To describe a compounding training plan in a tertiary hospital pharmacy service. The project aimed pharmacy assistant technicians to use a digital training platform and simulation techniques.
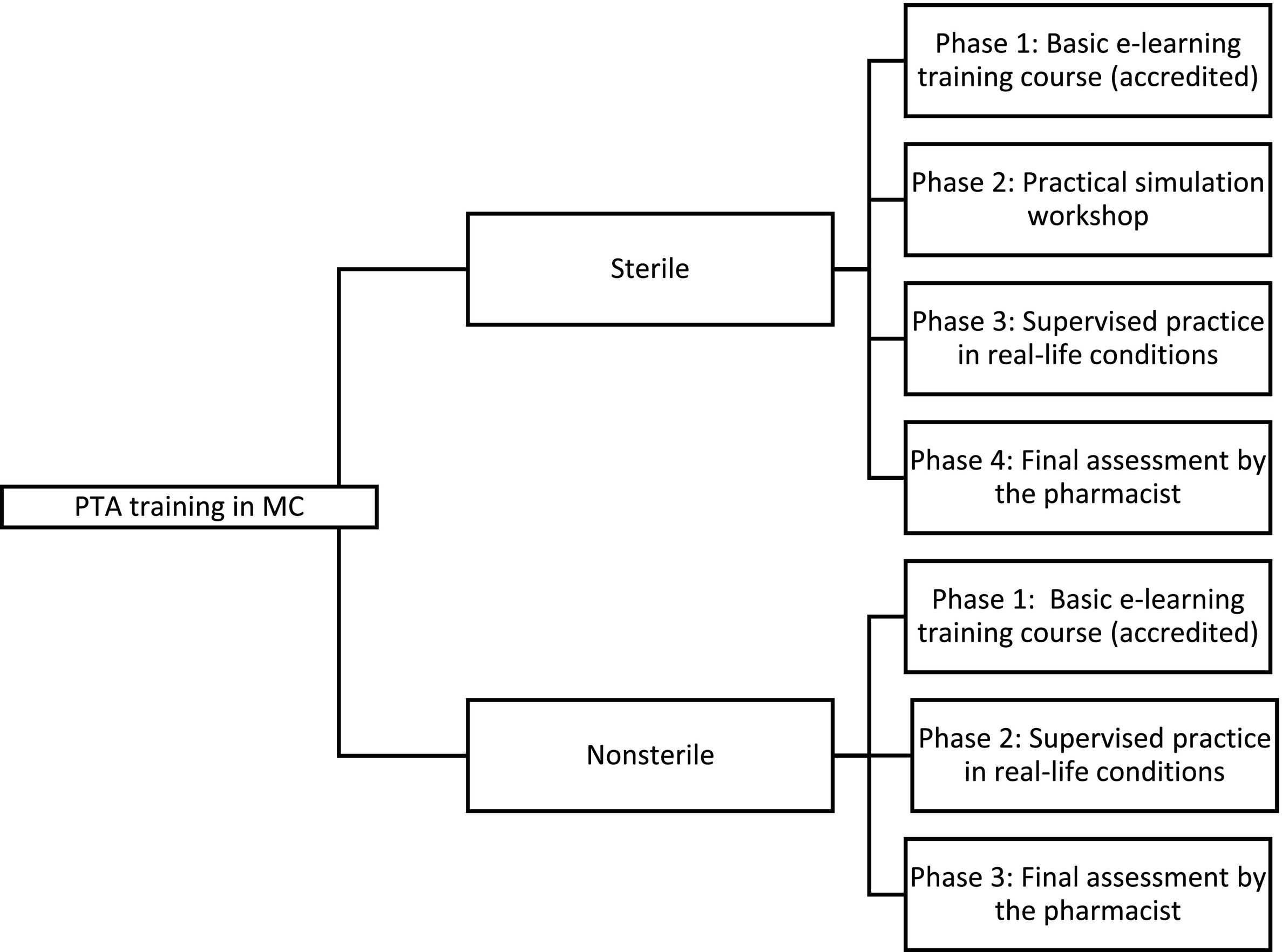
MethodsTwo training programs were designed, one for sterile and the other for non-sterile drugs. Each programme consists of several phases: a basic online training course (digital e-learning platform), a practical simulation workshop, a supervised practice in real conditions, and a final verification by the pharmacist to qualify the technician. Both programs include continuous and accredited evaluation by the hospital's Continued Education Commission.
