The goals of this study were to analyze the type of antithrombotic treatment administered to institutionalized patients with nonvalvular atrial fibrillation (and any ensuing complications) and to evaluate the degree of anticoagulation control achieved with vitamin K antagonists.
MethodThis was a prospective observational follow-up study carried out in seven elderly care facilities during 2016. Patients with nonvalvular atrial fibrillation were evaluated for their antithrombotic therapy and any embolic or hemorrhagic events, as well as for mortality. Subjects on anticoagulation treatment with VKAs were evaluated for anticoagulation control, with control considered poor if the mean time in therapeutic range was < 65% when measured with Rosendaal's method or < 60% when determined by the direct method.
ResultsOf the 699 residents evaluated, 20.6% had a diagnosis of NVAF. Average age was 85.83 years. Both the cardioembolic (mean CHA2DS2-VASc score: 4.79), and the hemorrhagic (mean HAS-BLED score: 3.04) risk were high. Fifty percent received anticoagulation treatment, mainly with vitamin K antagonists, of whom at least 56% were not within the therapeutic range. Sixteen percent of the residents, the oldest and most functionally and cognitively dependent ones, had not been prescribed any antithrombotic therapy. A higher frequency of hospital admissions induced by cardiovascular and bleeding events was found in these residents, although differences were not statistically significant.
ConclusionsHalf of institutionalized geriatric patients with nonvalvular atrial fibrillation are anticoagulated, a third on antiplatelet therapy, and some without any antithrombotic treatment. This study showed that as functionality decreases, treatment strategies are increasingly aimed at therapeutic deintensification. Given that the degree of anticoagulation control with vitamin K antagonists is inadequate in 56% of cases, it is essential to monitor the time in therapeutic range to optimize treatment as needed.
Los objetivos de este trabajo son estudiar el tipo de tratamiento antitrombótico y sus complicaciones en pacientes institucionalizados con fibrilación auricular no valvular y evaluar el grado de control anticoagulante con medicamentos tipo antivitamina K.
MétodoEstudio observacional de seguimiento prospectivo realizado en siete centros gerontológicos durante el año 2016, valorando en aquellos residentes con fibrilación auricular no valvular la terapia antitrombótica establecida y las incidencias embólicas, hemorrágicas y la mortalidad. En los residentes anticoagulados con antivitamina K se midió el control de la anticoagulación, estimándose un mal control si el método de Rosendaal fuese < 65% o el tiempo en rango terapéutico directo < 60%.
ResultadosDe los 699 residentes analizados, el 20,6% tenían un diagnóstico de fibrilación auricular no valvular, con una edad media de 85,83 años. El riesgo cardioembólico fue alto (CHA2DS2-VASc medio 4,79), así como el riesgo hemorrágico (HAS-BLED medio 3,04). El 50% estaban anticoagulados, principalmente con antivitamina K, de los cuales al menos el 56% no se encontraban dentro del rango terapéutico. Un 16% de los residentes no tenían prescrita terapia antitrombótica, destacando en éstos una mayor dependencia funcional, cognitiva y edad más avanzada. Se encontró una mayor frecuencia de ingresos hospitalarios de causa cardiovascular y de sangrados en aquellos residentes anti-coagulados, aunque no hubo diferencias significativas.
ConclusionesLa mitad de los pacientes geriátricos institucionalizados con fibrilación auricular no valvular están anticoagulados, un tercio antiagregados y algunos sin tratamiento antitrombótico, observando que a medida que disminuye la funcionalidad las estrategias van en la línea de una desintensificación terapéutica. El grado de control anticoagulante con antivitamina K es inadecuado en el 56% de los casos, por lo que es imprescindible monitorizar el tiempo en rango terapéutico para optimizar el tratamiento cuando sea necesario.
Atrial fibrillation (AF) is the most frequent cardiac arrythmia in the geriatric population. It affects 6% of the general Spanish population1, and up to 17% of residents of long-term care facilities2,3.
AF increases cardiovascular morbidity and mortality and is the cause of 15% of ischemic cardiovascular events and 30% of overall cardiovascular events. Such events result in permanent disability in 60% of cases and in a mortality rate of 20%4.
