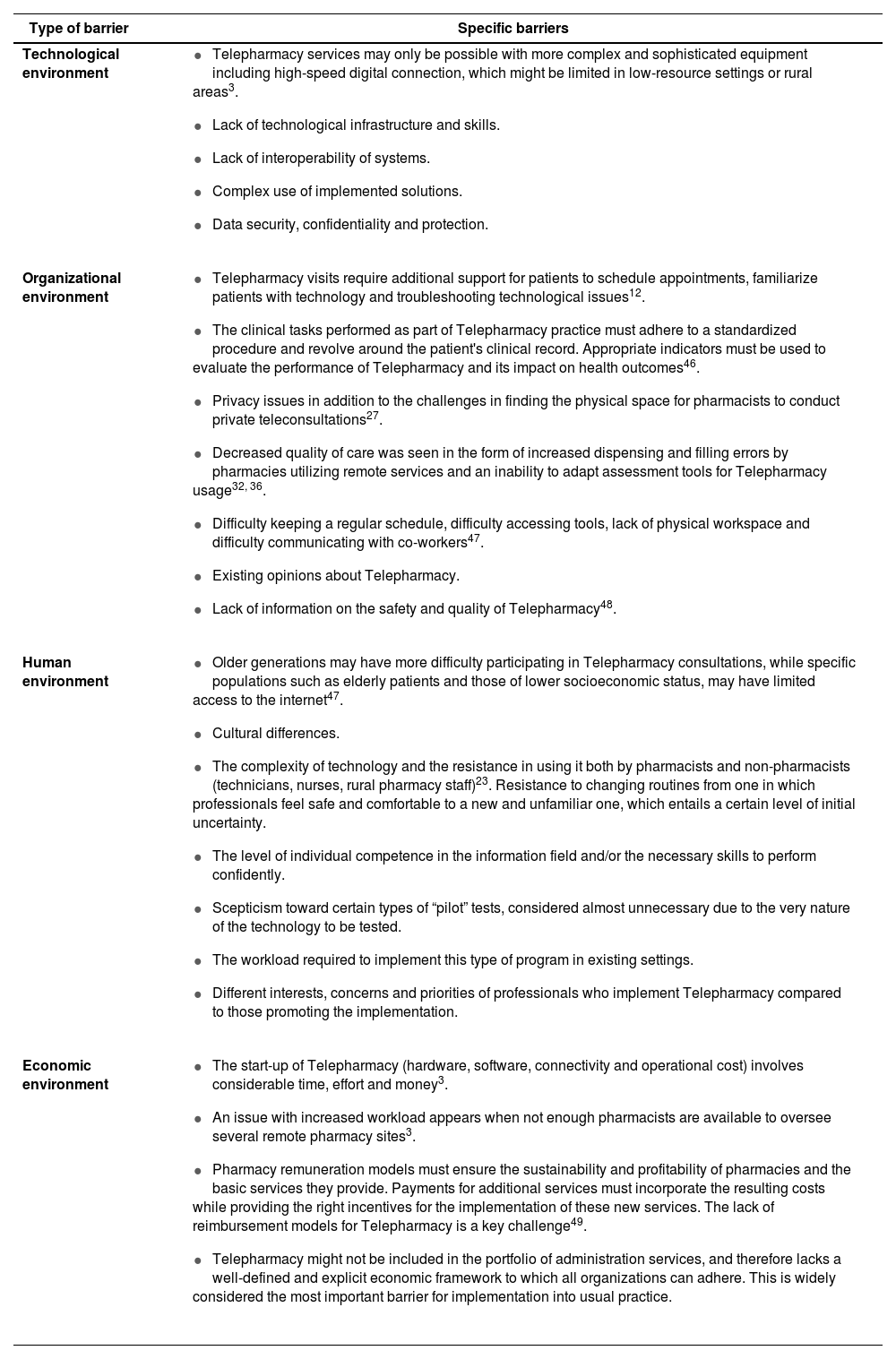
Implementation of Telepharmacy servicesDespite the benefits of Telepharmacy services, major barriers for implementation remain including confidentiality and privacy of health information, among others8. Outcomes to its successful use may be influenced by individual health and digital literacy and the extent to which pharmacy is integrated within existing care pathways. The complexity of Telepharmacy is often underestimated, and it's use is influenced by a number of factors ranging from societal acceptance to evidence that supports policy making44. Barriers to the implementation of Telepharmacy have been identified and classified into four different environments: technological, organizational, human and economic (Table 1)45. The identified barriers must be considered during the implementation of Telepharmacy, the context in which it is to be implemented and strategies developed to overcome these barriers.
Barriers to the implementation of Telepharmacy services
| Type of barrier | Specific barriers |
|---|---|
| Technological environment |
|
| Organizational environment |
|
| Human environment |
|
| Economic environment |
|
The abovementioned barriers contrast with several benefits that may facilitate the implementation of Telepharmacy into usual pharmacy practice. These include:
- –
Adaptation to a future technology-based environment:
The outbreak of the COVID-19 pandemic has accelerated the arrival and implementation of various technologies. Health systems have seen a significant increase in the uptake and use of technology for the delivery of health care. Therefore, there will be a need to integrate Telepharmacy to optimise the value of the pharmacist in improving patient outcomes10.
- –
Increased value for pharmacies and pharmacists and adapting to patients’ needs:
Pharmacists may utilise Telepharmacy to increase time spent with patients15, by obtaining information from patients to optimize appointment time50, building trust with patients for efficient Telepharmacy visits and protecting privacy by obtaining patient consent before a Telepharmacy consultation10. The use of Telepharmacy services can prevent unnecessary physical journeys to access care, which can result in cost-savings for patients51. Pharmacists may identify patient preferences (i.e. individuals who would prefer a Telepharmacy consultation) or identify patients who require intensive pharmaceutical care and determine whether they would benefit most from a Telepharmacy consultation or an in-person consultation34. There is an opportunity for pharmacists to determine patient satisfaction while providing choice through offering phone calls instead of video chats, or offering Wi-Fi video instead of using cellular data9.
