To describe the current situation of the hospital pharmacist in intensive care units and their activity in care, in teaching and in research.
MethodMulticenter and prospective study through a survey disseminated by the Spanish Society of Hospital Pharmacy, which consisted of several sections: personal and hospital's data, hospital's characteristics, pharmacist's involvement in intensive care units and teaching.
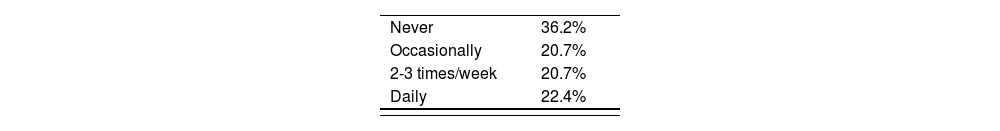
ResultsA number of 58 completed surveys were obtained. The number of pharmacists involved in intensive care units was 1 in 77.6% of cases, assisting an average of 30.8 beds (5-70). Experience of pharmacists in the intensive care unit was 5 years on average (2 months-25 years). Visitor's pass assistance and shift changes were between “never” by 36.2% to “daily” by 22.4%. Out of respondents, 93.1% reported a part-time intensive care unit involvement. Regarding activities undertaken, between 40-60% of pharmacists manage narcotics, teaching at intensive care unit, conciliation and safety. Between 60-80%, pharmacists cover clinical nutrition, notarization, optimization of pharmacokinetics and antibiotics; and 84.5% perform pharmacotherapy follow-up. Out of the surveyed pharmacists, 77.6% have specialized medical training, rotating intensive care unit residents in 86% of cases.
ConclusionsMost of the surveyed hospitals have one part-time pharmacist in these units. In order to improve the quality of pharmaceutical care of critically ill patients, it would be necessary to extend the involvement in time and staff, regarding the current situation, and a greater number of hospitals should include pharmacists in hospital intensive care units.
Describir la situación actual del farmacéutico de hospital en las unidades de cuidados intensivos, su actividad asistencial, docente e investigadora.
MétodoEstudio multicéntrico, prospectivo mediante encuesta difundida por la Sociedad Española de Farmacia Hospitalaria, la cual constaba de varios apartados: datos personales y del hospital, características del hospital, implicación del farmacéutico en la unidad de cuidados intensivos y docencia.
ResultadosSe obtuvieron 58 encuestas completadas. El número de farmacéuticos implicados en unidades de cuidados intensivos era 1 en el 77,6% de los casos, atendiendo una media de 30,8 camas (5-70). La experiencia en la unidad de cuidados intensivos del farmacéutico fue de 5 años de mediana (2 meses-25 años). La asistencia al pase de visita o cambios de guardia fue entre “nunca” en un 36,2% a “diariamente” en un 22,4%. El 93,1% de los encuestados reportaron dedicación a tiempo parcial en la unidad de cuidados intensivos. Respecto a actividades desarrolladas, entre el 40-60% gestiona estupefacientes, docencia en unidad de cuidados intensivos, conciliación y seguridad; entre el 60-80% abarca nutrición clínica, protocolización, optimización de antibióticos y farmacocinética, y un 84,5% realizan seguimiento farmacoterapéutico. Un 77,6% cuenta con formación sanitaria especializada, rotando los residentes en la unidad de cuidados intensivos en un 86% de los casos.
ConclusionesLa mayor parte de los hospitales encuestados cuenta con un solo farmacéutico a tiempo parcial en estas unidades. Con objeto de mejorar la calidad de la atención farmacéutica del paciente crítico sería necesario ampliar la dedicación en tiempo y personal respecto a la situación actual y que más centros incluyan al farmacéutico en las unidades de cuidados intensivos hospitalarias.
Pharmacists are essential members of the multidisciplinary healthcare team, and it has been shown to significantly contribute to optimizing pharmacotherapy and prevention of medication errors1. The intensive care unit (ICU) is one of the areas that benefit most from the incorporation of a pharmacist into the care team due to the characteristics of critically ill patients, who have a severe disease, multiple organ failure and multiple comorbidities, requiring a complex pharmacotherapeutic treatment. The use of high-risk medications and the susceptibility of patients makes medication errors have more serious consequences than in other hospitalization floors2.