The most frequent cause of AF is ischemic or hypertensive heart disease, with a distinction being made between valvular AF, occurring in subjects with moderate or severe mitral valve stenosis or in those with a mechanical valve prosthesis, and nonvalvular AF (NVAF), as each of those conditions requires different treatment strategies5.
Anticoagulation treatment is the most effective method to prevent stroke and systemic embolism in patients with NVAF. Use of vitamin K antagonists (VKAs) is associated with a narrow therapeutic window, a scarcely predictable response, and multiple interactions with other drugs or with foods. However, VKAs have the advantage that their effect can be easily reversed with an antidote and they are associated with a favorable cost/benefit ratio6. Direct oral anticoagulants (DOACs) produce a more predictable response without the need for close monitoring, they are less prone to interactions, and are recommended as first choice treatment by the American Heart Association (AHA) and the European Society of Cardiology (ESC)5,7. Given the high embolic and hemorrhagic risk profile and limited life expectancy faced by the institutionalized population, implementation of thromboembolic prevention therapy poses a significant clinical and ethical dilemma. Moreover, the absence of such patients from clinical trials limits the amount of scientific evidence available regarding the efficacy and safety of the different interventions.
For the foregoing reasons, several attempts have been made to determine the right therapeutic strategy for NVAF. A study performed in elderly care homes8 analyzed the factors associated with selecting between different anticoagulation strategies and found that a history of stroke tended to result in the use of DOACs, while the presence of chronic renal disease led to the prescription of VKAs. Another study in elderly care homes examined why institutionalized patients with AF did not receive anticoagulation therapy and found that the presence of repeated falls, a hemorrhagic history and advanced age came up as the most recurring reasons9.
The efficacy and tolerability of VKAs depends on the quality of anticoagulation control as reflected by the mean time in therapeutic range (TTR) of the international normalized ratio (2.0–3.0). A suboptimal TTR is associated with a higher risk of adverse events and a significant increase in mortality10.
Thromboembolic risk can be estimated using the CHA2DS2-VASc scale, the high-risk threshold standing at ≥ 2 for males and at ≥ 3 for females11. Hemorrhagic risk is measured with the HAS-BLED scale, a score ≥ 3 being regarded as high risk12. A systematic review observed that, except for intracranial hemorrhage, the bleeding risk of antiplatelet therapy (aspirin or clopidogrel) and of oral anticoagulation is similar, with similar mortality rates13.
The main goal of this study was to examine different kinds of antithrombotic treatment and the complications they cause in institutionalized patients with NVAF. Secondary goals included the extent to which VKAs are able to control anticoagulation.
MethodsThis is a multicenter prospective observational long-term follow-up study performed in seven elderly care facilities in the province of Guipuzcoa, Spain. The study included all the patients diagnosed with permanent NVAF at least six months prior to enrolment.
The clinical and demographic data were obtained from the patients’ electronic medical records (EMRs) on 1 October 2015. To determine the degree of anticoagulation control with AVKs, the TTR was calculated at two points of time (1 October 2015 and 1 April 2016). The mean of both results and the degree of control were duly recorded. Patients on antithrombotic treatment were subjected to a follow-up period that ran from 1 October 2015 to 1 October 2016, in the course of which all potential adverse events were evaluated.
Variables analyzed included age, sex, the Charlson comorbidity index, functional ability as measured by the Barthel index, cognitive status as determined by the Mini Mental State Exam (MMSE) and Reisberg's GDS-FAST staging system, body mass index (BMI), the number of falls, and the number of drugs prescribed, excluding medications prescribed on demand. Creatinine clearance was estimated using Cockroft & Gault's formula14. Cardioembolic risk was calculated using the CHA2DS2-VASc scale11 and hemorrhagic risk was determined by means of the HAS-BLED scale12. Variables studied during the follow-up period included the presence of embolic [stroke, deep venous thrombosis (TVP), pulmonary thromboembolism (PTE)] and hemorrhagic events of any degree of severity, as well as hospital admissions due to cardiovascular events (ischemic heart disease, heart failure) and mortality. The information was obtained from the patients’ EMR.