- –
Enhanced interprofessional care:
Proactive involvement by other healthcare professionals and collaboration in care delivery is critical when considering the implementation of Telepharmacy. An interprofessional care coordinator may be vital for stakeholder buy-in and for the coordination of care within a collaborative model delivered in-person or virtually52. Inpatient Telepharmacy services offer the opportunity to work collaboratively in a clinical team, providing consistent pharmacy expertise in line with clinical model guidelines53.
- –
Increased efficiency of health systems and the provision of patient-centred services:
It has been shown that pharmacists utilising Telepharmacy for care delivery in remote locations is more efficient in remote locations when provided full access to electronic health record (EHR) systems54. In one study, both an on-site and remote pharmacist were significantly more likely to deliver remote pharmaceutical care interventions, when compared with a remote pharmacist alone (i.e., without an on-site pharmacist)55. Off-site pharmacists have shown to free up on-site pharmacists time to complete other tasks, such as providing enhanced patient care, serve on hospital committees or in the education of students56. Off-site pharmacists may also contribute to antimicrobial stewardship activities, medication reviews and discharge medication reconciliation56. Justifying the cost of an added on-site pharmacist, though, is a major barrier that can be exacerbated in remote areas struggling to retain or obtain the services of full-time pharmacists49.
In summary, the development of Telepharmacy should respond to a clearly perceived need by health professionals and will vary depending on geographical location and context. Pharmacy organizations should play a role in supporting pharmacists’ involvement in the delivery of Telepharmacy services. It is necessary to consider the aforementioned barriers to Telepharmacy implementation, the context and specific needs of the environment in which it is to be implemented, and the clinical, economic and humanistic benefits which may be achieved57.
International Pharmaceutical Federation's work around telehealth/Telepharmacy and future perspectives in this areaDelivering pharmaceutical care and services through digital health and platforms is a key priority area identified by the FIP. Digital health is one of the 21 Development Goals (DGs) launched by FIP in 202058. Development Goal 20 “Digital health” describes the global goals across pharmaceutical practice, science and workforce. The workforce element aims to enable digital transformation within the pharmacy workforce and effective processes to facilitate the development of a digitally literate pharmaceutical workforce. The science element supports the application of digital technology in healthcare delivery and in the development of innovative medical products. The practice element aims for systems and structures to be introduced for the delivery of quality digital health and pharmaceutical care services, through ensuring digital literacy, the utilisation of technology and digital enablers, and the configuration of responsive digital services to widen access and equity. Of particular importance are the Practice Element mechanisms required to achieve this goal, which include:
- 1.
Utilizing digital enablers and new technologies such as shared electronic health records, applications and AI to support the delivery of innovative services, appropriate care and decision-making.
- 2.
Demonstrating digital literacy and understanding of governance issues surrounding data ownership, ethics, privacy, quality information; with policies to support the development of the workforce as managers of health data.
- 3.
Recognizing digital health as a mechanism for widening access and equity, including access to digital pharmaceutical care.
- 4.
Identifying and understanding the ethical and operational implications of digital technologies, as well as the implications in terms of professional accountability for patient outcomes of expanded access to patient information and shared electronic records.
Many digital health technologies, including telehealth, strongly depend on uptake, appropriate use by healthcare professionals and implementation. The delivery of course content in pharmacy curriculum and training on digital health is important to support the pharmaceutical workforce with appropriate competencies, ensuring pharmacists understand and have the skills to use digital health in practice.
The FIP Digital Health in Pharmacy Education report, launched in 2021, presents findings from a global survey completed by academics, pharmacy practitioners and pharmacy students in 91 countries59. The report provides evidence to integrate digital health into pharmaceutical education to better equip the pharmaceutical workforce with the necessary digital health knowledge and skills, to optimize patient care. Focusing on the knowledge and skills status specifically related to telehealth in pharmaceutical education, the most common areas covered in the pharmacy curriculum included mobile applications (63%; n=112) and telehealth (41%; n=112). For respondents indicating that digital health was not embedded in their pharmacy curriculum (43%; n=267), telehealth was amongst the top three tools/services in which respondents were interested in teaching at their universities59.
A key gap in digital health education is the skillset and knowledge of pharmacists on how to best utilise technology to solve existing clinical problems and improve patient outcomes. Greater work is needed to demonstrate how digital health can be leveraged by pharmacists including specific guidance on the implementation of digital health tools in usual practice. Digital health education, as part of continuous professional development, and awareness by pharmacists are also critically important59.
FIP is committed to supporting its pharmacy education network to integrate digital health further into pharmaceutical education. As a result, FIP launched the 'train the trainer’ course in 2022 for educators which covers digital health. The course aims to empower educators on how to integrate digital health in pharmacy education curricula60.
ConclusionIt is clear there has been increasing application and implementation of Telepharmacy services globally, demonstrated by the large volume of published literature in this area, since 2019. This is a positive development when considering the sustainability of health care delivery. Technology is a key enabler for the delivery of pharmaceutical care and should be utilised to maximise clinical, humanistic and economic benefits for individuals and health systems. The potential for delivering pharmaceutical care via Telepharmacy is growing, as digital health industries expand, creating opportunities for integration and for pharmacists to deliver enhanced collaborative, patient-centred care, and at the same time, reducing inequity due to access. Interoperability with other technologies and systems required for the provision of care are important factors to consider in future.
FundingNo funding.
Conflict of interestsNo conflict of interests.