To design the patient onboarding in a multidisciplinary severe asthma unit, according to the needs identified by patients and professionals in the unit.
MethodsQualitative study using the human-centred design conducted between November 2022 and February 2023. Patients and professionals from the severe asthma unit and experts in the methodology participated. Three workshops were held. In the first, we elaborated the patient experience map, identifying positive aspects and needs. Possible solutions were devised. In the second, we selected the solutions described in a previous project applicable to onboarding and determined the key moments. In the third, we finalised the definition of the key moments, the professionals in charge in each step and the tools to be incorporated. Finally, in short sessions (sprints) we developed the necessary material and infographics.
ResultsWe identified the main needs of patients (better control of the disease and autonomy in care, two-way conversation with professionals and receiving coordinated and personalised care) and professionals (defining, structuring, unifying and adapting the information provided to patients and managing to maintain open conversations with them). We determined that onboarding should establish a controlled welcome to the severe asthma unit, which is identifiable by patients, promotes the patient-professional relationship and the learning, use and functioning of the severe asthma unit.
Previously devised solutions applicable to onboarding, such as the landing kit or the patient diary, were selected. We established the key moments of onboarding (identification consultation, initial consultation, onboarding consultation and complementary consultations), the professionals involved and the necessary information, material and infographics.
Finally, we developed the design, structure and final content of the necessary tools, such as the patient diary or the asthma infographic.
ConclusionsThis work has allowed us to design, structure and standardise the onboarding, providing an environment that facilitates self-care and open, empathetic, two-way conversation between patients and professionals, according with the key needs expressed by both. These findings may be useful for other multidisciplinary care units.
Diseñar la acogida del paciente en una unidad multidisciplinar de asma grave, de acuerdo con las necesidades identificadas por pacientes y profesionales de la unidad.
MétodoEstudio cualitativo, empleando un diseño centrado en las personas, realizado entre noviembre de 2022 y febrero de 2023. Participaron pacientes y profesionales de la unidad y expertos en la metodología. Se realizaron 3 talleres: en el primero, se elaboró el mapa de experiencia del paciente, identificando aspectos positivos y necesidades, y se idearon posibles soluciones. En el segundo, se seleccionaron las soluciones descritas en un proyecto anterior aplicables a la acogida del paciente y se determinaron los momentos clave. En el tercero, se finalizó la definición de los momentos clave, los profesionales responsables y las herramientas que debe incorporar. Por último, en sesiones cortas (sprints) se desarrollaron el material y las infografías necesarias.
ResultadosSe identificaron las principales necesidades de los pacientes (mejor control de la enfermedad y autonomía en los cuidados, conversación bidireccional con los profesionales y recibir una atención coordinada y personalizada) y de los profesionales (definir, estructurar, unificar y adecuar la información proporcionada a los pacientes y lograr mantener conversaciones abiertas con ellos). Se determinó que se debía establecer una acogida controlada a la unidad, identificable por los pacientes, y que promueva la relación paciente-profesional y el aprendizaje, uso y funcionamiento de la unidad.
Se seleccionaron las soluciones previamente ideadas aplicables a la acogida del paciente, como el kit de aterrizaje o el diario del paciente. Se establecieron los momentos clave de la acogida del paciente (consulta de identificación, consulta de inicio, consulta de incorporación y consultas complementarias), los profesionales involucrados y la información y material necesario.
Finalmente, se desarrollaron el diseño, la estructura y el contenido final de las herramientas necesarias, tales como el propio diario del paciente o la infografía sobre el asma.
ConclusionesEste trabajo nos ha permitido diseñar, estructurar y estandarizar la acogida del paciente, proporcionando un entorno que facilita el autocuidado y la conversación abierta, empática y bidireccional entre pacientes y profesionales, de acuerdo con las necesidades clave expresadas por ambos. Estos hallazgos pueden ser útiles para otras unidades multidisciplinares.
