Most cytostatic drugs cannot be administered directly to patients in their marketed presentation, but require previous reconstitution conducted in the Pharmacy Unit areas for cytostatic preparation.
There are systems that allow drug reconstitution and transfer once it has been diluted, in order to protect staff from any potential contamination during handling. These are commonly known as Closed Systems, and generally have a piece for vial attachment and a syringe adapter with a built-in filter, that replace the traditional needles. Closed systems feature different characteristics and costs which is necessary to analyze in order to determine the most efficient one.
La mayoría de fármacos citostáticos no pueden ser administrados directamente desde la presentación comercial al paciente, sino que requieren de una reconstitución previa realizada en las áreas de elaboración de citostáticos en los Servicios de Farmacia.
Existen sistemas que permiten reconstituir y extravasar el fármaco una vez diluido, para evitar la posible contaminación derivada de su manejo al personal. Estos sistemas se conocen comúnmente como sistemas cerrados, y de manera genérica constan de una pieza de fijación al vial y un adaptador para la jeringa con filtro integrado, que sustituyen a las tradicionales agujas. Los sistemas cerrados presentan diversas características y costes que son necesarios analizar para conocer cuál es el sistema más eficiente.
Occupational safety has become one of the main concerns in hospitals, and exposure to cytotoxic agents is one of the most relevant issues, as well as accidental needle-sticks. Since the 70s, it has been well known that nurses who prepare chemotherapy presented high levels of mutagenic agents in their bodies1. Therefore, there have been many guidelines and agreement documents2,10 prepared in order to try to minimize the exposure of workers to this type of agents3. One of the first advances in this field was the use of biological safety cabinets in combination with individual protection equipment, and the use of closed systems for preparation and transfer of antineoplastic agents4, according to Royal Decree (RD 665/97) which was subsequently modified (RD 1124/2000 and RD 349/2003)5,6. This Royal Decree regulates closed systems and therefore encourages their use, and sophisticated systems have been launched that will replace the use of traditional needles. These complex devices present heterogeneous costs that require their cost-efficiency assessment7. The Pharmacy Area is legally responsible for this assessment (RD 1591/2009)8, which will allow to select the most efficient devices. In order to conduct this assessment, it will be essential to consider that the increased safety offered for cytostatic handling by these Closed Systems (CS) is obtained at the expense of dead space, higher than that of traditional loading needles, which does not allow the total extraction of the liquid contents from the vials9. Therefore, in this study we have analyzed the potential economic impact of incorporating each one of these systems in a third-level hospital; additionally, a cost-efficiency study has been conducted for said devices, based on the most efficient use of the vials.
MethodsA study was conducted with the objective of measuring the cost-efficiency of some of the CS available in the market. The following CS were assessed:
BD-Phaseal®; Hospira ICU CLAVE® CH 70 and CH74; Baxter-ChemoAIDE®; Care Fusion Smart Site® and VM04®; Fresenius Extra Spike®; Braun Chemo V Mini Spike®.
These systems include, among other features, an awl that allows to pierce the rubber septum of each vial, remaining affixed through anchorage. They also allow to access the vial contents through a luer connector to the syringe, not requiring the use of needles. All these systems feature 0.2 μm venting filters in all their models, except for BD Phaseal, which features an airtight expansion chamber.
The calculation of the estimated economic impact for one year included:
- –
The cost associated with the loss of the drug that remains in the system. To this aim, the outcomes from the study were extrapolated with each vial size and CS model included, shown in table 1, to the vials used during one year in our hospital, in the Day Hospital areas for Oncology and Haematology.
