To describe an injectable extended-release antipsychotic pharmacotherapeutic follow-up program and to assess adherence among patients included in the program.
MethodA coordinated program is described involving hospital and primary care pharmacy, which included electronic prescription, reviewing, and dispensing of injectable antipsychotic agents in mental health and primary health care centers. Adherence to treatment was assessed in a 1-month prospective observational cross-sectional study which included all patients under treatment with injectable extended-release antipsychotics in a health area of more than 500,000 inhabitants. The variables collected were: medication administered, frequency of administration, administration center, and whether or not the patient attended the center. Patients were considered to have adhered to treatment if they had attended their appointments within a margin of ± 7 days.
ResultsA total of 919 patients and 1,073 appointments were included. Eleven mental health units and 40 primary health care centers participated in data collection. In 95.7 % (1,027) of cases, the patients attended the appointment. No differences were found in adherence between drugs or administration frequency. However, differences were found between mental health units and primary health care centers. Patient adherence was slightly higher in mental health units (97.6% vs 91.1%; P < 0.001).
ConclusionsThe high adherence rate shows that the described follow-up program is effective. Further long-term studies are needed to confirm this trend.
Describir un programa de seguimiento farmacoterapéutico de antipsicóticos inyectables de liberación prolongada y evaluar la adherencia de los pacientes incluidos.
MétodoSe describe un programa de prescripción electrónica, validación y dispensación de antipsicóticos a unidades de salud mental y centros de salud, coordinado entre farmacia de hospital y de atención primaria. La adherencia al tratamiento se evaluó mediante un estudio prospectivo, observacional y transversal de un mes realizado en un área sanitaria a más de 500.000 habitantes, en el que se incluyeron todos los pacientes en tratamiento con un antipsicótico inyectable de liberación prolongada. Las variables recogidas fueron: medicamento administrado, frecuencia de administración, centro de administración y si el paciente acudía o no a la administración, considerando que acudía si lo hacía en ± 7 días.
ResultadosSe incluyeron un total de 919 pacientes y 1.073 consultas programadas. En la recogida de datos participaron 11 unidades de salud mental y 40 centros de salud. En un 95,7% (1.027) de los casos, los pacientes acudieron a la administración del antipsicótico inyectable de liberación prolongada. No se encontraron diferencias en la adherencia entre los medicamentos ni entre frecuencias de administración, pero sí con respecto al centro donde se administraba el medicamento (unidades de salud mental frente a centros de salud), presentando una ligera mayor adherencia los pacientes de las unidades de salud mental (97,6% frente al 91,1%; p < 0,001).
ConclusionesLa elevada adherencia conseguida revela que el programa de seguimiento descrito es efectivo. En el futuro son necesarios estudios de mayor duración que confirmen esta tendencia.
The main objectives in the treatment of schizophrenia are to control symptoms, reduce the frequency and severity of psychotic episodes, improve quality of life, and facilitate the socio-occupational and family integration of the schizophrenic patient1. The ideal treatment is based on three pillars: early treatment, choice of the most appropriate antipsychotic for each patient, and adherence to treatment.
Maintaining adherence is fundamental to improving prognosis, but nonadherence rates range between 50% and 90%2. The Spanish Clinical Consensus on Therapeutic Adherence in Schizophrenia3 recommends as the first-line strategy the use of injectable extended-release antipsychotics (IERA), mainly second-generation or atypical. The use of second-generation IERAs can improve attitudes toward treatment and reduce the number of relapses4. These findings have recently led to this group of drugs being widely prescribed, and thus they have become a cause of high costs to health services5. As a consequence, prescription optimization strategies and pharmacotherapeutic follow-up programs are being developed to efficiently facilitate access to these treatments and to encourage adherence.
In this setting, the IERA Pharmacotherapeutic Follow-up Program was launched in our health area in 2015, with the aim of facilitating patient adherence to treatment and ensuring the traceability of the drug prescription, validation, and administration process registered in the electronic medical record system (IANUS®).