For residents on VKA treatment, the degree of anticoagulation control was determined by calculating TTR with both the Rosendaal method (RM)15, which estimates the percentage of time the patient is within the therapeutic range, assuming a linear progression of change between consecutive INR values; and with the direct method (DM), which counts the number of tests within range and divides them by the total number of tests. The INR range for effective coagulation has been established at 2–3, with RM- or direct method-based TTR values of < 65% and < 60% respectively being considered indicative of poor anticoagulation control.
A descriptive analysis was carried out of central tendency measures (mean and median) and dispersion (standard deviation, and interquartile range) for quantitative variables, and of absolute and relative frequencies for qualitative variables. Non-parametric statistical analyses were used to compare qualitative (chi squared) and quantitative variables (Mann-Whitney U test and Kruskall-Wallis test). The analyses were carried out using the IBM SPSS Statistics 19.0 software package, with p values < 0.05 being considered statistically significant.
The data was extracted from the patients’ EMR with an exclusively investigative purpose and in compliance with all prevailing ethical norms. All the data were duly anonymized. The paper was evaluated and approved by the relevant research ethics committee (Identification number: PFI-ACO.2015–01).
ResultsThe total population of the nine elderly care centers studied comprised 699 residents, with a mean age of 83.5 years. Eighty percent of them were women, 46% were severely dependent (Barthel score < 40), and 69% exhibited cognitive impairment (MMSE < 20 points). The mean number of medications was 7.31.
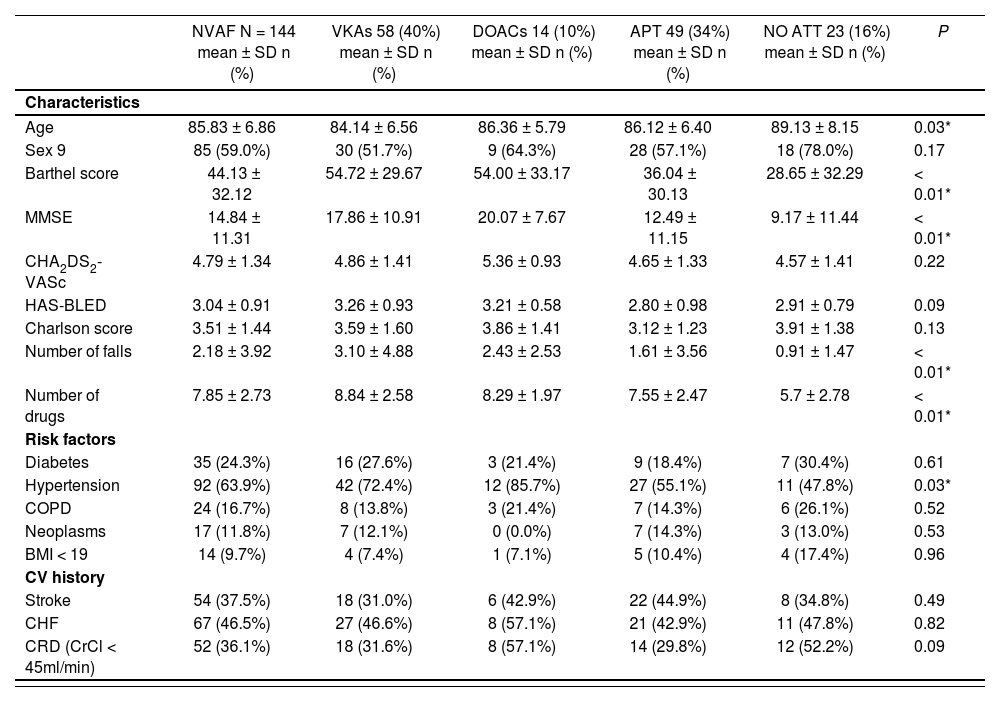
Prevalence of NVAF was 20.6% (n = 144), with a mean age of 84.81 years (82.84 ± 6.10 years in males and 86.42 ± 6.88 years in females); 41% of NVAF patients were male. Fifty percent of these patients were on antiplatelet treatment, mainly VKA. Table 1 shows the residents’ demographic and clinical characteristics with the different treatment strategies employed. As regards the anticoagulation treatments prescribed, 100% of VKAs were acenocumarol; DOACs comprised rivaroxaban (57%), apixaban (36%), and dabigatran (7%). Antiplatelet treatment consisted mostly in acetylsalicylic acid (88%), although clopidogrel (10%) and dual therapy with acetylsalicylic acid and clopidogrel (2%) were also identified. No resident was being treated with a combination of an anticoagulant and an antiplatelet agent. Sixteen percent of patients were not being treated with any antithrombotic medication.