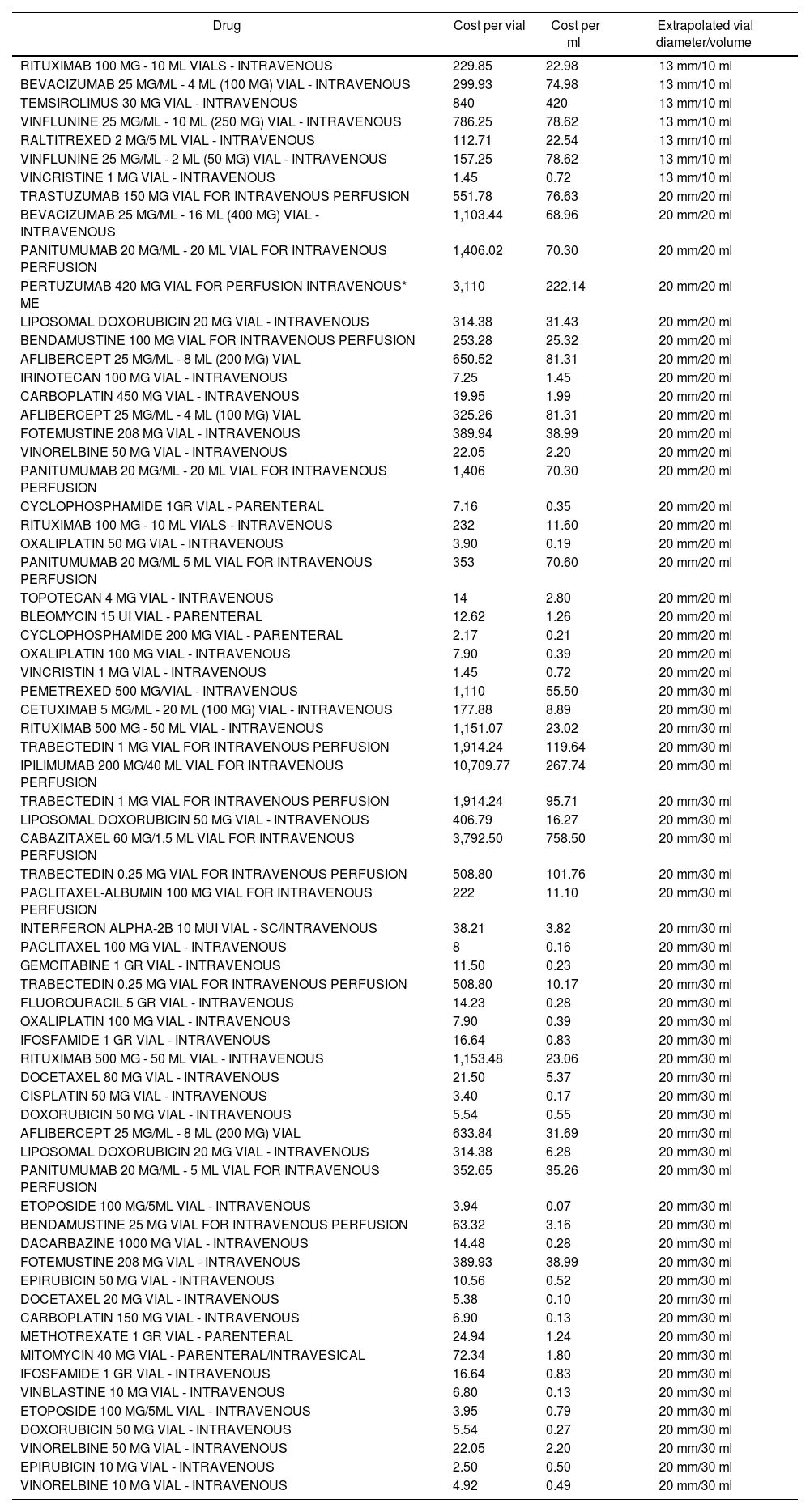
Table 1.Classification of the marketed presentations used in Oncology and Haematology Day Hospitals in 2014
Drug Cost per vial Cost per ml Extrapolated vial diameter/volume RITUXIMAB 100 MG - 10 ML VIALS - INTRAVENOUS 229.85 22.98 13 mm/10 ml BEVACIZUMAB 25 MG/ML - 4 ML (100 MG) VIAL - INTRAVENOUS 299.93 74.98 13 mm/10 ml TEMSIROLIMUS 30 MG VIAL - INTRAVENOUS 840 420 13 mm/10 ml VINFLUNINE 25 MG/ML - 10 ML (250 MG) VIAL - INTRAVENOUS 786.25 78.62 13 mm/10 ml RALTITREXED 2 MG/5 ML VIAL - INTRAVENOUS 112.71 22.54 13 mm/10 ml VINFLUNINE 25 MG/ML - 2 ML (50 MG) VIAL - INTRAVENOUS 157.25 78.62 13 mm/10 ml VINCRISTINE 1 MG VIAL - INTRAVENOUS 1.45 0.72 13 mm/10 ml TRASTUZUMAB 150 MG VIAL FOR INTRAVENOUS PERFUSION 551.78 76.63 20 mm/20 ml BEVACIZUMAB 25 MG/ML - 16 ML (400 MG) VIAL - INTRAVENOUS 1,103.44 68.96 20 mm/20 ml PANITUMUMAB 20 MG/ML - 20 ML VIAL FOR INTRAVENOUS PERFUSION 1,406.02 70.30 20 mm/20 ml PERTUZUMAB 420 MG VIAL FOR PERFUSION INTRAVENOUS* ME 3,110 222.14 20 mm/20 ml LIPOSOMAL DOXORUBICIN 20 MG VIAL - INTRAVENOUS 314.38 31.43 20 mm/20 ml BENDAMUSTINE 100 MG VIAL FOR INTRAVENOUS PERFUSION 253.28 25.32 20 mm/20 ml AFLIBERCEPT 25 MG/ML - 8 ML (200 MG) VIAL 650.52 81.31 20 mm/20 ml IRINOTECAN 100 MG VIAL - INTRAVENOUS 7.25 1.45 20 mm/20 ml CARBOPLATIN 450 MG VIAL - INTRAVENOUS 19.95 1.99 20 mm/20 ml AFLIBERCEPT 25 MG/ML - 4 ML (100 MG) VIAL 325.26 81.31 20 mm/20 ml FOTEMUSTINE 208 MG VIAL - INTRAVENOUS 389.94 38.99 20 mm/20 ml VINORELBINE 50 MG VIAL - INTRAVENOUS 22.05 2.20 20 mm/20 ml PANITUMUMAB 20 MG/ML - 20 ML VIAL FOR INTRAVENOUS PERFUSION 1,406 70.30 20 mm/20 ml CYCLOPHOSPHAMIDE 