Severe uncontrolled asthma (SUA) affects around 3.9% of patients with asthma.1 SUA is a complex chronic illness with a negative impact on the quality of life of patients that has been associated with a heavy healthcare burden.2 The prevalence and relevance of comorbidities, added to the emergence of new therapeutic options, have led to the establishment of multidisciplinary severe asthma teams (MDSATs) to ensure appropriate management.2,3
MDSATs have demonstrated to positively impact the management of the SUA, with a major role in healthcare, research and training.3,4 However, the operation of MDSATs entails considerable organizational complexity, as it involves streamline communication and coordination between professionals from different departments. Therefore, for MDSATs to effectively meet the needs of patients and professionals, it is essential to adopt a comprehensive and integrative design and implementation strategy.5 In this context, the MDSAT of our hospital developed the ASfarMA project.6
Our MDSAT was created in 2018 and holds certification from the Spanish Society of Allergology and Clinical Immunology (SEAIC) of the Spanish Society of Pulmonology and Thoracic Surgery (SEPAR) of the World Allergy Organization (WAO). The MDSAT involves professionals from the departments of allergology, pharmacy, immunology, pulmonology, otorhinolaryngology, pediatrics, psychiatry and radiology. Initiated in 2020, the ASfarMA project encompasses a set of innovative, person-centered measures and adopts a comprehensive approach that integrates illness, treatment, healthcare delivery, and perceived quality, with the overarching aim of improving healthcare standards.6
Person-centered design (PCD) is a holistic approach to solving problems and designing products, systems or processes that are useful and practical for users by meeting their real needs.7,8 In this model, users are actively integrated in the development process to better understand and systematically analyze their needs, expectations and experiences and jointly design innovative solutions that satisfy their needs.9,10 The resulting design not only enables the accomplishment of the desired tasks but also ensures a meaningful and pleasurable experience.5
In 2021, the PCD methodology was implemented within the framework of the ASfarMA project to define the ideal MDSAT. The process to define the ideal MDSAT involved three steps: (a) identifying and understanding the processes, experiences and needs of the stakeholders involved; (b) defining the needs of MDSAT patients and professionals and identifying the critical points that define the ideal MDSAT; (c) co-designing solutions that will ultimately shape up the ideal MDSAT. In the last step, 21 innovative solutions were identified: 14 quick wins (requiring little effort but with a substantial positive impact) and 7 transformative solutions (having a greater impact but requiring more resources and effort). One of the seven transformative solutions included an MDSAT patient onboarding plan.6
“Onboarding” is generally used to refer to the process of integrating a new employee into an organization. The purpose of onboarding is to enable the professional to become competent and independent in performing their role, while also ensuring they understand the values of the organization. This concept has been transferred to the healthcare domain.11 Retaining a comparable meaning, the term “onboarding” is used in this study to refer to the set of actions, material and structured information delivered during the first contacts of the patient with the MDSAT. This part of the healthcare process has been identified as essential both by patients and professionals, who associate it with a high emotional burden and deem it to determine the patient-MDSAT relationship. As a result, onboarding was established as a priority solution that required action.
This study expands the preceding phase of the project and leverages previous findings in order to design an MDSAT patient onboarding process based on the needs identified by MDSAT patients and professionals.
MethodsA qualitative study was performed in a tertiary hospital using the PCD methodology. The study involved two phases: (a) a problem-centered phase; and (b) a solution-centered phase. Each of these phases was further divided into two sequential stages: a divergent approach intended to capture a wide and in-depth perspective, followed by a convergent approach designed to distil the essential elements. The four stages include Discover, Define, Develop and Validate.5
The core group included at least a professional from each specialty included in the MDSAT (allergology, pharmacy, immunology, pulmonology, otorhinolaryngology, pediatrics and psychiatry), along with four patients who were representative of the archetypes identified in the ASfarMA project6 and a PCD-expert company. Each archetype is a representation of a group of matched individuals in terms of behavior, age, comorbidities and lifestyle, as well as in terms of preferences, concerns and perceptions in relation to asthma.9 An archetype is not a stereotype or represents a particular individual, but is based on real-world patterns. The four archetypes identified include6:
- •
An adolescent who wants to forget their illness and fit into his environment, which is unaware of their illness. They would like not to have a daily treatment and are concerned about the long-term effects of corticosteroid therapy. They downplay the significance of their symptoms or conceal them from others.
- •
A middle-aged patient with healthy life habits who demonstrates a high level of self-demand in both personal and professional aspects of life. They are emotional and their environment overprotects them because of their illness, sometimes limiting their activities. They long to control the situation and feel anxious about experiencing unexpected exacerbations.
- •
A middle-aged patient suffering from other asthma-related comorbidities that require frequent visits to different specialists. They regularly seek information about their illness and symptoms on the Internet. They would like to have easy access to healthcare professionals and feel that they are empathetic and understanding of their symptoms.