In 2000, a work group of the Society of Critical Care Medicine and the American College of Clinical Pharmacy defined the level of clinical practice and specialized skills that should characterize the ICU pharmacist as a clinician, educator, researcher and manager, and established fundamental desirable and optimal requirements, both in pharmacy services and staff for providing pharmaceutical care to critically ill patients3. Similarly, the National Institute for Health and Care Excellence (NICE) established the optimization of pharmacotherapeutic treatments as an essential component of patient care, comprising various facets of pharmacy practice, such as medication reconciliation, treatment review, monitoring security and development of support systems for clinical decision-making4.
In a study conducted in 2015 which included 279 ICUs in the UK, it was observed that 96.6% of them had at least one pharmacist in the staffing of health care personnel. In addition, it was found in said study that pharmacists spent 24.5% of their working hours in multidisciplinary visitor's passes; 58.5% to the independent review of patients and treatments, while the remaining 17% spent their working hours in other activities related to the intensive care field5.
In studies available to date, it is shown that the involvement of pharmacists in ICUs is relevant due to the fact that it has been proven to have a positive impact, both clinically and economically. The findings show that pharmaceutical interventions in connection with optimizing treatments are linked to a significant improvement in patient care, as well as to a reduction in length of ICU stay, in the incidence of adverse events and mortality6–12. Since 2000, in Spain, pharmacists have gradually joined different hospital's clinical areas. Nevertheless, integration in ICUs had been limited to some specific hospitals. Over the past five years, the number of pharmacists who have joined ICUs has increased, which is why in 2018 the FarMIC work group (Pharmacists of Intensive Care and critically ill patients) was established within the Spanish Society of Hospital Pharmacy (SEFH). The main objective of this group is to bring together pharmacists who –through their work experience in ICU– could share knowledge with other colleagues, encouraging activity in care, in teaching and in research of this field. During the making of the group, the need to obtain a map of the current situation regarding the pharmacist's role at the hospital in ICUs in Spain was raised, in order for it to serve as a starting point for the group's activity.
The main objective of this study is to describe the current situation of the pharmacist's role at the hospital in ICUs, their activity in care, in teaching and in research.
MethodsMulticenter, prospective study, initiated and conducted by survey by SEFH's FarMIC work group through Google®'s virtual platform forms, directed to SEFH's mailing list along with a letter explaining the reason for the survey and brief instructions on how to properly carry it out. The survey was conducted in April, 2018 and its completion was absolutely voluntary and without monetary compensation.
The questionnaire consisted of a series of semi-structured or closed questions, clearly and concisely formulated, and easy to answer. It consisted of several parts or sections, including: personal and hospital data –where respondents are pharmacists–, ICU's number and characteristics of hospital, pharmacist's involvement in ICU –taking into account the number of pharmacists, specific tasks performed, time spent and experience time for its evaluation–, training for internal resident pharmacists (FIR in Spanish) –rotations, interns, external rotating pharmacists–, and research activities carried out along with the ICU's multidisciplinary team. The details of the survey are presented in Annex I.
The obtained responses were collected in an Excel® database created for this purpose, whose access was restricted only to the researchers of the study. Each formulated question was globally and separately analyzed.
A descriptive analysis of the responses presenting qualitative variables as percentages and quantitative variables as mean (± standard deviation) was performed, in case they were distributed according to normal law, or as mean and interquartile range if not met.