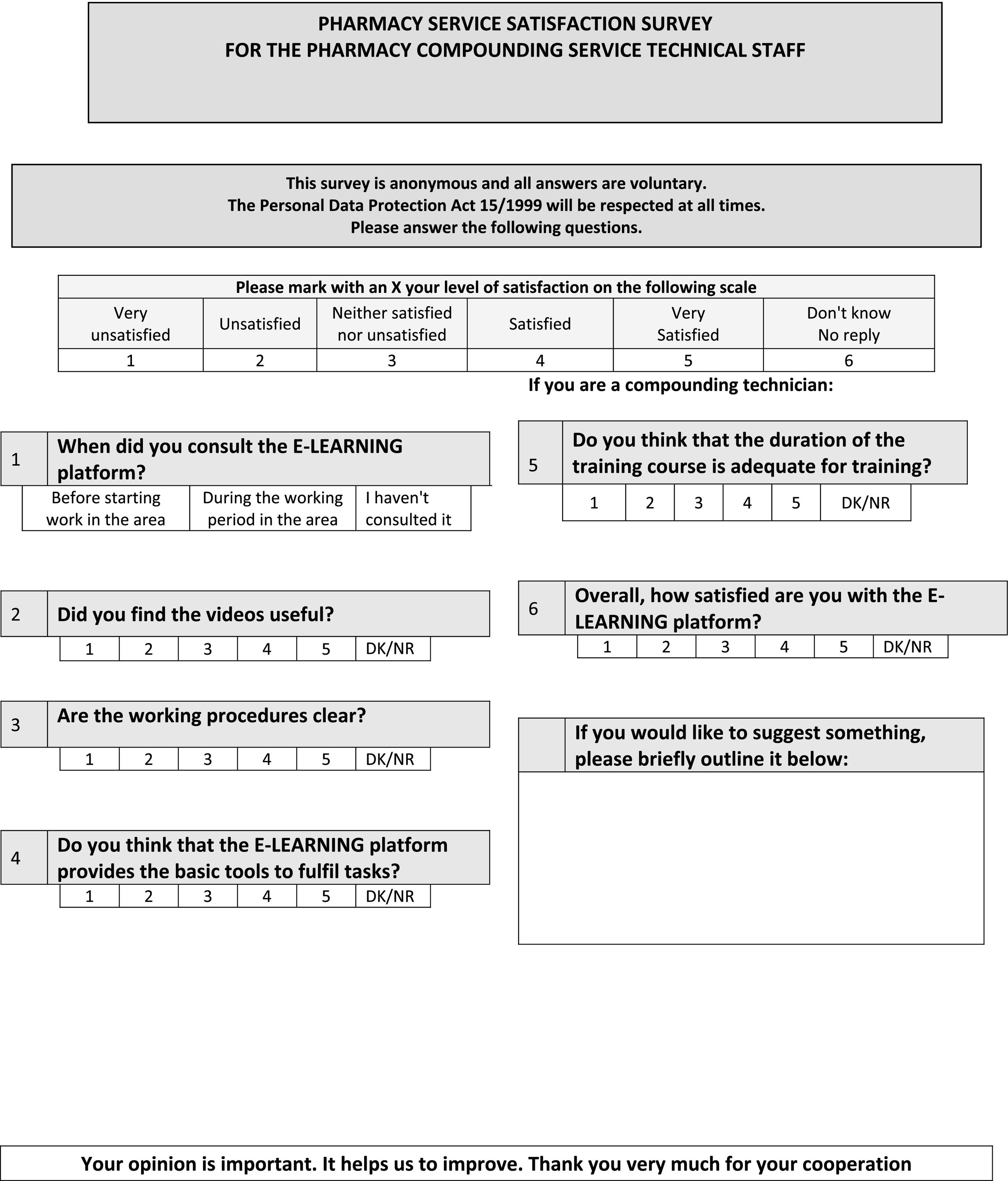
A satisfaction survey on training (e-lerning platform) was designed and conducted for pharmacy technicians (sterile and non-sterile).
ResultsThe project has been running for 3 years. Six specialist pharmacists from different areas involved in compounding are responsible for training and continuous evaluation. Twenty-one technicians have been trained, and nineteen have obtained qualifications. Two of them were found to be unfit. Currently, we employ13 pharmacy technicians who were initially trained.