- •
An advanced-age patient who has long lived with the illness and has other comorbidities affecting their quality of life. They feel like a burden to their relatives and therefore attempt to remain unnoticed. Their main sources of motivation include time with significant others, preservation of autonomy and feeling heard by healthcare professionals.
Following the PCD methodology, the stages of discovery and understanding, definition of needs, and co-creation (design) of solutions were conducted. The starting point was the information obtained in the previous stage of the ASfarMA project.6
The project involved three workshops followed by several sprint sessions.
- •
First workshop (November 2022): held face-to-face with patients, healthcare professionals and PCD experts. Patient experiences with their illness before and after referral to the MDSAT were collected, placing the focus on their first contacts with the multidisciplinary care team. A Patient Experience Map was designed (a tool that thoroughly collects patient process in relation to their illness and the emotions and perceptions they feel throughout the journey). This map contributed to identifying the positive aspects and unmet needs of patients. Finally, potential solutions were developed to design the patient onboarding process.
- •
The second workshop (December 2022) was held online with the healthcare professionals in the core group and the PCD group. These professionals identified the solutions previously developed in the ASfarMA project that were applicable to patient onboarding. Then, they identified ‘hotspots’ in the patient onboarding journey.
- •
The third workshop (January 2022) was held online with the healthcare professionals in the core group and the PCD group. The hotspots patient onboarding process was further defined, specifying the professionals responsible for each point and the resources (artifacts) required to inform and engage (activate) patients.
- •
Sprint sessions (February 2023): held online in small groups of healthcare professionals and members of the PCD group. The final content of the material was thoroughly developed.
The local Ethics Committee for research with medicines exempted us from the obligation to receive authorization for the study, as it was aimed at improving healthcare standards, thereby not raising any ethical considerations. Informed consent was obtained from all participants prior to inclusion.
ResultsWhen reporting their experience, patients expressed unfamiliarity with and anxiety about their illness (“I didn't know that this could happen to sportive people”) and its implications. Patients reported to feel vulnerable when communicating with healthcare professionals in a hierarchical patient-doctor relationship (“They've the power and you feel small” or “they're talking about me but not having a conversation”). In this context, patients adopt a skeptical stance regarding the recommendations and treatments provided by healthcare professionals. Later on their patient journey, these attitudes were reversed when conversations became bidirectional (“you start to listen because they listen to you”).
In relation to MDSAT onboarding, the needs expressed by patients included understanding their illness to gain autonomy in the management of their care; receiving personalized and coordinated care; maintaining bidirectional communication with physicians regarding their illness and treatment; having easy access to their physician in case of emergency; gaining control of their illness (“I want a life without limitations”); and reducing the use of oral corticosteroids.
In turn, healthcare professionals emphasized the need to delivery pre-defined, unified and structured information to patients, as well as hold open empathetic conversations with patients (“What concerns doctors often differs from what concerns patients, so, if questions during the consultation are too directed, these issues may not be identified”); and deliver appropriate information that helps patients lead a normal life (i.e. empowering patients, “that having a normal life is in the hands of the patients themselves”).
Based on these findings, along with those from the ASfarMA project, it was determined that the patient onboarding process should address the following needs: (a) establishing a controlled onboarding process (key professionals, points of contact, information to be delivered and the tools required [artifacts]); (b) designing an MDSAT onboarding entry point that is identifiable for patients, who should understand and appreciate what this multidisciplinary team offers; (c) defining the information to be delivered as well as how, when and who will deliver such information; (d) promoting more intense contact that strengthens the patient-doctor relationship and facilitates patient learning and engagement with MDSAT's processes, timelines, activities, and pathways).