Demographic and clinical characteristics of nonvalvular atrial fibrillation patients distributed across the different treatment strategies employed
| NVAF N = 144 mean ± SD n (%) | VKAs 58 (40%) mean ± SD n (%) | DOACs 14 (10%) mean ± SD n (%) | APT 49 (34%) mean ± SD n (%) | NO ATT 23 (16%) mean ± SD n (%) | P | |
|---|---|---|---|---|---|---|
| Characteristics | ||||||
| Age | 85.83 ± 6.86 | 84.14 ± 6.56 | 86.36 ± 5.79 | 86.12 ± 6.40 | 89.13 ± 8.15 | 0.03* |
| Sex 9 | 85 (59.0%) | 30 (51.7%) | 9 (64.3%) | 28 (57.1%) | 18 (78.0%) | 0.17 |
| Barthel score | 44.13 ± 32.12 | 54.72 ± 29.67 | 54.00 ± 33.17 | 36.04 ± 30.13 | 28.65 ± 32.29 | < 0.01* |
| MMSE | 14.84 ± 11.31 | 17.86 ± 10.91 | 20.07 ± 7.67 | 12.49 ± 11.15 | 9.17 ± 11.44 | < 0.01* |
| CHA2DS2-VASc | 4.79 ± 1.34 | 4.86 ± 1.41 | 5.36 ± 0.93 | 4.65 ± 1.33 | 4.57 ± 1.41 | 0.22 |
| HAS-BLED | 3.04 ± 0.91 | 3.26 ± 0.93 | 3.21 ± 0.58 | 2.80 ± 0.98 | 2.91 ± 0.79 | 0.09 |
| Charlson score | 3.51 ± 1.44 | 3.59 ± 1.60 | 3.86 ± 1.41 | 3.12 ± 1.23 | 3.91 ± 1.38 | 0.13 |
| Number of falls | 2.18 ± 3.92 | 3.10 ± 4.88 | 2.43 ± 2.53 | 1.61 ± 3.56 | 0.91 ± 1.47 | < 0.01* |
| Number of drugs | 7.85 ± 2.73 | 8.84 ± 2.58 | 8.29 ± 1.97 | 7.55 ± 2.47 | 5.7 ± 2.78 | < 0.01* |
| Risk factors | ||||||
| Diabetes | 35 (24.3%) | 16 (27.6%) | 3 (21.4%) | 9 (18.4%) | 7 (30.4%) | 0.61 |
| Hypertension | 92 (63.9%) | 42 (72.4%) | 12 (85.7%) | 27 (55.1%) | 11 (47.8%) | 0.03* |
| COPD | 24 (16.7%) | 8 (13.8%) | 3 (21.4%) | 7 (14.3%) | 6 (26.1%) | 0.52 |
| Neoplasms | 17 (11.8%) | 7 (12.1%) | 0 (0.0%) | 7 (14.3%) | 3 (13.0%) | 0.53 |
| BMI < 19 | 14 (9.7%) | 4 (7.4%) | 1 (7.1%) | 5 (10.4%) | 4 (17.4%) | 0.96 |
| CV history | ||||||
| Stroke | 54 (37.5%) | 18 (31.0%) | 6 (42.9%) | 22 (44.9%) | 8 (34.8%) | 0.49 |
| CHF | 67 (46.5%) | 27 (46.6%) | 8 (57.1%) | 21 (42.9%) | 11 (47.8%) | 0.82 |
| CRD (CrCl < 45ml/min) | 52 (36.1%) | 18 (31.6%) | 8 (57.1%) | 14 (29.8%) | 12 (52.2%) | 0.09 |
APT: antiplatelet therapy; ATT: antithrombotic therapy; BMI: body mass index; CHA2DS2-VASc: stroke risk assessment scale; CHF: congestive heart failure; COPD: chronic obstructive pulmonary disease; CrCl: creatinine clearance; CRD: chronic renal disease; DOACs: direct oral anticoagulants; HAS-BLED: scale used to estimate the anticoagulation treatment-induced bleeding risk; MMSE: Mini Mental State Exam; NVAF: nonvalvular atrial fibrillation; SD: standard deviation; VKAs: vitamin K antagonists.