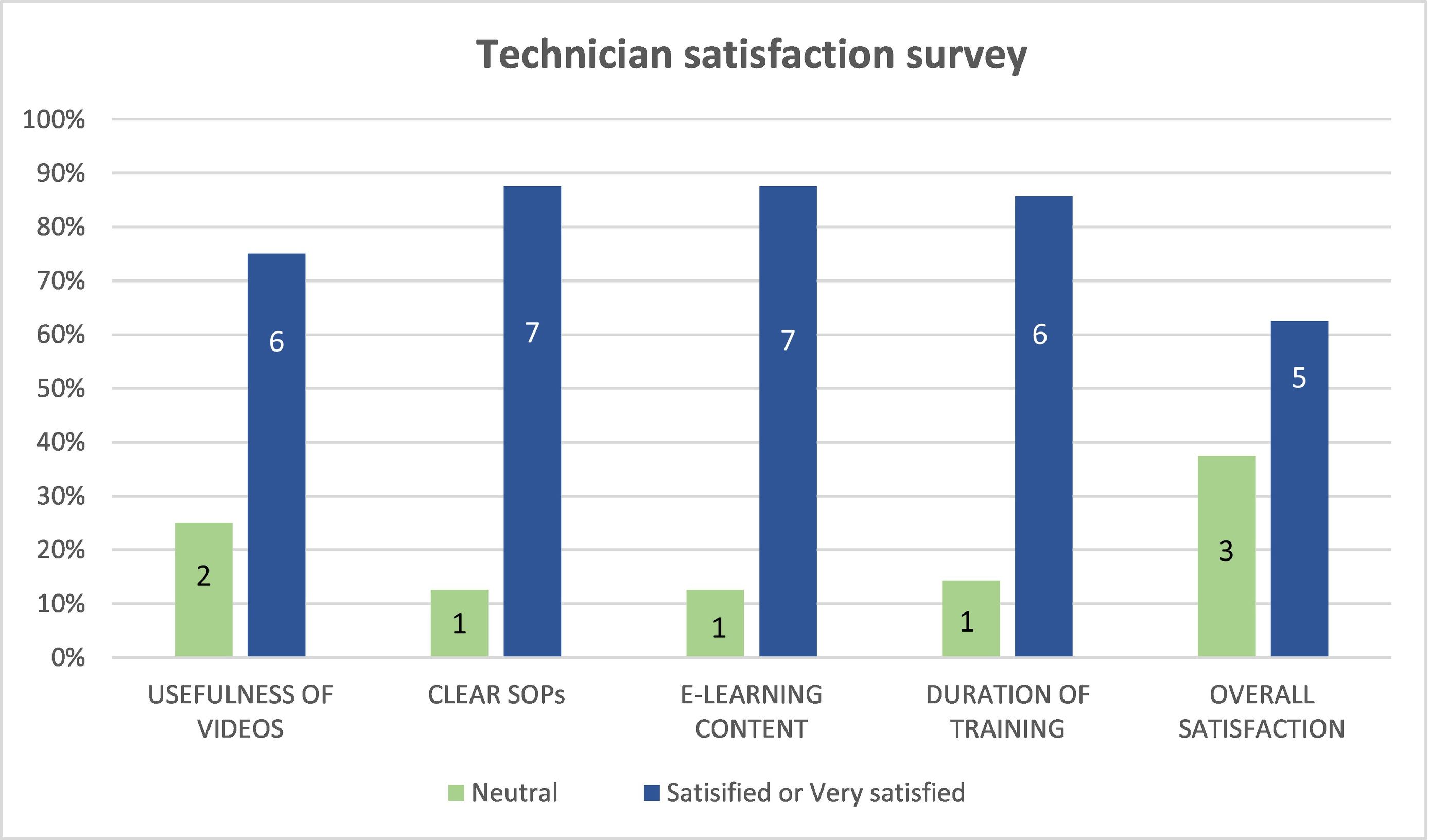
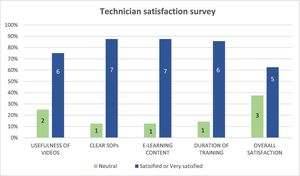
The participation rate in the satisfaction survey on training (e-learning platform) was 61.5% (n=8) out of a total number of current developers (n=13). Overall, 62.5% of technicians reported being satisfied or very satisfied, while the remaining 37.5% were indifferent.
ConclusionsCompounding training program is currently in its third year. It has been crucial in delegating tasks to pharmacy technicians. The use of digital technology is essential in this training. We consider that, specific training in compounding, is indispensable and should be included in the academic plan for pharmacy technicians.
Describir un plan de formación en elaboración de medicamentos del Servicio de Farmacia de un hospital de tercer nivel dirigido a los Técnicos Auxiliares de Farmacia utilizando una plataforma digital de formación y técnicas de simulación.
MétodosSe diseñaron dos programas de formación, uno para elaboración de medicamentos estériles y otro para no estériles. Cada programa consta de varias fases: curso básico de formación online (plataforma digital e-learning), taller práctico de simulación, prácticas tutorizadas en condiciones reales y verificación final realizada por el farmacéutico con el fin de cualificar al técnico. Ambos programas contemplan evaluación continuada y están acreditados por la Comisión de Formación Continuada del hospital.