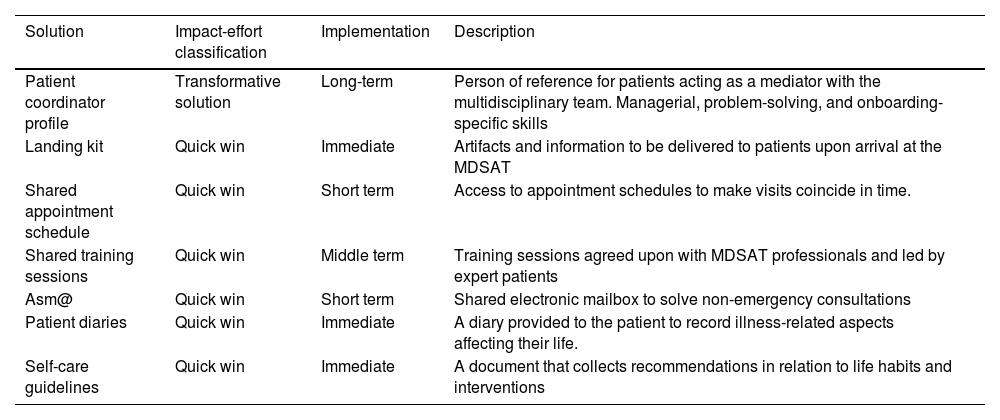
A total of seven ASfarMA solutions previously identified as useful for patient onboarding were selected. Table 1 summarizes their title, impact-effort classification (transformative solution vs quick win), implementation planning (immediate vs short-term vs long-term) and a brief description of the solutions identified.
Solutions previously identified in ASfarMA that are useful for patient onboarding.
| Solution | Impact-effort classification | Implementation | Description |
|---|---|---|---|
| Patient coordinator profile | Transformative solution | Long-term | Person of reference for patients acting as a mediator with the multidisciplinary team. Managerial, problem-solving, and onboarding-specific skills |
| Landing kit | Quick win | Immediate | Artifacts and information to be delivered to patients upon arrival at the MDSAT |
| Shared appointment schedule | Quick win | Short term | Access to appointment schedules to make visits coincide in time. |
| Shared training sessions | Quick win | Middle term | Training sessions agreed upon with MDSAT professionals and led by expert patients |
| Asm@ | Quick win | Short term | Shared electronic mailbox to solve non-emergency consultations |
| Patient diaries | Quick win | Immediate | A diary provided to the patient to record illness-related aspects affecting their life. |
| Self-care guidelines | Quick win | Immediate | A document that collects recommendations in relation to life habits and interventions |
MDSAT: Multidisciplinary severe asthma care team. The solutions identified were classified according to an impact-effort matrix (requiring little effort but with a considerable positive impact) and transformative solutions (having a greater impact but requiring more resources and efforts).
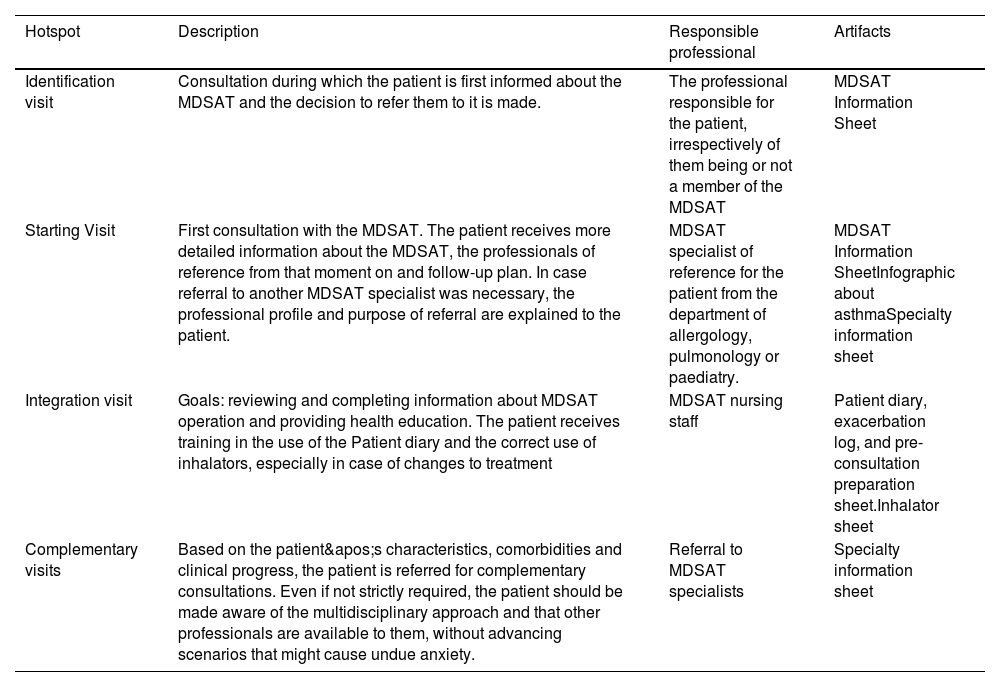
Table 2 depicts the onboarding ‘hotspots’ detected, the professionals involved, and the information and material required. The term “severe” was found to cause anxiety in patients. This term can be used to educate patients about asthma, adapting explanations to their prior knowledge to contextualize it and reduce anxiety.