1GR VIAL - PARENTERAL 7.16 0.35 20 mm/20 ml RITUXIMAB 100 MG - 10 ML VIALS - INTRAVENOUS 232 11.60 20 mm/20 ml OXALIPLATIN 50 MG VIAL - INTRAVENOUS 3.90 0.19 20 mm/20 ml PANITUMUMAB 20 MG/ML 5 ML VIAL FOR INTRAVENOUS PERFUSION 353 70.60 20 mm/20 ml TOPOTECAN 4 MG VIAL - INTRAVENOUS 14 2.80 20 mm/20 ml BLEOMYCIN 15 UI VIAL - PARENTERAL 12.62 1.26 20 mm/20 ml CYCLOPHOSPHAMIDE 200 MG VIAL - PARENTERAL 2.17 0.21 20 mm/20 ml OXALIPLATIN 100 MG VIAL - INTRAVENOUS 7.90 0.39 20 mm/20 ml VINCRISTIN 1 MG VIAL - INTRAVENOUS 1.45 0.72 20 mm/20 ml PEMETREXED 500 MG/VIAL - INTRAVENOUS 1,110 55.50 20 mm/30 ml CETUXIMAB 5 MG/ML - 20 ML (100 MG) VIAL - INTRAVENOUS 177.88 8.89 20 mm/30 ml RITUXIMAB 500 MG - 50 ML VIAL - INTRAVENOUS 1,151.07 23.02 20 mm/30 ml TRABECTEDIN 1 MG VIAL FOR INTRAVENOUS PERFUSION 1,914.24 119.64 20 mm/30 ml IPILIMUMAB 200 MG/40 ML VIAL FOR INTRAVENOUS PERFUSION 10,709.77 267.74 20 mm/30 ml TRABECTEDIN 1 MG VIAL FOR INTRAVENOUS PERFUSION 1,914.24 95.71 20 mm/30 ml LIPOSOMAL DOXORUBICIN 50 MG VIAL - INTRAVENOUS 406.79 16.27 20 mm/30 ml CABAZITAXEL 60 MG/1.5 ML VIAL FOR INTRAVENOUS PERFUSION 3,792.50 758.50 20 mm/30 ml TRABECTEDIN 0.25 MG VIAL FOR INTRAVENOUS PERFUSION 508.80 101.76 20 mm/30 ml PACLITAXEL-ALBUMIN 100 MG VIAL FOR INTRAVENOUS PERFUSION 222 11.10 20 mm/30 ml INTERFERON ALPHA-2B 10 MUI VIAL - SC/INTRAVENOUS 38.21 3.82 20 mm/30 ml PACLITAXEL 100 MG VIAL - INTRAVENOUS 8 0.16 20 mm/30 ml GEMCITABINE 1 GR VIAL - INTRAVENOUS 11.50 0.23 20 mm/30 ml TRABECTEDIN 0.25 MG VIAL FOR INTRAVENOUS PERFUSION 508.80 10.17 20 mm/30 ml FLUOROURACIL 5 GR VIAL - INTRAVENOUS 14.23 0.28 20 mm/30 ml OXALIPLATIN 100 MG VIAL - INTRAVENOUS 7.90 0.39 20 mm/30 ml IFOSFAMIDE 1 GR VIAL - INTRAVENOUS 16.64 0.83 20 mm/30 ml RITUXIMAB 500 MG - 50 ML VIAL - INTRAVENOUS 1,153.48 23.06 20 mm/30 ml DOCETAXEL 80 MG VIAL - INTRAVENOUS 21.50 5.37 20 mm/30 ml CISPLATIN 50 MG VIAL - INTRAVENOUS 3.40 0.17 20 mm/30 ml DOXORUBICIN 50 MG VIAL - INTRAVENOUS 5.54 0.55 20 mm/30 ml AFLIBERCEPT 25 MG/ML - 8 ML (200 MG) VIAL 633.84 31.69 20 mm/30 ml LIPOSOMAL DOXORUBICIN 20 MG VIAL - INTRAVENOUS 314.38 6.28 20 mm/30 ml PANITUMUMAB 20 MG/ML - 5 ML VIAL FOR INTRAVENOUS PERFUSION 352.65 35.26 20 mm/30 ml ETOPOSIDE 100 MG/5ML VIAL - INTRAVENOUS 3.94 0.07 20 mm/30 ml BENDAMUSTINE 25 MG VIAL FOR INTRAVENOUS PERFUSION 63.32 3.16 20 mm/30 ml DACARBAZINE 1000 MG VIAL - INTRAVENOUS 14.48 0.28 20 mm/30 ml FOTEMUSTINE 208 MG VIAL - INTRAVENOUS 389.93 38.99 20 mm/30 ml EPIRUBICIN 50 MG VIAL - INTRAVENOUS 10.56 0.52 20 mm/30 ml DOCETAXEL 20 MG VIAL - INTRAVENOUS 5.38 0.10 20 mm/30 ml CARBOPLATIN 150 MG VIAL - INTRAVENOUS 6.90 0.13 20 mm/30 ml METHOTREXATE 1 GR VIAL - PARENTERAL 24.94 1.24 20 mm/30 ml MITOMYCIN 40 MG VIAL - PARENTERAL/INTRAVESICAL 72.34 1.80 20 mm/30 ml IFOSFAMIDE 1 GR VIAL - INTRAVENOUS 16.64 0.83 20 mm/30 ml VINBLASTINE 10 MG VIAL - INTRAVENOUS 6.80 0.13 20 mm/30 ml ETOPOSIDE 100 MG/5ML VIAL - INTRAVENOUS 3.95 0.79 20 mm/30 ml DOXORUBICIN 50 MG VIAL - INTRAVENOUS 5.54 0.27 20 mm/30 ml VINORELBINE 50 MG VIAL - INTRAVENOUS 22.05 2.20 20 mm/30 ml EPIRUBICIN 10 MG VIAL - INTRAVENOUS 2.50 0.50 20 mm/30 ml VINORELBINE 10 MG VIAL - INTRAVENOUS 4.92 0.49 20 mm/30 ml - –
The cost of the syringes for cytostatic preparations (attached to the CS for handling during preparation).