The objective of this study was to describe this program and assess adherence to treatment among patients included in the program.
MethodsThe IERA Pharmacotherapeutic Follow-up Program was developed by a working group comprising hospital pharmacists, primary care (PC) pharmacists, and health professionals from the psychiatric unit, quality unit, nursing unit management, and direction of the integrated management organizational structure. Mental health units (MHU) and healthcare centers (HC) participated in the program and all patients receiving IERAs in the area were included. The healthcare area has a population of 564,452 inhabitants living in 26 municipalities. The program involved the psychiatrists responsible for the patients, hospital and PC pharmacists, family doctors, and MHU and HC nursing staff.
The procedure for the implementation and development of the IERA Pharmacotherapeutic Follow-up Program in the Healthcare Area was presented to the Healthcare Committee and approved by the heads of the Hospital Pharmacy and Psychiatry Service and the Area Management. The program was launched in February 2015.
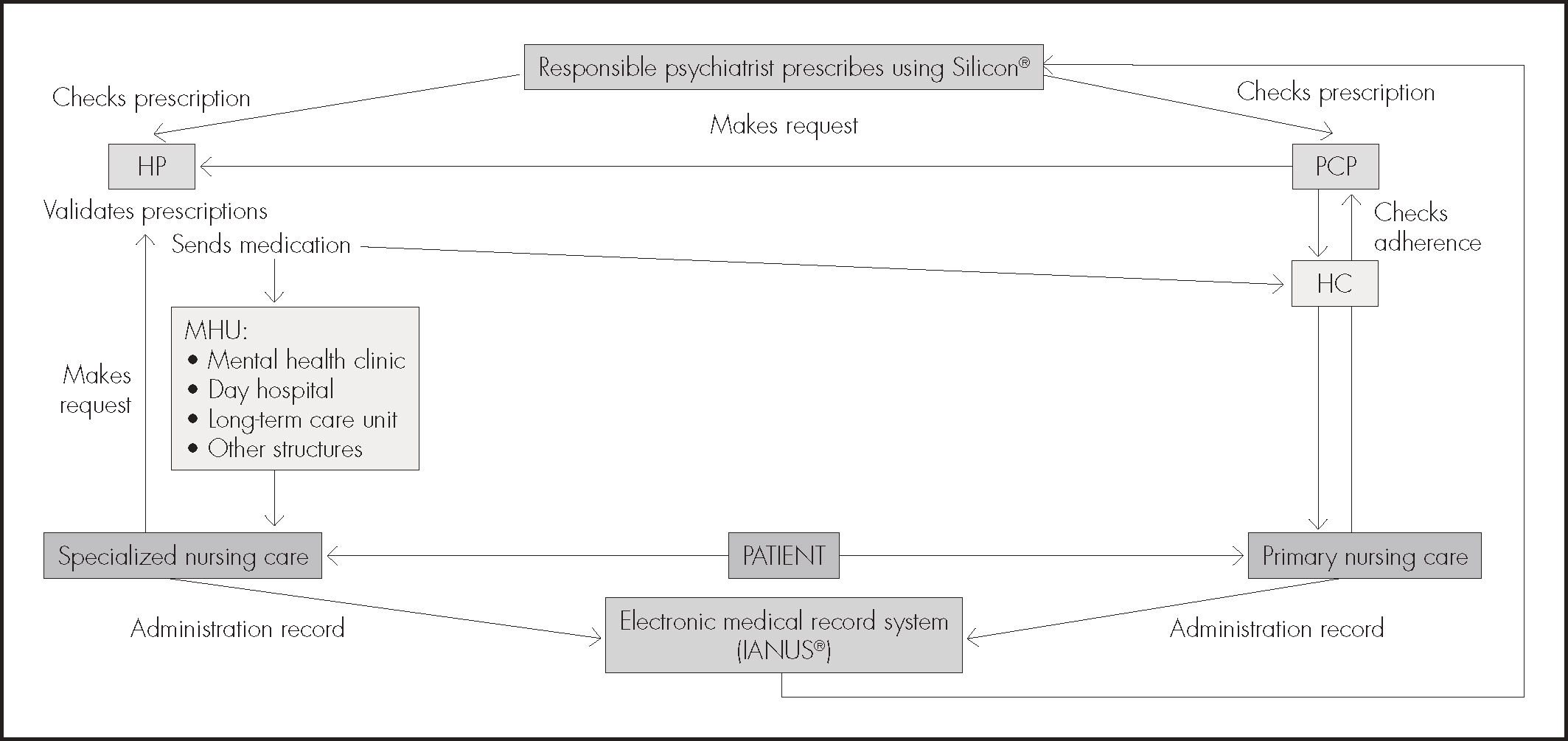
According to this program, the responsible psychiatrist directly prescribes the medication using the electronic form in the Silicon® application and indicates where the patient will be given it: MHUs (mental health clinics, day hospital, long-term care unit, or other mental health installations in the area) or HCs. The hospital pharmacist validates the prescription and checks that its indication, dosage, and conditions are in accordance with the summary of product characteristics, and the protocols approved by the regional Pharmacy and Therapeutic Committee (CAFT) and the local Pharmacy and Therapeutic Committee of the area.