Hotspots in MDSAT onboarding.
| Hotspot | Description | Responsible professional | Artifacts |
|---|---|---|---|
| Identification visit | Consultation during which the patient is first informed about the MDSAT and the decision to refer them to it is made. | The professional responsible for the patient, irrespectively of them being or not a member of the MDSAT | MDSAT Information Sheet |
| Starting Visit | First consultation with the MDSAT. The patient receives more detailed information about the MDSAT, the professionals of reference from that moment on and follow-up plan. In case referral to another MDSAT specialist was necessary, the professional profile and purpose of referral are explained to the patient. | MDSAT specialist of reference for the patient from the department of allergology, pulmonology or paediatry. | MDSAT Information SheetInfographic about asthmaSpecialty information sheet |
| Integration visit | Goals: reviewing and completing information about MDSAT operation and providing health education. The patient receives training in the use of the Patient diary and the correct use of inhalators, especially in case of changes to treatment | MDSAT nursing staff | Patient diary, exacerbation log, and pre-consultation preparation sheet.Inhalator sheet |
| Complementary visits | Based on the patient's characteristics, comorbidities and clinical progress, the patient is referred for complementary consultations. Even if not strictly required, the patient should be made aware of the multidisciplinary approach and that other professionals are available to them, without advancing scenarios that might cause undue anxiety. | Referral to MDSAT specialists | Specialty information sheet |
MDSAT: Multidisciplinary severe asthma care team.
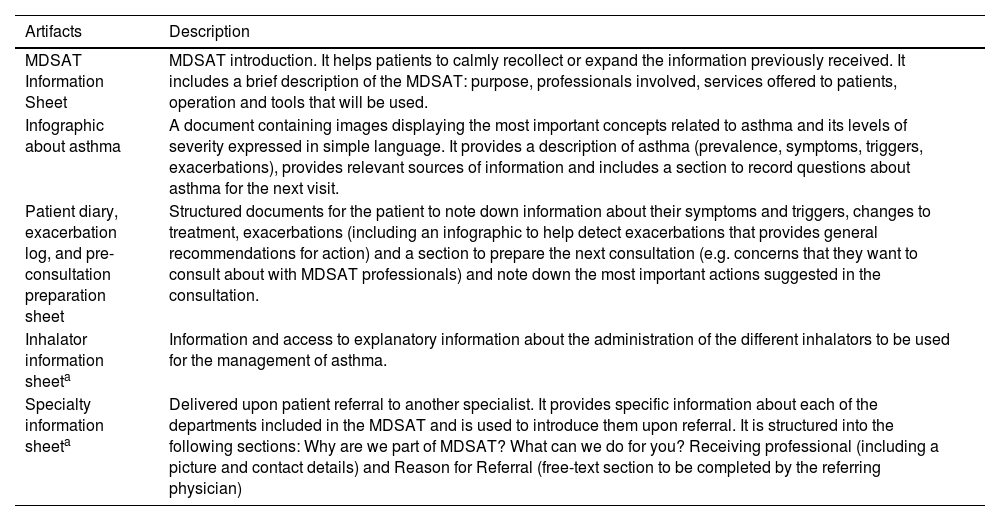
The final design, structure and artifact contents were defined (Table 3). Artifacts: patient diary, exacerbation log book, and pre-consultation preparation sheet, inhalator information sheet and a pulmonology department information sheet are available for consultation in the Supplementary Material.
Onboarding support artifacts in the multidisciplinary severe asthma care team.
| Artifacts | Description |
|---|---|
| MDSAT Information Sheet | MDSAT introduction. It helps patients to calmly recollect or expand the information previously received. It includes a brief description of the MDSAT: purpose, professionals involved, services offered to patients, operation and tools that will be used. |
| Infographic about asthma | A document containing images displaying the most important concepts related to asthma and its levels of severity expressed in simple language. It provides a description of asthma (prevalence, symptoms, triggers, exacerbations), provides relevant sources of information and includes a section to record questions about asthma for the next visit. |
| Patient diary, exacerbation log, and pre-consultation preparation sheet | Structured documents for the patient to note down information about their symptoms and triggers, changes to treatment, exacerbations (including an infographic to help detect exacerbations that provides general recommendations for action) and a section to prepare the next consultation (e.g. concerns that they want to consult about with MDSAT professionals) and note down the most important actions suggested in the consultation. |
| Inhalator information sheeta | Information and access to explanatory information about the administration of the different inhalators to be used for the management of asthma. |
| Specialty information sheeta | Delivered upon patient referral to another specialist. It provides specific information about each of the departments included in the MDSAT and is used to introduce them upon referral. It is structured into the following sections: Why are we part of MDSAT? What can we do for you? Receiving professional (including a picture and contact details) and Reason for Referral (free-text section to be completed by the referring physician) |
MDSAT: Multidisciplinary severe asthma care team.