- –
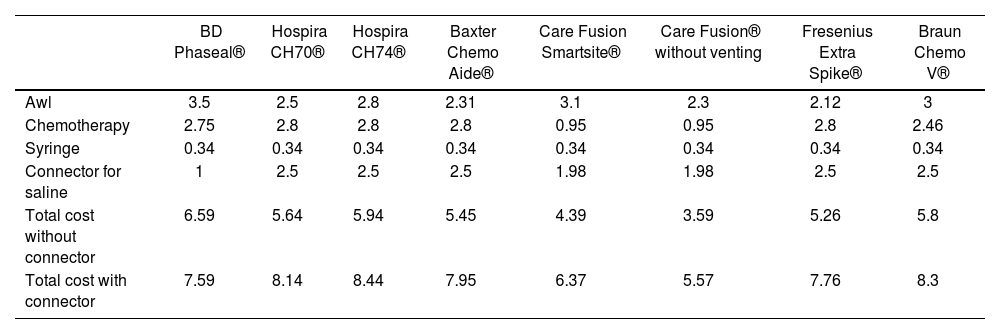
The costs of the CS available at the time of conducting the study (Table 3).
Table 3.Breakdown of the costs of CS by components
BD Phaseal® Hospira CH70® Hospira CH74® Baxter Chemo Aide® Care Fusion Smartsite® Care Fusion® without venting Fresenius Extra Spike® Braun Chemo V® Awl 3.5 2.5 2.8 2.31 3.1 2.3 2.12 3 Chemotherapy 2.75 2.8 2.8 2.8 0.95 0.95 2.8 2.46 Syringe 0.34 0.34 0.34 0.34 0.34 0.34 0.34 0.34 Connector for saline 1 2.5 2.5 2.5 1.98 1.98 2.5 2.5 Total cost without connector 6.59 5.64 5.94 5.45 4.39 3.59 5.26 5.8 Total cost with connector 7.59 8.14 8.44 7.95 6.37 5.57 7.76 8.3
The cost of drug loss was estimated through the weight difference technique. The procedure was conducted as follows:
- a.
Empty 10, 20 and 30 ml vials were weighed.
- b.
Vials were filled with an innocuous and coloured solution, with the respective volumes (10, 20 and 30 mL).
- c.
Each CS model was attached, according to size, to the relevant vial.
- d.
Liquid extraction was conducted through each one of the CS.
- e.
Each vial was weighed once its liquid contents had been extracted. We applied the weight difference technique regarding the initial weight of the empty vial.
This process was conducted three times by three different operators, with the objective of avoiding any bias caused by the level of skill in the use of these systems: Operator 1: with high experience in cytostatic preparation, conducted in his daily practice, wide knowledge of CS; Operator 2: limited experience, with knowledge of the mechanism and performance, and occasionally handling these preparation materials; and Operator 3, without any experience, with knowledge of the mechanism and performance of CS.
The mean level of the 3 measurements was taken as reference. This specific value for each vial size and CS model was considered as drug loss in ml.