In the MHUs, the patient is given an appointment with a member of the nursing staff, who is in charge of ordering the treatment of each patient from the hospital pharmacist each month using calendar-like speadsheets. In the HC, the PC pharmacist reviews and coordinates patient treatment and orders the antipsychotics every month from the hospital pharmacist, who sends them directly to the HC.
Dispensing is recorded per patient using Silicon® (i.e. the aforementioned application used for prescription and validation), which is connected to the unique electronic medical record (IANUS). Nursing staff administer the treatments and record them in the medical record (Figure 1). If patients fail to attend their appointments, staff members phone them and attempt to convince them to attend. A mental health integrated program of nursing care is followed in the MHUs.
This study presents the results of the program 3 years after its inception. This study was a prospective observational cross-sectional study that collected data from the patients included in the program over a period of one month.
The data collected were: scheduled appointments, appointments fulfilled, center where the patient had an appointment, and medication and frequency of administration. The medical record number was encrypted in a separate column to prevent access to the patients’ personal data. These data were tabulated using FreeOffice Calc, which is the spreadsheet component of the LibreOffice application. No demographic data were collected.
If a patient had several appointments that month they were counted independently, whereas if the patient had no appointment that month (e.g. quarterly IERA), it was not counted. Patients were considered to have adhered to treatment if they had attended their appointments within a margin of ± 7 days.
In the case of patients with appointments in the HCs, the PC pharmacist was responsible for tabulating the data and sending them to the study coordinator.
The hospital management department was asked for the number of patients who received nursing care in the entire area (both specialized care and PC) and the total number of patients with appointments during the same month in order to compare the patients included in the program with the rest of patients who usually attended nursing care services.
Descriptive stratified data analysis was conducted in relation to patient adherence (adherent vs non-adherent). The percentages of adherent patients were calculated and the following groups were compared:
- –
Patients receiving IERAs in MHUs and other patients attending specialized nursing care services.
- –
Patients receiving IERAs and other patients attending the HC nursing services.
- –
Patients receiving IERAs attending the MHUs and those attending the HCs.
- –
Different drugs.
- –
Different dosage intervals.
Depending on the case, two-tailed chi-square tests or two-tailed z-tests were conducted using a P value = 0.05 as a cutoff for statistical significance.
ResultsA total of 1,073 appointments corresponding to 919 patients were included. Data from 40 HCs and 11 MHUs were collected.