The PCD model enabled the engagement of all stakeholders in the onboarding process to better understand their views, experiences and needs and co-design comprehensive, innovative solutions. Healthcare has been traditionally linked to the two first components of the so-called “good design”, namely, performance (i.e. functionality, how well it does the task or is fit for purpose, implementation of evidence-based medicine) and engineering or organization (security and reproducibility standards safeguarding patient safety); but less to usability (esthetics of experience, the way the whole interaction with the process or product is experienced or felt).12 Incorporating experience (third component of the “good design”) does not involve replacing the other two components but rather expands them. The aim is to identify challenges and opportunities for a more effective and safer process, reduce variability, and engage patients. The needs expressed by patients included receiving education on asthma, attaining greater autonomy in self-management, and enhancing their relationship and communication with healthcare professionals. Hence, addressing these needs –the pivotal factors of patient onboarding– will contribute to improving clinical outcomes.13–16
Understanding process flow and experiences is crucial to be able to provide information at the right time and in the right place that is useful and adapted to the patient's characteristics. This will help strengthen patient-healthcare professional cooperation in the long term.17 The importance of onboarding is also highlighted by Bellei et al.,18 who selected a set of requirements about patient onboarding and welcoming that health centers of excellence should meet in the management of hidradenitis suppurativa. Requirements included implementing a standardized process; providing relevant information about the illness and guidance on how to proceed in emergency situations, and establishing a detailed referral flow and patient care. To the best of our knowledge, this is the first study to establish and design a battery of solutions for MDSAT patient onboarding.
Previous studies also identify similar needs and solutions which, although they do not explicitly refer to the moment at which they should be addressed, it would seem appropriate to plan them from the onboarding. Van Harlingen et al.19 designed a toolkit to facilitate communication and expression of preferences for patients with chronic obstructive pulmonary illness or chronic heart failure when consulting with their healthcare providers. The toolkit includes a symptom log book, along with pre-designed forms to note down questions or topics to be addressed during the consultation. Additionally, the authors underlined the importance of access to disease-related documents or informative websites. Philpot et al.20 identified several factors with a high potential to influence patient experience. These factors include providing information to patients regarding their disease, self-management, and medication, and informing on the disease stage. Some of the solutions suggested include providing pre-consultation questionnaires to identify changes in the disease; providing access to downloadable patient education material; planning key questions that should be addressed during the consultation; providing follow-up education and instructions adapted to the patient; and designing a patient-centered referral pathway. Sonney et al.21 designed an asthma essentials kit to support parent–child shared asthma management. Patients reported requiring an action plan, educational materials on asthma and inhalers, and artifacts to track triggers and symptoms, findings that are consistent with our study.
The limitations of this study lie in the fact that the experiences of patients and professionals were collected in a single center within a specific period. Therefore, as our recommendations are aimed at satisfying user needs in a specific time–space framework, other priorities may exist in other environments, considering the rapidly evolving landscape of scientific-technological research and its social impact.
Nevertheless, a rigorous qualitative research methodology was used for stakeholders to report their needs and co-design tailored solutions. We firmly believe that our findings may be useful for other MDSATs and multidisciplinary teams attending complex chronic patients, irrespectively of any potential differences with other centers or any changes in patient needs as new technological solutions emerge. Indeed, the needs and solutions suggested in this project are comparable to those identified in previous studies in different environments and periods. The solutions developed can be implemented directly or adapted to the particularities of each center. The methodology described can be a road map for other projects aimed at enhancing healthcare standards. Additionally, both the needs and solutions developed go beyond the use of technologies and should be positively approached. Hence, technological advancements will not render our solutions obsolete but will contribute to refining, enhancing or adapting them to different formats. It is also important to highlight that the involvement of all departments in the MDSAT has strengthened its multidisciplinary character and internal cohesion, while enabling the identification of strengths and weaknesses. Patient involvement in the project, including the co-design of solutions, provided valuable insights that guided the design of the patient onboarding process and the development of the supporting artifacts.