Se diseñó y realizó una encuesta de satisfacción sobre la formación en plataforma digital e-learning dirigida a los técnicos elaboradores tanto de medicamentos estériles como no estériles.
ResultadosDurante los tres años que lleva en marcha el proyecto, seis farmacéuticos especialistas de las diferentes áreas implicadas en elaboración de medicamentos son los responsables de la formación y evaluación continuada. Se han formado 21 técnicos, de los cuales, 19 han obtenido la cualificación de elaboradores y dos han sido no aptos. En la actualidad contamos con 13 elaboradores de los inicialmente formados.
La participación global en la encuesta de satisfacción sobre la formación en plataforma e-learning fue del 61,5% (n = 8) respecto a la plantilla total de elaboradores actuales (n = 13). El grado de satisfacción global fue bueno con un 62,5% de técnicos satisfechos o muy satisfechos y el resto indiferente (37,5%).
ConclusionesEl programa de formación en elaboración de medicamentos en sus tres primeros años ha sido crucial para poder delegar las funciones de preparación de medicamentos en los técnicos de Farmacia. La utilización de tecnología digital y simulación es imprescindible en la formación. Consideramos muy necesaria una formación específica en elaboración de medicamentos en el plan de estudios académico de los Técnicos Auxiliares de Farmacia.
Medication compounding is an activity rooted in the historical origins of pharmacy, evolving alongside the profession and remaining a specialised task primarily entrusted to pharmacists. This technical endeavour has a clear clinical purpose, providing significant added value to the pharmacist's role in areas demanding personalised pharmacotherapy. To conduct this function, it is essential to adapt and delegate such activities to non-pharmaceutical professionals, such as pharmacy technical assistants (PTAs), who have intermediate-level academic training. Pharmacists are responsible for providing training in pharmacotechnics to qualify PTAs as medication compounders, thereby ensuring the optimal quality, efficacy, and safety of the medications produced.
Until March 2020, nursing staff performed medication compounding in our hospital pharmacy service (PS). They were responsible formedication compounding, including the preparation of both sterile and non-sterile medications. With the onset of the COVID-19 pandemic coincided with a period of change in PSs, there wasa gradual replacement of nursing and auxiliary staff with pharmacy technical staff. This transition was made in accordance with the Resolution of the Autonomous Community of Madrid, published in 2017, which mandated the incorporation of the professional category of PTA in health centres under the jurisdiction of the Madrid health service. Due to the pandemic,nurses were assigned to clinical units dedicated to the care of patients with COVID-19. To address this situation, we established a training program in medication compounding, aiming for PTAs to fully assume this activity. Hence, a schedule was established, initially involving the participation of the nursing staff. As PTAs underwent training, the nurses were assigned to the clinical units.
The curriculum for PTAs is regulated by Royal Decree (RD) 1689/2007, which establishes the title of Pharmacy and Parapharmacy Technician and sets out the minimum training requirements. Article 10 outlines the professional modules of basic laboratory operations (0103) and magistral preparation (0104).1
The curriculum for the intermediate-level training cycle leading to the title of Pharmacy and Parapharmacy Technician is set out in Provision 13249 of the BOE (Official State Gazette) no. 192 (2009) of the Ministry of Education Order EDU/2184/20092 and in DECREE 13/2009 for the Community of Madrid.3
The main objective of this article is to describe a training program that qualifies PTAs as medication compounders in the PS of a tertiary hospital using a digital training platform and simulation techniques. The secondary objective is to report on the level of satisfaction among the PTAs who completed the training.
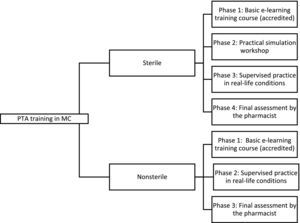
MethodsThe training of PTAs in medication compounding is divided into two programs: sterile and non-sterile compounds. The design and development of each training program are detailed in the standard operating procedures (SOPs) of our PS: “Technician training in sterile compounding” and “Technician training in non-sterile compounding”. Technicians undergo initial training in sterile compounding, and upon successful completion, some of them move on to training in non-sterile medication compounding.
Accreditation for both training programmes is provided by the hospital's Nursing Continuing Education Commission. This accreditation is applicable to both PTAs and teaching pharmacists.
Theoretical training is delivered through the e-learning platform of our PS. This proprietary platform which is accessible to all staff members via personal passwords. The platform includes training videos, a library of written procedures and training materials, recorded sessions, and evaluation questionnaires. Pharmacists in each specific area contribute essential training content to the platform as a basis for conducting tasks.