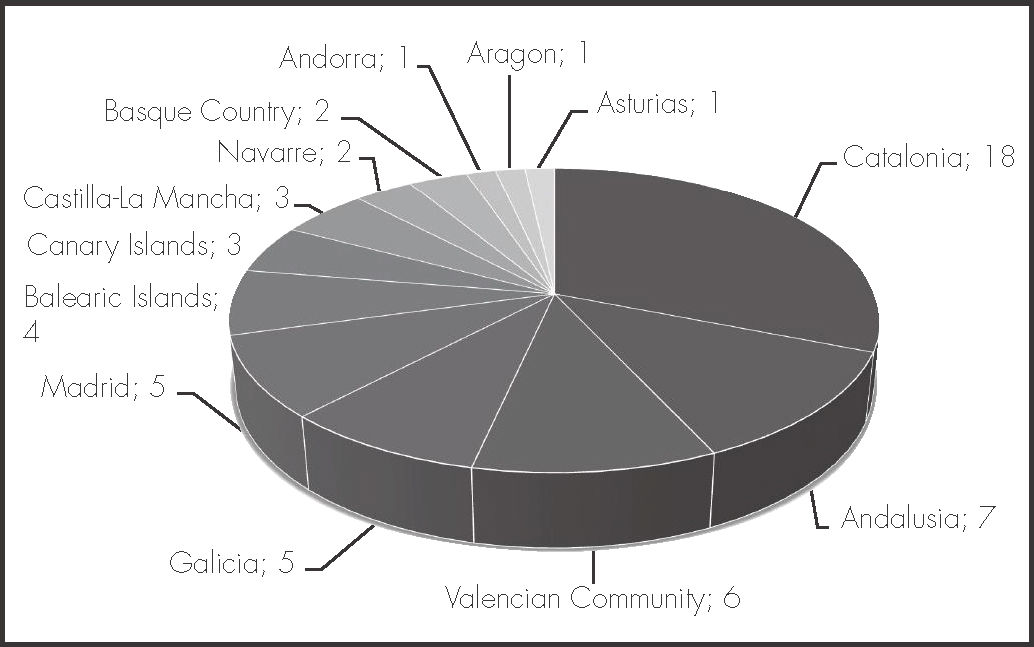
ResultsA number of 58 completed surveys belonging to 56 hospitals were obtained. Geographical distribution is shown in figure 1.
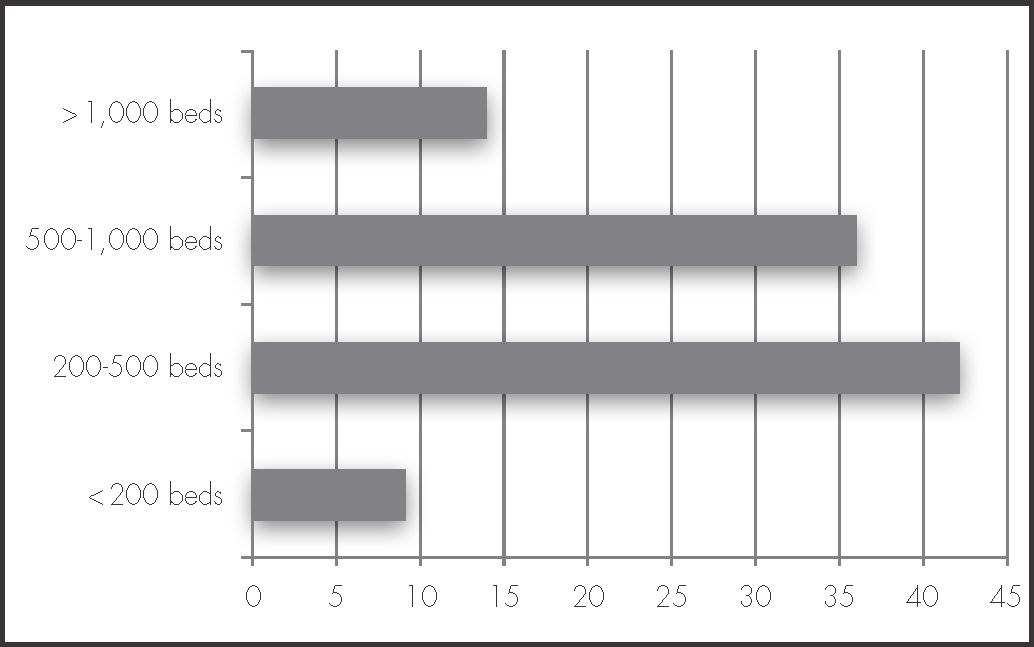
Data from the completed surveys were from hospitals with different number of beds as shown in figure 2.