The mean score on the CHA2DS2-VASc scale was 4.86 ± 1.25 (males 4.71 ± 1.40; females 4.85 ± 1.31). On the HAS-BLED scale, the mean score was 3.04 ± 0.92 (males 3.12 ± 1.01; females 2.99 ± 0.83). This is indicative of a right cardioembolic and hemorrhagic risk among the studied population.
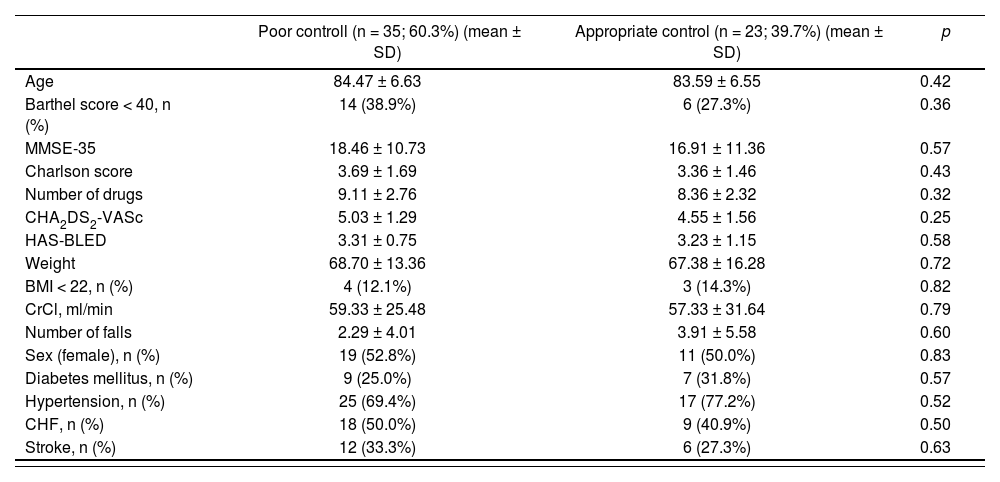
The degree of coagulation control through the one-year follow-up period was inadequate in 56.2% of residents according to the RM and in 60.3% according to the DM. Table 2 contains the subjects’ clinical characteristics as a function of the level of anticoagulation control measured by the DM. No statistically significant differences were observed. During follow-up, a higher incidence of mortality was observed in poorly controlled patients on VKA (371%) than in those who exhibited adequate anticoagulation control (17.4%). This difference was however not significant (OR = 2.89, CI95% 0.78–10.07; p = 0.106).
Factors associated to the degree of anticoagulation therapy control with vitamin K antagonists as calculated using the direct method
| Poor controll (n = 35; 60.3%) (mean ± SD) | Appropriate control (n = 23; 39.7%) (mean ± SD) | p | |
|---|---|---|---|
| Age | 84.47 ± 6.63 | 83.59 ± 6.55 | 0.42 |
| Barthel score < 40, n (%) | 14 (38.9%) | 6 (27.3%) | 0.36 |
| MMSE-35 | 18.46 ± 10.73 | 16.91 ± 11.36 | 0.57 |
| Charlson score | 3.69 ± 1.69 | 3.36 ± 1.46 | 0.43 |
| Number of drugs | 9.11 ± 2.76 | 8.36 ± 2.32 | 0.32 |
| CHA2DS2-VASc | 5.03 ± 1.29 | 4.55 ± 1.56 | 0.25 |
| HAS-BLED | 3.31 ± 0.75 | 3.23 ± 1.15 | 0.58 |
| Weight | 68.70 ± 13.36 | 67.38 ± 16.28 | 0.72 |
| BMI < 22, n (%) | 4 (12.1%) | 3 (14.3%) | 0.82 |
| CrCl, ml/min | 59.33 ± 25.48 | 57.33 ± 31.64 | 0.79 |
| Number of falls | 2.29 ± 4.01 | 3.91 ± 5.58 | 0.60 |
| Sex (female), n (%) | 19 (52.8%) | 11 (50.0%) | 0.83 |
| Diabetes mellitus, n (%) | 9 (25.0%) | 7 (31.8%) | 0.57 |
| Hypertension, n (%) | 25 (69.4%) | 17 (77.2%) | 0.52 |
| CHF, n (%) | 18 (50.0%) | 9 (40.9%) | 0.50 |
| Stroke, n (%) | 12 (33.3%) | 6 (27.3%) | 0.63 |
Poor control (direct method): < 60%; appropriate control (direct method): ≥ 60%.