Online PTA training is highly valuable as it ensures uniformdelivery of the same concepts to all new staff, eliminating interference between outgoing and incoming staff. This guarantees that each staff member receives uniform training from the pharmacist responsible for the specific area (see Fig. 1).
Training programme in sterile medication compoundingThis program involves compounding of cytostatics, parenteral nutrition, non-cytostatic hazardous medicinal products, and other sterile compounds, such as intravenous mixtures and ophthalmic preparations.
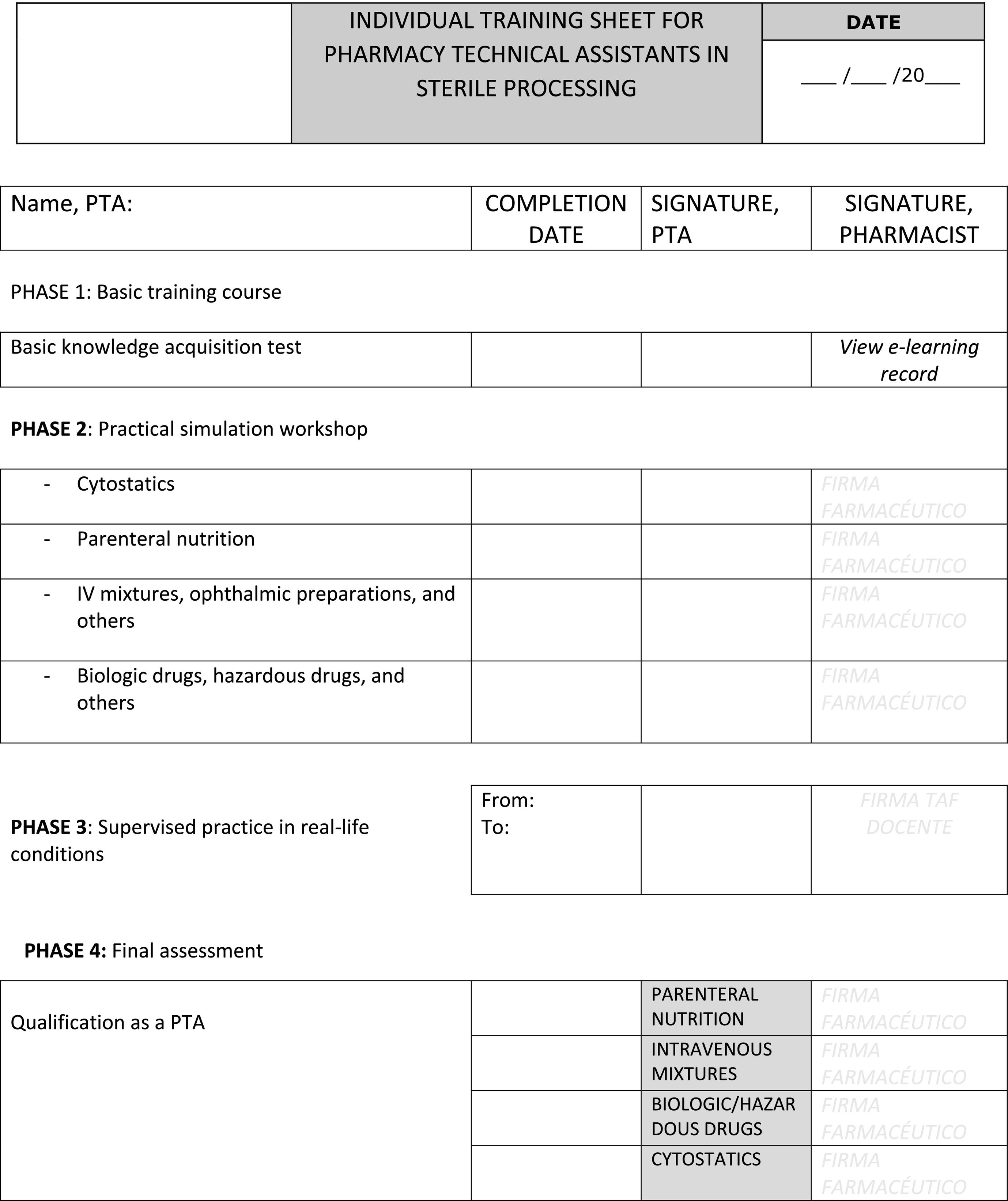
The program consists of four training phases designed to qualify individuals as a medication compounder: an online training course integrated into the e-learning digital platform; a practical simulation workshop; supervised practice in real-life conditions; and a final assessment by the pharmacist.
- 1.