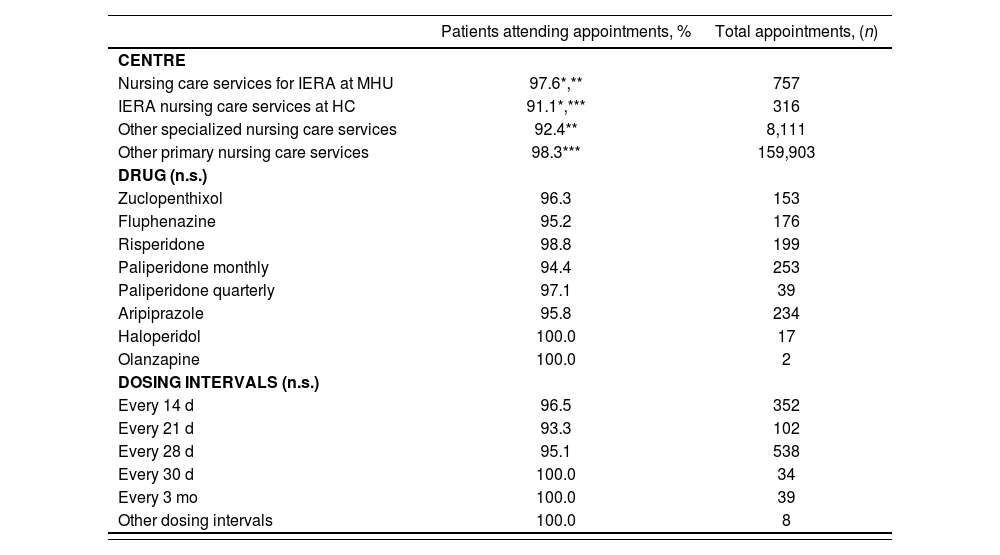
In 95.7% (1,027) of cases, the patients attended the nursing care services for the administration of IERAs. In 98.0% of cases, patients attended other general nursing care services. The results are shown in Table 1. No differences were found in adherence to treatment between the different prescribed medications or between administration frequencies, which varied between 2 weeks and 3 months. However, a significant difference was found in adherence to treatment between patients who received medication in MHUs and those who received it in HCs (97.6% vs 91.1%; P < 0.001).
Percentage of patients attending scheduled appointments
| Patients attending appointments, % | Total appointments, (n) | |
|---|---|---|
| CENTRE | ||
| Nursing care services for IERA at MHU | 97.6*,** | 757 |
| IERA nursing care services at HC | 91.1*,*** | 316 |
| Other specialized nursing care services | 92.4** | 8,111 |
| Other primary nursing care services | 98.3*** | 159,903 |
| DRUG (n.s.) | ||
| Zuclopenthixol | 96.3 | 153 |
| Fluphenazine | 95.2 | 176 |
| Risperidone | 98.8 | 199 |
| Paliperidone monthly | 94.4 | 253 |
| Paliperidone quarterly | 97.1 | 39 |
| Aripiprazole | 95.8 | 234 |
| Haloperidol | 100.0 | 17 |
| Olanzapine | 100.0 | 2 |
| DOSING INTERVALS (n.s.) | ||
| Every 14 d | 96.5 | 352 |
| Every 21 d | 93.3 | 102 |
| Every 28 d | 95.1 | 538 |
| Every 30 d | 100.0 | 34 |
| Every 3 mo | 100.0 | 39 |
| Other dosing intervals | 100.0 | 8 |
HC: health centers; IERA: injectable extended-release antipsychotics; MHU: mental health units; n.s. = non-significant differences.
The program described has several advantages over the previous system of obtaining a prescription and then dispensing in a community pharmacy. Since its implementation, treatments must be prescribed by a psychiatrist and validated by a pharmacist, which improves safety and adherence to approved protocols and guidelines. The program has contributed to improving integration between hospital pharmacy and PC pharmacy, as well as improving transitional care. There has been a favourable response from the staff involved in the program and many patients have asked to be included following its launch to avoid having to visit the community pharmacy before each nursing appointment.
Patients were considered to have adhered to their scheduled appointments if they attended them within a margin of ± 7 days. The literature6,7 defines nonadherent patients as those who stop taking their medication for 7 days over 3 months. No definition that addressed periods of one month was found. Nonadherent patients fulfilled the definition provided in the study, but some patients who were considered to be adherent may have experienced more delays in their appointments or may have even failed to attend in 3 months. Thus, the number of adherent patients was overestimated. The main limitation of this study is its short duration; nevertheless, it provides a snapshot of the current situation.