BMI: body mass index; CHA2DS2-VASc: stroke risk estimation scale; CHF: congestive heart failure; CrCl: creatinine clearance; HAS-BLED: scale used to estimate the anticoagulation treatment-induced bleeding risk; SD: standard deviation.
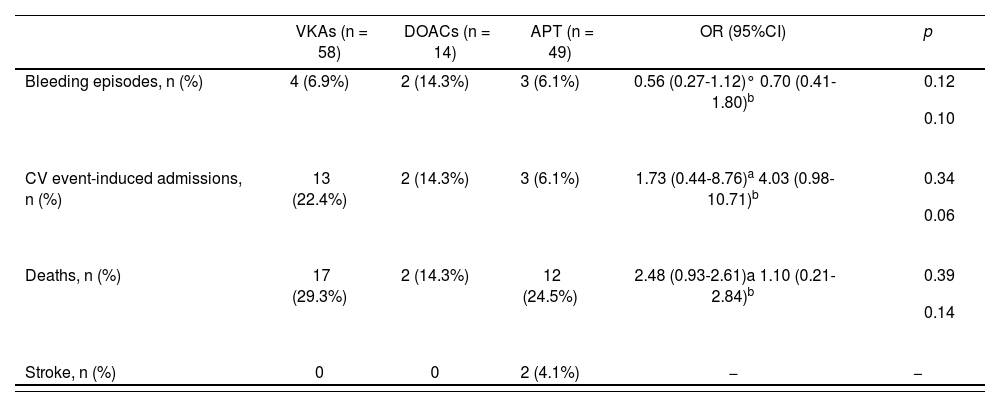
Table 3 shows the adverse events recorded over the one-year follow-up period with the different antithrombotic strategies. An increased incidence of bleeding and admissions due to cardiovascular events were observed in subjects on anticoagulation treatment, without differences reaching statistical significance. Only two cerebrovascular events were reported during the follow-up period, which corresponded to patients on antiplatelet treatment. No cases of DVT or PTE were recorded.
Adverse events associated with antithrombotic therapy
| VKAs (n = 58) | DOACs (n = 14) | APT (n = 49) | OR (95%CI) | p | |
|---|---|---|---|---|---|
| Bleeding episodes, n (%) | 4 (6.9%) | 2 (14.3%) | 3 (6.1%) | 0.56 (0.27-1.12)° 0.70 (0.41-1.80)b |
|
| CV event-induced admissions, n (%) | 13 (22.4%) | 2 (14.3%) | 3 (6.1%) | 1.73 (0.44-8.76)a 4.03 (0.98-10.71)b |
|
| Deaths, n (%) | 17 (29.3%) | 2 (14.3%) | 12 (24.5%) | 2.48 (0.93-2.61)a 1.10 (0.21-2.84)b |
|
| Stroke, n (%) | 0 | 0 | 2 (4.1%) | − | − |
APT: antiplatelet therapy; CV: cardiovascular; DOACs: direct oral anticoagulants; OR: odds No statistically significant differences were observed. During follow-up, a higher incidence of mortality was observed in poorly controlled patients on VKA (37.1%) than in those who exhibited adequate anticoagulation control (17.4%). This difference was however not significant (OR = 2.89, CI95% 0.78-10.07; p = 0.106).
ratio; VKAs: vitamin K antagonists.