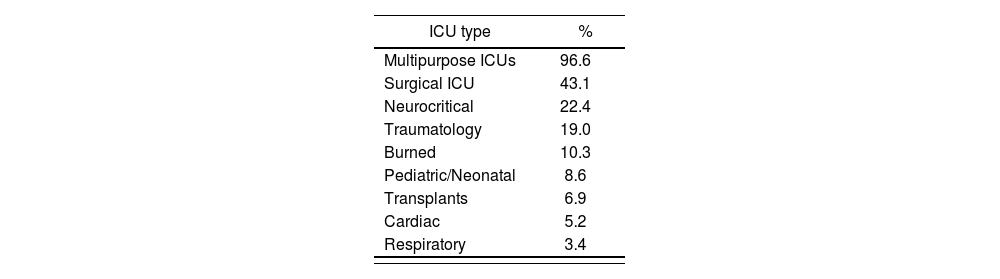
Based on the findings, the referenced type of ICU characteristics are distributed according to table 1.
As for the number of involved pharmacists activity in ICU was 1 in 77.6% of cases, 2 in 15.5% and 3 in 6.9%; processing an average of 30.8 beds for every pharmacist (5-70). Pharmacists’ professional experience in clinical pharmacy activities in intensive care ranged from 2 months to 25 years, which serves a mean of 5 years.
Visitor's pass assistance and shift changes are shown in table 2.
Out of the respondents, 93.1% reported a part-time involvement at the ICU, which serves an average of 2.7 ± 1.7 daily hours. 8.6% of respondents count on interns’ collaboration in ICU to carry out the activity.
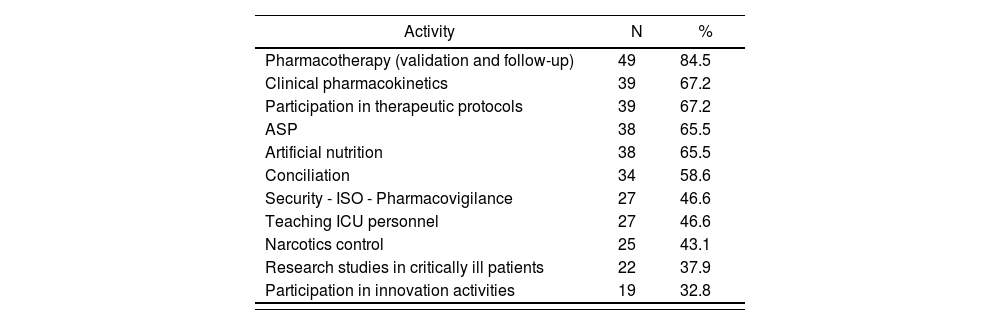
The activities performed by pharmacists for pharmaceutical care in critically ill patients are shown in table 3. In summary, less than 40% is dedicated to research and/or innovation; between 40 and 60% manages narcotics, as well as teaching ICU's personnel, also conciliation and safety; 60 to 80% covers clinical nutrition, notarization, Antimicrobial Stewardship Programs (ASP) and pharmacokinetics; and 84.5% of respondents perform validation and pharmacotherapy follow-up.
Activities carried out by respondents on pharmaceutical care in critically ill patients
| Activity | N | % |
|---|---|---|
| Pharmacotherapy (validation and follow-up) | 49 | 84.5 |
| Clinical pharmacokinetics | 39 | 67.2 |
| Participation in therapeutic protocols | 39 | 67.2 |
| ASP | 38 | 65.5 |
| Artificial nutrition | 38 | 65.5 |
| Conciliation | 34 | 58.6 |
| Security - ISO - Pharmacovigilance | 27 | 46.6 |
| Teaching ICU personnel | 27 | 46.6 |
| Narcotics control | 25 | 43.1 |
| Research studies in critically ill patients | 22 | 37.9 |
| Participation in innovation activities | 19 | 32.8 |
ASP: Antimicrobial Stewardship Programs; ISO: International Organization for Standardization; ICU: intensive care unit.