This study demonstrates the high rate of patient adherence according to the measurement criteria used. The short duration of the study appears not to be sufficient to explain the results obtained. Published rates of lack of adherence to treatment range between 50% and 90%. Marcus et al.8 conducted a study of oral antipsychotics and IERAs prescribed at hospital discharge and found nonadherence rates (i.e. adherence < 80% over 6 months) to IERAs of 51.8%, although the sample comprised patients with a history of poor adherence. In Spain, Gutiérrez Casares et al.9 conducted a prospective study of patients who had their therapeutic strategy changed and found adherence rates (i.e. adherence > 80% over 3 months) ranging from 79% to 94%.
In a recent review, Arango et al.10 emphasised the importance that these medications are made immediately available once they have been offered to the patient as a therapeutic option and that the Spanish national health service offers them without major restrictions. Accessibility is even higher in the program described, because the patient does not have to get the medication in a community pharmacy before going elsewhere for its administration; instead, it is available in the same place in which it is administered. The Pharmaceutical Management Law of the autonomous region of Galicia states that the functions of primary care pharmacy services are “to dispense medications (…) that require particular supervision and the control of a multidisciplinary team”, thereby supporting the implementation of similar programs throughout the region.
The adherence rate was significantly higher among patients who attended their MHU than among those who attended HCs. This difference could be explained by the mental health integrated care program implemented in the MHUs, the specialist nursing staff, and by the proximity and accessibility of the psychiatrist. However, the difference was small.
The users of the HC nursing services (non-IERA users) had higher adherence rates than those included in the program (P < 0.001). In the case of the non-IERA users, this finding could be due to the fact that most of these appointments are requested at very short notice to solve immediate problems (and this is not the case for patients receiving IERAs, who are usually given appointments 4 weeks in advance), or it could be due to the different health care provision offered. In contrast, adherence to appointments was higher among patients receiving IERAs attending MHUs than among non-IERA patients with appointments in specialized nursing care. The difference was statistically significant (P < 0.001) given the volume of appointments studied.
These results have the advantage of not being due to any special intervention aimed at increasing adherence: thus, it can be assumed that they reflect what happens in clinical practice as the result of a program that has been running for 3 years. Mantaining the usual working activities was a key aspect for the validity of the data obtained, and thus we strongly encouraged all staff to avoid making any changes to their procedures during the month of data collection.
The major strength of this study is its large sample size. A literature search did not find any study on adherence that included such a large sample of patients, that measured adherence in such an objective manner (i.e. the nursing record that the medication had been administered), and that did not influence the patients’ habitual attitude. Thus, the data obtained had high external validity. Furthermore, the patients included in the program were those considered by their psychiatrist to have medication adherence problems and therefore could benefit from IERAs. The main limitations of the study are that adherence was defined using a less strict criterion than that used in other studies. Moreover, as it is a descriptive noncomparative study, it cannot be concluded that the implemented program is better than other strategies to promote adherence.
In conclusion, the high adherence rate shows that the program described is effective. Further long-term studies are needed to confirm this trend.
FundingNo funding.
AcknowledgementsWe would like to thank all the mental health nursing personnel, primary care pharmacists, and psychiatrists of the EOXI Vigo who are actively involved in the program and participated in collecting the data needed for this study. We also thank the staff of the Quality department for their contribution to designing the program protocol and the Management control staff for providing us with the data needed for the study.
Conflict of interestsNo conflict of interests.
Contribution to the scientific literatureThe program described achieves very good adherence to treatment among patients treated with injectable extended-release antipsychotics. These patients are typically considered to be bad adherers. However, adherence is a determinant of clinical results among these patients and their health costs are very high. The data obtained had high external validity due to the large sample used and the objective manner in which adherence was measured. A literature search did not find any study that included such a large sample.
A 95.7% adherence score among 919 patients confirms the usefulness of a strategy that can be implemented in other health areas and health systems.