This work allowed us to design, structure, and standardize patient onboarding, providing an environment that facilitates self-management and open, empathetic, bidirectional communication between patients and healthcare professionals, in line with the essential needs expressed by both groups. These findings may be useful for other multidisciplinary care teams. The next step will be to assess the impact of the implemented solutions on healthcare quality and patient knowledge of the illness.
Contribution to the scientific literatureThe results reported provide information about the needs of patients and healthcare providers in a multidisciplinary severe asthma care team regarding onboarding. In addition, we suggest a battery of solutions and co-designed tools developed using the person-centered design methodology.
These solutions and tools may help other multidisciplinary severe asthma care teams or other projects aimed at enhancing the quality of care in chronic illness.
CRediT authorship contribution statementHilario Martínez-Barros: Writing – review & editing, Writing – original draft, Project administration, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. María Muñoz-García: Writing – review & editing, Supervision, Project administration, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Darío Antolín-Amérigo: Writing – review & editing, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Silvia Sánchez-Cuéllar: Writing – review & editing, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Ana Morales-Tirado: Writing – review & editing, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Ana de-Andrés-Martín: Writing – review & editing, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Gonzalo de-los-Santos-Granados: Writing – review & editing, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Laura Yeguas-Ramírez: Writing – review & editing, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Enrique Blitz-Castro: Writing – review & editing, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Alfonso Santamaría-Gadea: Writing – review & editing, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Belén de-la-Hoz-Caballer: Writing – review & editing, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Sagrario Martín-Aragón: Writing – review & editing, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. David González-de-Olano: Writing – review & editing, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Ana María Álvarez-Díaz: Writing – review & editing, Methodology, Investigation, Funding acquisition, Formal analysis, Data curation, Conceptualization.
Ethical considerationsThe local Ethics Committee for research with medicines exempted us from the obligation to receive authorization to carry out the study, as it was a study aimed at improving healthcare standards not raising any ethical considerations. Informed consent was obtained from all participants prior to inclusion.
AuthorshipAll authors contributed to the conception and design of the study. Hilario Martínez-Barros drafted the first version of the manuscript under the supervision of María Muñoz-García, which was critically reviewed by the other authors, who contributed to the final manuscript. The three authors approved the final version of the manuscript submitted for publication.
FundingThe authors declare that this work was funded by AstraZeneca and Sanofi.
ASfarMA was supported by AstraZeneca and Sanofi. Hilario Martínez-Barros received support from AMGEN for travel expenses and attendance at the Midyear Clinical Meeting 2023 of the American Society of Health-System Pharmacists, held in December 2023. María Muñoz-García has received honoraria for lectures from AstraZeneca and GSK and for advisory activities from Astrazeneca, GSK and Sanofi. Darío Antolín-Amérigo has received honoraria for lectures from for lectures from AstraZeneca, Chiesi, Gebro, GSK, Leti Pharma, Menarini, Roxall and Sanofi and honoraria for advisory activities from ALK-Abelló, AstraZeneca, Chiesi and Gebro. Silvia Sánchez-Cuéllar has received honoraria for lectures from AstraZeneca, Bial, Chiesi, Faes, Gebro Pharma, GSK, Novartis and Sanofi and honoraria for advisory activities from AstraZeneca, Chiesi, GSK, Novartis and Sanofi, as well as support from AstraZeneca, Bial, Chiesi, Faes, Gebro Pharma, GSK, Novartis and Sanofi for travel and attendance at scientific meetings. Ana Morales-Tirado has received support from Sanofi for attending scientific meetings. Laura Yeguas-Ramírez has received honoraria for lectures from GSK. Enrique Blitz-Castro has received honoraria for lectures from GSK and support from Sanofi for attending scientific meetings. Alfonso Santamaría-Gadea has received honoraria for lectures from AstraZeneca, GSK and Sanofi and honoraria for advisory activities from AstraZeneca, GSK and Sanofi, and has received support from Sanofi for attending scientific meetings. Belén de-la-Hoz-Caballer has received honoraria for lectures from Inmunotek and honoraria for advisory activities from Leti Pharma and Sanofi.