The vials of the marketed presentations of drugs used in Oncology and Haematology were classified into 3 groups, according to their diameter size and volume: 13 mm/10 mL, 20 mm/20 mL and 20 mm/30 mL (Table 1); this allowed to extrapolate the loss of the drug discarded in the vial represented by the use of each CS model, through calculating the cost per drug ml, using the price reported at the date of the study, on February, 2015.
The number of total preparations was obtained from the Oncowin® computer system, and the use of vials from SAP®.
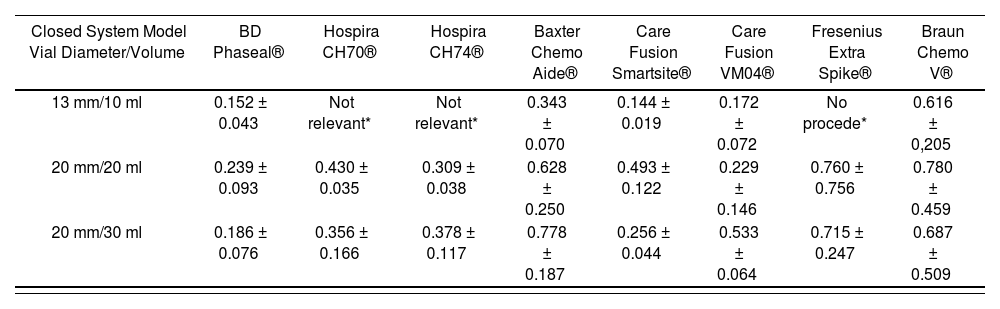
ResultsIn total, there were 63 tests through difference in weight, with each vial size and CS model measured three times, and the mean level of drug not used in each of the three measurements was used as value of reference. These systems were not available to us; Hospira ICU CLAVE® CH 70, CH74, or Fresenius Extra Spike® for the 10ml vial size. The outcomes are stated in table 2.
Volume (ml) of drug lost during the preparation process
| Closed System Model Vial Diameter/Volume | BD Phaseal® | Hospira CH70® | Hospira CH74® | Baxter Chemo Aide® | Care Fusion Smartsite® | Care Fusion VM04® | Fresenius Extra Spike® | Braun Chemo V® |
|---|---|---|---|---|---|---|---|---|
| 13 mm/10 ml | 0.152 ± 0.043 | Not relevant* | Not relevant* | 0.343 ± 0.070 | 0.144 ± 0.019 | 0.172 ± 0.072 | No procede* | 0.616 ± 0,205 |
| 20 mm/20 ml | 0.239 ± 0.093 | 0.430 ± 0.035 | 0.309 ± 0.038 | 0.628 ± 0.250 | 0.493 ± 0.122 | 0.229 ± 0.146 | 0.760 ± 0.756 | 0.780 ± 0.459 |
| 20 mm/30 ml | 0.186 ± 0.076 | 0.356 ± 0.166 | 0.378 ± 0.117 | 0.778 ± 0.187 | 0.256 ± 0.044 | 0.533 ± 0.064 | 0.715 ± 0.247 | 0.687 ± 0.509 |
It was observed that the CS with the best efficient use of the drug in 10ml vials was the system marketed by Care Fusion Smartsite®, with a mean loss of 0.144 ± 0.019 mL, followed by BD-Phaseal® with 0.152 ± 0.433 ml; the system with the highest loss was Braun's Awl, with 0.661 ± 0.205 mL.
For the 20 mL vial size, the device by Care Fusion® model VM04 allowed the most efficient use of the vial contents (0.229 ± 0.146 mL), followed by BD-Phaseal® with a 0.239 ± 0.093ml loss; the device by Braun® presented the highest recorded loss (0.780 ± 0.459 mL).
For 30 mL vials, the BD-Phaseal® system showed the best results (0.186 ± 0.760 mL), followed by the Care Fusion Smarthsitesystem with 0.256 ± 0.044 mL.