Phase 1 involves a two-day basic e-learning training course at the PS library with individual computer access. During this phase, the PTAs have personalised access to the service's e-learning digital training platform, where they study the SOPs of the preparation area and watch training videos on handling sterile medications. An evaluation test is conducted on the last day to assess the knowledge acquired. The PTAs also have unrestricted access to the platform for clarifying and reinforcing their knowledge.
- 2.
Phase 2. The PTAs participate in a practical simulation workshop. Initially, the workshop was run by the pharmacists responsible for each area. Later, a PTA trainer role was createdto oversee workshop training under pharmacist supervision. Training is conducted in groups of no more than three individuals over four days organised by specific area.
- 3.
Phase 3. The PTAs receive individual supervised practice in real-life compounding scenarios. The initial training is conducted by nursing staff but qualified PTAs subsequently lead to training. The training focuses on foundational activities, as determined by the pharmacist in each area, and lasts for a 4-week period. The responsible pharmacist also monitors techniques and handling.
- 4.
Phase 4. A practical examination is performed by the pharmacist to assess and qualify the PTA.
Each PTA's training is recorded on an individual training sheet (see Annex 1), which is dated and signed by each of the corresponding pharmacist. Oncethe PTA is qualified, continuous assessment is conducted on an ongoing basis, initially monthly for the first 6 months, and bimonthly thereafter. The continuous assessment data are also recorded on the individual training sheet.
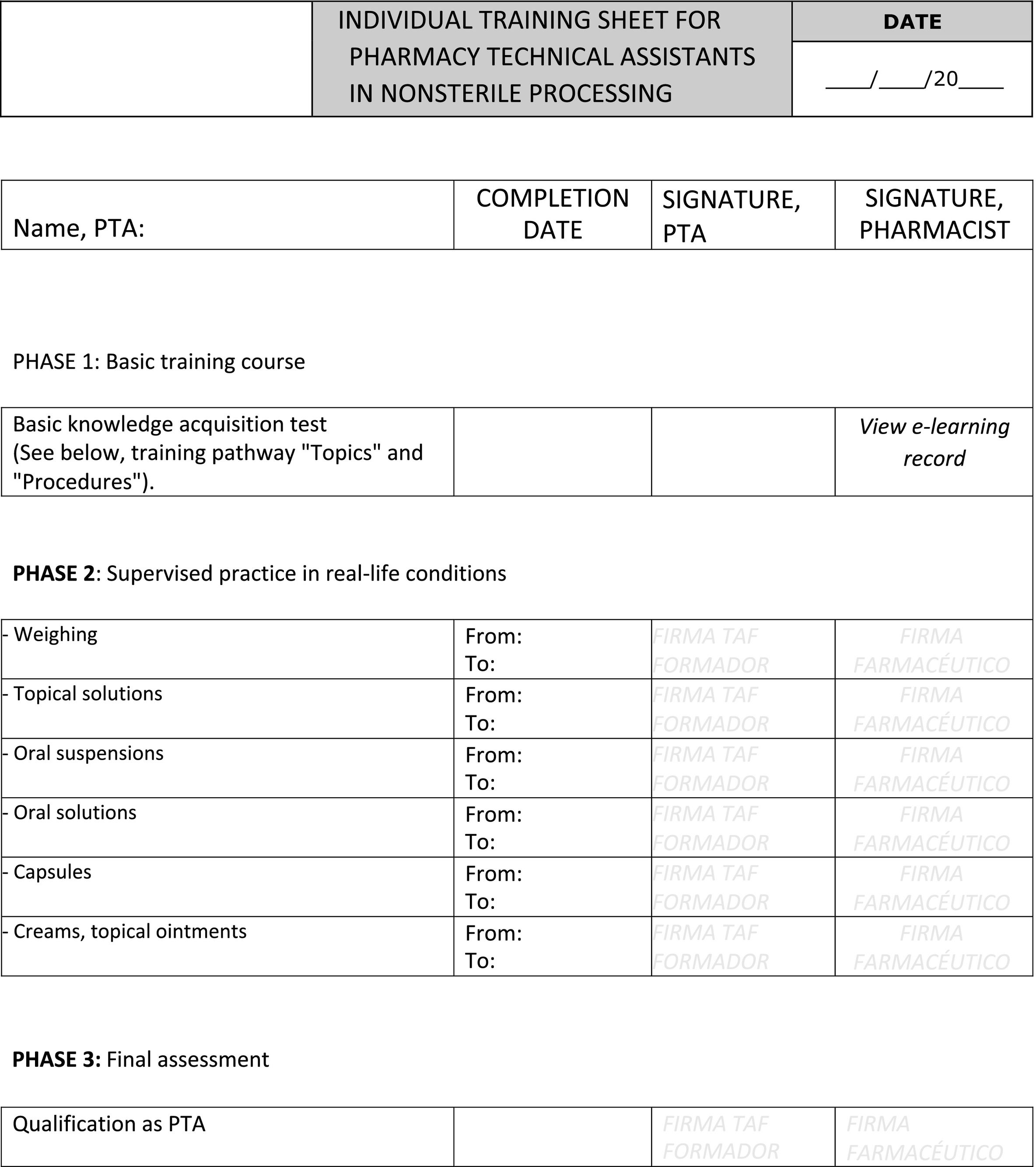
Training programme in non-sterile medication compoundingThis program is structured in 3 phases.