Prevalence of NVAF among the institutionalized population considered in our study was 20.6%, which is higher than the rate found in long-term care facilities or in the community. This figure rose considerably in the case of residents over 85 years of age2. In contrast, a study performed in elderly care facilities9 obtained a prevalence of AF of 10.1%. The difference was possibly due to the fact that in this study all residents were subjected to an ECG.
An evaluation of the influence of demographic and clinical variables on the treatment strategy adopted showed significant differences for age, Barthel score, MMSE, number of falls, number of drugs administered, and hypertension. It would seem that, as patients grown older and their functional and cognitive status deteriorates, treatment strategies tend to favor anticoagulation, with fewer drugs being administered. In the previously mentioned study conducted in elderly care centers9, less than 50% of patients received anticoagulation treatment despite their high stroke risk. This is in line with the findings of this study. An appropriate assessment of the need of anticoagulation therapy in very elderly institutionalized patients should consider, apart from the CHA2DS2-VASc and HAS-BLED scores, information related to the patients’ overall geriatric status, which usually serves as a basis to establish each resident's clinical goals. Anticoagulation in NVAF patients with short life expectancy is controversial, as mentioned in the STOPP-Frail criteria16. Petidier et al. provide a normo-gram that facilitates decision making regarding anticoagulation treatment taking into consideration life expectancy as determined by the NECPAL scale together with the frailty index. The instrument quantifies nutritional, cognitive, and emotional aspects, as well as different geriatric syndromes such as falls, dysphagia and polymedication17. After carefully analyzing such factors, it is essential to involve the resident (or their principal care-giver if they are unable to make decisions by themselves) in all decisions regarding their therapeutic management so that all risks and clinical goals are appropriately shared18.
Furthermore, it should be said that 34% of subjects were on antiplatelet medication despite the ESC clinical guidelines’ recommendation not to use these drugs for preventing thromboembolic events5. In the same vein, according to the latest STOPP-Frail criteria use of acetylsalicylic acid to prevent stroke in patients with AF who are not amenable to anticoagulation therapy is barely effective and increases the risk of hemorrhage16,19.
As regards anticoagulation treatment with VKAs patients in this study exhibited a high prevalence of poor anticoagulation control. Indeed, 56% of patients were outside the therapeutic range (as measured by the RM) for the length of the study; the figure rose to 60.3% when the direct method was used. Pivotal studies comparing the different DOACs with VKAs achieved a TTR of 65% (interquartile range: 51–76%), which shows the variability of results and the difficulties inherent in maintaining anticoagulation therapy even in controlled scenarios20. A community study carried out in the Galicia region showed that, over the course of one year, more than 40% of NVAF patients anticoagulated with VKAs were poorly controlled21. The high incidence of poor control in this study could be due to drug-drug interactions, drug-food interactions, or to the clinical complexities exhibited by these frequently polymedicated patients in an environment characterized by high levels of compliance given the strict supervision by the nursing staff.
The group of patients on poorly controlled VKA treatment exhibited higher mortality rates, yet with no statistically significant differences. A large-scale population-based study found that the mortality risk among properly controlled patients was 81% lower than among poorly controlled ones22. This demonstrates the importance of monitoring the degree of anticoagulation control in patients on VKAs. Should poor anticoagulation control be detected, a review of the patients’ pharmacological treatment is in order to rule out drug-drug and/or drug-food interactions and, if required, test the feasibility of DOAC treatment in those patients.
Some of the studied residents exhibited wide INR fluctuations which, if associated with laukoaraiosis-induced brain injury (as detected on neuroimaging) or high blood pressure, may result –together with advanced age– in a high risk of intracranial hemorrhage23. At the same time, it is advisable to carry out regular blood tests to screen for potential anemia and to control renal function, particularly in the context of a loss of brain volume (fever, vomiting, diarrhea, and acute decompensated heart failure), to ensure that these severely dependent patients are treated as safely as possible.