The estimated cost that these losses would represent for the hospital was calculated based on the preparations conducted during 2014 for the Oncology and Haematology Units. In total, 71 different commercial presentations were used, classified by vial size and diameter into 3 groups, as appears in table 1.
During this period, 34,598 cytostatic preparations were conducted in total, using 16,788 vials.
In terms of the different CS models used, the detailed cost was the one available at the time of the study. Table 3 shows the breakdown of these costs by components: chemotherapy, awl, and adapter to the infusion system.
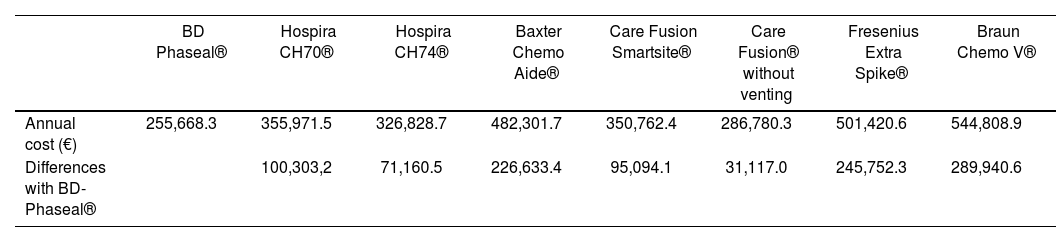
The economic impact represented by the use of each CS model during one year in a third level hospital included the cost of the drug loss, the remains that were not used in each marketed vial, and the cost of CS. The outcomes of this analysis appear in table 4: we consider that the most efficient CS model would be BD-Phaseal®, with a cost of 255.668,3 €/ year. On the other hand, according to our study, the Braun® model would be considered the least efficient, with an impact of 544,808,9 €/year.
Annual economic impact derived of the use of each Closed System
| BD Phaseal® | Hospira CH70® | Hospira CH74® | Baxter Chemo Aide® | Care Fusion Smartsite® | Care Fusion® without venting | Fresenius Extra Spike® | Braun Chemo V® | |
|---|---|---|---|---|---|---|---|---|
| Annual cost (€) | 255,668.3 | 355,971.5 | 326,828.7 | 482,301.7 | 350,762.4 | 286,780.3 | 501,420.6 | 544,808.9 |
| Differences with BD-Phaseal® | 100,303,2 | 71,160.5 | 226,633.4 | 95,094.1 | 31,117.0 | 245,752.3 | 289,940.6 |
Closed Systems have been gradually incorporated in Pharmacy Units, due to the recommendations by our current legislation (RD1591/2009).
One of the main drawbacks for their implementation has been their high budgetary impact, as well as the current continuous innovation in this market. The objective of this study was to present an evaluation method for the efficiency of closed systems, through a cost-efficiency analysis, based on the lack of efficient use of the vials shown by these systems.
According to our data, the system with the lowest overall impact on the budget is, however, the one with the highest cost of purchase: the system marketed by BD-Phaseal®; the essential reason for this is that it allows a most efficient use of the drug vials, almost 15% higher than the mean of the other CS.
It is true that this is not the only characteristic that must be assessed at the time of incorporating a new healthcare technology. In fact, this is one of the limitations in our study, which is simply based on cost aspects derived of the purchase of systems and the efficient use of vials. There are even studies that have been publishediii, taking into account the time of preparation of treatments based on the CS used. Besides, currently there are rules that classify these CS into different levels of safety; among these, the BD-Phaseal® systems meet the most demanding requirements. However, we have assumed that all systems present the same sealing and safety datax, and also that there is an equivalent handling of these systems by the nursing staff. The study presented is only a tool for calculating the direct costs derived of the use of different CS. Different hospitals will be able to incorporate these analyses, if they consider them necessary for their assessment of these systems.
- Inicio
- Todos los contenidos
- Publique su artículo
- Acerca de la revista
- Métricas