- 1.
Phase 1 involves an e-learning training course integrated within the digital platform. The PTAs study the online training course modules on basic PS processes, including non-sterile preparations, which are hosted on the TECNIFARMH platform4 of the SEFH (Spanish Society of Hospital Pharmacy) and pharmacotechnical procedures. An evaluation test is conducted on the final day to assess the knowledge acquired. The PTAs have unrestricted access to the platform whenever they need to resolve questions.
- 2.
Phase 2. Supervised practice in real-life conditions over a 4-week period in the PS pharmacotechnical laboratory.
- 3.
Phase 3. A practical examination administered by the pharmacist to assess and qualify the PTA as a non-sterile medication compounder.
Non-sterile medication compounding training does not include a simulation workshop, This isbecause the PTA trainees have already successfully qualified as a sterile medication compounders and demonstrated the necessary skills and techniques needed to progress to the next phase. However, practical training in real-life conditions includes full-time personalised supervision during each working day.
After the PTA is qualified, continuous assessment is conducted on an ongoing basis. The assessment is conducted monthly for the first 6 months, and bimonthly thereafter.
Each PTA's training is recorded on an individual training sheet (see Annex 2), which is dated and signed by the corresponding pharmacist.
In April 2023, 3 years after the start of the training program, a satisfaction survey for both sterile and non-sterile medication compounders was developed and administered over the e-learning digital platform (Annex 3).
The questionnaire comprised 5 questions scored on a scale of 1–5 (1=very dissatisfied, 2=dissatisfied, 3=neither satisfied nor dissatisfied, 4=satisfied, 5 = very satisfied), and Yes/No + DK/NR (Don't Know/No Response).
ResultsSince the implementation of the training program, six pharmacists specialising in different areas of medication compounding in the PS have been responsible for the training and continuous assessing the PTAs. In total, 21 PTAs have undergone training: 19 individuals (90.5%) obtained the qualification in sterile compounding, whereas 2 individuals (9.5%) did not meet the requirements. Of the 19 qualified PTAs, nine were selected for training in non-sterile compounding.
Three years after the start of the training program, a training satisfaction survey was conducted over the e-learning platform. At that time, there were 13 PTAs in the compounding staff, with 4 of them on sick leave. The survey results of the interviewees were as follows:
- -
The overall participation rate was 61.5% (n=8) of the total number of fully trained PTA compounders. The participation rate was 88.9% (n=9) of the PTAs active at the time of the survey.
- -
The overall level of satisfaction was good with 62.5% (n=5) of PTAs expressing satisfaction or being very satisfied, 37.5% (n=3) indicating a neutral opinion.No respondents expressed dissatisfaction.
- -
The provision of the basic tools needed to fulfil tasks on the e-learning platform was awarded the highest level of satisfaction (88%) (n=7), followed by clear working procedures (88%) (n=7).
- -
The lowest rating was achieved on usefulness of the videos; nevertheless, satisfaction was good (75%) (n=6).
- -
All respondents (100%; n=8) consulted the e-learning platform before starting work, and 37.5% (n=3) also consulted it during their work period. The PTAs who consulted the e-learning platform both before work and during the working period reported higher satisfaction (100%), in contrast to the PTAs who only consulted it before starting work (neutral rating: 66%).
Fig. 2 shows the overall results of the survey.
This article describes a 3-year training programme for PTAs in medication compounding at a tertiary-level hospital in the Community of Madrid. The programme was implemented in 2020 and has continuedto the present day. Initially, this project was a challenge requiring a very rapid response within a narrow time-window, due to the urgent circumstances of the COVID-19 pandemic at that time.
The program was implemented in May 2020, and by October of the same year, integrated into the service's digital e-learning platform. Currently, our PS has 57 PTAs, with 13 individuals (23%) being members of the medication compounding group.