As for the number of involved pharmacists activity in ICU was 1 in 77.6% of cases, 2 in 15.5% and 3 in 6.9%; processing an average of 30.8 beds for every pharmacist (5-70). Pharmacists' professional experience in clinical pharmacy activities in intensive care ranged from 2 months to 25 years, which serves a mean of 5 years.
Out of the respondents, 77.6% of hospitals count on FIR training, rotating residents in ICU in 86% of cases. Out of the respondents, 46.6% in external rotation for residents from other centers are accepted.
DiscussionAccording to the findings of our survey, the presence and activity of the hospital pharmacist in ICUs is unevenly distributed among hospitals in our area. The pharmacist's presence –if ever– in these units and its number varies widely between different hospitals in the same region. These differences are even greater when compared between regions.
Pharmacists have established themselves as team members of critically ill patients’ units for over 40 years13,14. Among the multiple tasks to be performed by pharmacists in assisting critically ill patients15, include validating the global pharmacotherapeutic profile, increasing adherence to clinical guidelines, carrying out activities to optimize antimicrobial therapy, assuring treatment conciliation at admission and discharge, adjusting medication dose to various clinical processes, evaluating and monitoring nutrition, and getting involved in different multidisciplinary work committees within the hospital. However, according to the results obtained, distribution and relevance of the diverse pharmacists’ tasks in said units in Spain differ from the classification presented by the American College of Clinical Pharmacy and the Society of Critical Care Medicine in its position paper regarding the essential, desirable and optimal tasks that should be included within the pharmacist's role in critical care units3.
To date, the degree of implementation of pharmacists in the ICUs in Spain has been unknown. The results of this study have shown that most hospitals have a one part-time pharmacist, being temporarily supplemented with a fellow or a resident, which results in executing a large number of clinical tasks with clearly insufficient resources. Note that in the hospitals of our environment, optimizing the use of antimicrobials, teaching FIR activities of clinical nutrition and pharmacokinetic monitoring are the most frequently implemented by the respondent pharmacists –validating the pharmacological treatment being the most frequent–. The pharmacotherapy review and adaptation of critically ill patients carried out by pharmacists can reduce the stay and save costs according to multiple studies9,16. On the other hand, the management of narcotics and participation in the unit's research/innovation are activities with a lesser degree of implementation.
Notably, involvement in patient safety activities was less than 50%. Given the high risk of medication errors in this group of complex patients and their potential consequences17–19, setting the goal of increasing the involvement of pharmacists in the development of strategies aimed at assuring the patient's safety is certainly a pending task in our hospitals. The afore mentioned experiences on pharmacists’ participation in activities aimed at different ICUs’ safety have proven their ability to reduce medication errors8,20,21. In fact, various safety guidelines for the critically ill patient recommend a pharmacist's involvement in these activities as a desirable action22,23.
Limitations of our study include the methodology of sending data for its voluntary reply via e-mail. It is known that those centers with greater activity tend to participate more actively in surveys than others. Thus, the activity of pharmacists in the ICUs in Spain could be less than it is shown in our findings. However, the homogeneous distribution of surveyed hospitals both in size and complexity allow collecting a wide variety of centers in terms of resources and available time, which properly ascertains the type of activities performed on critically ill patients in our environment.
In short, the pharmacist's participation in critical care units is irregular in Spanish hospitals. In order to improve the quality of pharmaceutical care for critically ill patients, it is essential to extend the involvement in time and staff regarding the current situation, as well as having more centers include pharmacists in the multidisciplinary teams for ICU patients.
FundingNo funding.
Conflict of interestsNo conflict of interests.
Contribution to the scientific literatureThe role of pharmacists in intensive care units is widely practiced across countries, being involved in different activities: optimizing the pharmacotherapy treatment and ensuring the patient's safety. It has proven an improvement in clinical and economical results. However, the hospitals’ degree of involvement in the intensive care units in our environment is unknown.
Our study shows for the first time in Spain the degree of implementation of hospital pharmacists in intensive care units, showing a great diversity in the carried out activities, as well as the time spent on pharmaceutical care of critically ill patients.