Patients in this study exhibited a high cardioembolic risk as calculated using the CHA2DS2-VASc scale (4.79 ± 1.34), equivalent to an annual stroke rate between 9.27 and 19.74 every 100 patients/year (calculated for a CHA2DS2-VASc score between 3 and 6 points, respectively)11. Moreover, the HAS-BLED score was 3.04 ± 0.91, indicating a high bleeding risk of between 1.88 and 8.70 episodes every 100 patients/year12 (calculated for a HAS-BLED score between 2 and 4 points respectively). This means that the cardioembolic risk was higher than the hemorrhagic risk.
As regards the incidence of hemorrhage, very few cases were recorded over the follow-up period, which complicates the interpretation of the differences found in patients receiving different kinds of treatment. Antithrombotic strategies did not exhibit differences in terms of the number of hospital admissions resulting from cardiovascular events. There did seem to be a tendency toward a higher number of admissions among patients on antiplatelet treatment. This could be attributed to the fact that patients on such treatments are often more frail and have a more limited life expectancy which, on many occasions, results in them not being transferred to a hospital. As far as deaths are concerned, no differences were observed between the treatment groups. A study conducted in an internal medicine department, which analyzed a similarly-sized sample of comparable age over a similar follow-up time, showed that subjects with NVAF who did not receive anticoagulation treatment on admission had a higher bleeding risk, a poorer functional status, and a higher risk of becoming frail. The study found statistically significant differences regarding the number of deaths, which was higher in patients not receiving antiplatelet treatment, which was attributed to factors such as frailty and the presence of advanced chronic diseases24. Further research is required into the benefits of anticoagulation at the end of life to settle the existing controversies in this area.
Observational studies allow an analysis of different aspects of clinical practice without the limitations of clinical trials, which negatively impact the external validity of the results obtained. This may be highly useful to understand the clinical experience of patient populations such as that of institutionalized elderly patients, who are often excluded from clinical trials.
This study is not without limitations. The sample size was not large enough to obtain statistically significant differences for some of the variables studied. Moreover, the analyzed populations were not homogeneous as the sample included patients with different therapeutic targets. Future studies could analyze the subjects’ frailty status as a confounding factor. The follow-up time was too short to appropriately evaluate effectiveness and safety in terms of the incidence of bleeding episodes, hospital admissions included by cardiovascular events, and mortality. The number of INR tests performed was not counted, with the TTR being calculated over a period of 6 months to minimize potential variations regarding the number of INR tests ordered by every clinician. Furthermore, information could have been lost in cases of referrals to the emergency room or hospital admissions as access to EMRs was restricted at the time of the study, with a low incidence of DVT and PTE being detected in both scenarios.
Despite the above, this study had provided a better understanding of the complexity of antithrombotic treatment of NVAF and of the difficulties inherent in maintaining antithrombotic control with VKAs in such a scarcely studied population as that of the institutionalized elderly. It has also helped understand the risks posed by the different antithrombotic therapies in a highly vulnerable population.
It is essential to gain a better understanding of the effectiveness and safety of anticoagulation therapy in the institutionalized population using larger sample sizes. Comparative studies are also needed between different anticoagulants to better individualize therapy.
In a nutshell, this study has shown a high prevalence of NVAF in the institutionalized population, with a high embolic and hemorrhagic risk. A high percentage of the subjects studied were not on any anticoagulation treatment. In some cases, they were inappropriately receiving antiplatelet agents and in others they were on antithrombotic treatment. We found that as effectiveness diminishes, treatment strategies are increasingly aimed at deintensification. Nevertheless, no data has been published demonstrating any benefit to maintaining anticoagulation at the end of life. Also, the degree of anticoagulation control with VKAs has been shown not to be appropriate on many occasions, which makes it essential to monitor the TTR to optimize treatment whenever necessary.
FundingNo funding.
AcknowledgementsThe authors would like to thank the subjects and their families for allowing them to analyze the data obtained, as well as the staff at the participating elderly care centers.
Conflict of interestNo conflict of interest.
Contribution to the scientific literature
The development of cognitive impairment in institutionalized individuals with nonvalvular atrial fibrillation has often resulted in deinteinten-sification of antithrombotic therapy.
An insight into the time in therapeutic range of vitamin K antagonists has allowed identification of a high percentage of poorly controlled patients, making it necessary to implement a series of follow-up strategies for the use of these drugs.