Training the PTAs presented a challenge to the PS, as it was, and still is essential to train all new technicians joining the service. The digital e-learning platform is a very helpful tool, particularly given the high turnover of technical staff. This online platform ensures consistent training for all new technical staff, avoiding interference between outgoing and incoming staff.It guarantees that all newcomers receive consistent training supervision by the pharmacist responsible for the specific area. The platform provides added value by allowing free access at any time to any PTA who wishes to consult the information contained on the platform.
The successful completion of this project is due to the additional effort and involvement of both the nursing staff and the pharmacists responsible for pharmacotechnics. The main challenge of the project, both at the beginning and currently, is the limited or lack of training in medication compounding among PTAs joining the service.
A further significant challenge arises from frequent staff turnover between other hospitals within the same Autonomous Community and those in other Autonomous Communities. Currently, only 68% of the originally trained staff remain on our team, Therefore, a great deal of effort and time has been invested in training PTAs who did not remain in our PS.
Pending issues include the need for a project manager responsible for the platform by updating essential videos, incorporating new procedures, managing potential changes, and other platform-related tasks.
This platform also certifies that PTAs have undergone initial training. However, it requires regular updates, which necessitates the continuing education of PTAs over time.
In addition, when a technician joins the service and requires training, both the pharmacist and the technician must invest time in the training process, which contributes to the burden of care overload.
In our opinion, the current academic training of PTAs may not adequately meet the needs of hospital-pharmacy services, particularly in regards to medication compounding. As a result, medical staff have to invest substantial effort to ensure that the technicians receive the necessary training in this regard. This process includes designing and implementing a training program, supervising the PTAs, overseeing their final training, and continously evaluating their perfomance to ensure the quality of the medicines compounded in our PS.
In Spain, initiatives of this type have been developed at the national-level by the TECNIFARMH coordinating group of the SEFH, whose online PTA training program includes courses on non-sterile preparations, sterile preparation for healthcare support personnel, parenteral nutrition, and compounding cytostatics. One of the overall aims of this project is to petition the Spanish Ministry of Education to create the qualification of Técnico Superior de Farmacia Hospitalaria (Hospital Pharmacy Technical Assistant).5
Likewise, similar initiatives have been developed at the local-level, such as the Hospital Pharmacy course organised by the corresponding service at the Reina Sofia Hospital (Cordoba, Spain). To provide more specialised training, this course is aimed at the staff who deliver training to pharmacy and parapharmacy technicians.6
Our initiative differs from other hospitals programs as it is based on the use of new technologies, such as our proprietary platform and simulation techniques. This makesour training more practical and less theoretical.It also ensures the continuing training of PTAs and free access to information on the platform at any time.
The participation of hospital pharmacists in the training of PTAs, starting from the curricula, is an investment in the future to ensure the proper functioning of the HPS. To ensure the quality of compounded medicines, the proactive delegation and adaptation of compounding functions are needed, while acknowledging that this activity has traditionally defined the hospital pharmacy collective.
Contribution to the scientific literatureThis article presents an accredited training program in sterile and non-sterile medication compounding for pharmacy technical assistants. Such training is crucial for effectively conducting one of the fundamental activities within hospital pharmacy services. The successful implementation of this project has enabled the delegation of medication compounding to the pharmacy technical assistants in our pharmacy service, ensuring the optimal quality, efficacy, and safety of the compounded medications.
A novel contribution is the use of a digital platform and simulation techniques in real-life conditions to achieve uniform training for all the personnel involved in medication compounding.
We are of the opinion that this project could prove useful to other PSs facing situations that are similar to ours.
Ethical responsibilitiesNot applicable.
FundingNone declared.
Statement of authorshipFátima Ros Castellar: Design of the training program; trainer responsible for the preparation of non-sterile and sterile medicines (such as intravenous mixtures and ophthalmic preparations); conception, design, and writing of the article.
Margarita Ruano Encinar: Design and implementation of the satisfaction survey on training on the e-learning digital platform; review of the article.
Tamara Pérez Robles: Design of the training program; trainer responsible for the preparation of hazardous noncytostatic and biological medicines; review of the article.
Natalia García Vázquez: Design of the training program; trainer responsible for parenteral nutrition compounding; review of the article.
Gema Casado Abad: Trainer responsible for the preparation of cytostatic medicines; review of the article.
Luis Sánchez-Rubio: Trainer responsible for cytostatic medication compounding; review of the article.
MilusKa yamil Rabanal Sánchez: Trainer in medication compounding; review of the article.
Alicia Herrero Ambrosio: Critical review with relevant intellectual contributions.
The authors would like to thank Elena Gómez del Pulgar, Laura Sanz, and all the nursing and pharmacy technician staff for their collaboration in the project.