Sustainable management of healthcare waste has a positive impact on the global environment. In order to reduce it, the sustainable practice of the pharmacotherapeutic process in all its stages is essential.
ObjectiveTo analyze the sustainability strategies proposed by the pharmacy service to reduce drug waste derived from the pharmacotherapeutic process. Secondary objectives: to analyze the stage of the pharmacotherapeutic process and the number and type of drugs involved.
MethodsThe study was carried out in a tertiary level hospital. To coordinate the proposals, a referent pharmacist from every pharmacy department area was selected. Four stages of the process were evaluated (procurement, validation, dispensing and compounding), patients concerned were classified as outpatients or inpatients, and drugs potentially involved were analyzed by the administration route: into oral or parenteral.
Results28 ideas were proposed, which could affect more than 1200 drugs. 39.3% would affect the validation process, 17.9% the procurement management, 17.9% dispensing and 7.1% the compounding. Implementation feasibility and acceptability of these proposals were evaluated. Those with the greatest potential were: limiting the duration of treatments when possible, favoring the implementation of computer prescription order entry, favoring the use of the oral route over the parenteral route, and implementing computers in the preparation areas to avoid the use of paper guides.
DiscussionIn our study, many ideas have been proposed by hospital pharmacists to improve the sustainability of the medication use process. When assessing these proposals by impact and feasibility, according to our results, shorten as much as possible the duration of treatments, computerization of the medication use process and oral administration over intravenous should be prioritized in order to reduce environmental impact.
La gestión sostenible de los residuos sanitarios tiene un impacto positivo en el medio ambiente mundial. Para reducirlo, es esencial la práctica sostenible del proceso farmacoterapéutico en todas sus etapas.
ObjetivoAnalizar las estrategias de sostenibilidad propuestas por el servicio de farmacia para reducir los residuos de medicamentos derivados del proceso farmacoterapéutico. Objetivos secundarios: Analizar la etapa del proceso farmacoterapéutico y el número y tipo de medicamentos implicados.
MétodosEl estudio se realizó en un hospital de tercer nivel. Para coordinar las propuestas se seleccionó un farmacéutico referente de cada área del servicio de farmacia. Se evaluaron cuatro etapas del proceso (Adquisición, validación, dispensación y formulación), se clasificaron los pacientes afectados como ambulatorios u hospitalizados y se analizaron los fármacos potencialmente implicados según la vía de administración: oral o parenteral.
ResultadosSe propusieron 28 ideas, que podrían afectar a más de 1.200 medicamentos. El 39,3% afectarían al proceso de validación, el 17,9% a la gestión, el 17,9% a la dispensación y el 7,1% a la formulación. Se evaluó la viabilidad de la aplicación y la aceptabilidad de estas propuestas. Las de mayor potencial fueron: limitar la duración de los tratamientos cuando sea posible, favorecer la implantación de la entrada de órdenes de prescripción por ordenador, favorecer el uso de la vía oral frente a la parenteral e implantar ordenadores en las áreas de preparación para evitar el uso de guías en papel.
ConclusionesEn nuestro estudio, son muchas las ideas propuestas por los farmacéuticos de hospital para mejorar la sostenibilidad del proceso de utilización de medicamentos. A la hora de valorar estas propuestas por impacto y viabilidad, según nuestros resultados, acortar al máximo la duración de los tratamientos, la informatización del proceso de uso de la medicación y la administración oral frente a la intravenosa deberían ser prioritarias para reducir el impacto ambiental.
Sustainable management of healthcare waste has a positive impact on the global environment.1 Available data reflect that more than half of the world's population is at risk of health damage from improperly treated healthcare waste.
The report on the global climate footprint of healthcare published in 2019 by Health Care Without Harm shows that healthcare accounts for 4.4% of global net emissions worldwide. In addition, healthcare activity generates an amount of greenhouse gas emissions that place it in fifth place according to this report. At the national level, the carbon footprint attributable to the healthcare sector has been estimated at 4.5% of the national total.2
Most of the medical waste, around 80%, is classify as low risk, unless it is burned, in which case it releases hazardous gases and compounds such as hydrochloric acid, dioxin and phorones, as well as toxic metals such as lead, cadmium and mercury. Combustion also generates large amounts of CO2 which contributes to global warming.3
Specifically speaking about medicines, waste management refers to any pharmaceutical product that remains unused or is not fully consumed throughout the supply and use chain.1 Thus, the disposal of medicines not administered to the patients causes an annual loss of up to $5.4 billion in the United States4 and around £300 million in the United Kingdom.5 Although most of the contamination derived from medicines is caused by human excreta because of taking them,6 the contribution of improper disposal of unused medicines cannot be underestimated.7 In many countries, it is common for sewage or household garbage to still be used as a disposal route for leftover medicines, resulting directly in their accumulation in the environment.8 Medicines are vital components of modern health care, but their contamination of global waterways is threatening environmental and human health, contributing to biodiversity loss, driving antimicrobial resistance, and jeopardizing progress toward the sustainable development goals.9
Although waste disposal management is a priority, it is important to start not generating avoidable waste from medicines that are not taken. For example, patients who do not use all the medication dispensed to them or who discontinue treatment early as a result of adverse events or lack of efficacy10,11 A Portuguese study showed that on average, out of the medicines kept at home, 72% were not in use, and 8% were mostly expired products ready to discard.12,13
There are some studies that evaluate how to reduce pharmaceutical residues in the environment such us Boxall et al. who suggested switching problematic active pharmaceutical ingredients with “greener” compounds; improve drug delivery to allow for smaller doses to; changes to prescribing practices; and improved wastewater treatment.14 Other studies analyze the environmental policies of different countries affecting pharmaceutical pollution and how the disparities have an impact on this matter.15
In order to contribute to reduce drug waste, it is essential to practice a sustainable pharmacotherapeutic process (PTP) in each of its phases, from procurement to compounding. Many studies have analyzed different methods and procedures to accomplish the sustainable PTP, for example, the eco-directed sustainable prescribing (EDSP) tools suggested by Helwig et al., guidelines to the prescribers toward the least harmful medicine that is therapeutically appropriate.16
Aware of this problem, the pharmacy service (PS) has suggested a series of sustainability proposals to minimize the environmental impact derived from the use of medicines:
Proposals for the sustainability of the PTP:
1. Procurement: prioritize the purchase of medicines manufactured by companies committed to the environment, for example, those that have unit dose presentation with QR code, that use recyclable packaging, generate less waste, or have a record of the carbon footprint of the medicines they manufacture.
2. Prescription: promote the prescription of medicines with a lower carbon footprint. Prioritize, as far as possible, prescriptions of medication that generate less waste, such as, medicines with a once-daily administration schedule as opposed to several times a day, stimulate the use of oral administration over parenteral, limiting treatments´ duration of whenever it is possible.
3. Dispensing: facilitate the use of drugs that do not require repackaging because they are correctly labeled. Minimize the use of plastics to dispense medications to hospitalized and non-hospitalized patients.
4. Compounding: considering the established requirements, prioritize preparations that generate less waste and evaluate the possibility of reusing or recycling the materials used in the compounding process. For example, some studies show that increasing the frequency of medication batch preparations or scheduling patients with the same therapy on the same day can reduce medication waste and expenditures17,18.
Therefore, this study aims to provide an overview of waste generation related to the use of medicines and to analyze the impact of these measures on the minimization of waste that can contribute to the sustainable supply and use of medicines at the hospital level.
The main objective of this study is to analyze the sustainability strategies (SS) proposed by the PS and their degree of implementation in order to reduce the environmental impact of the PTP from drug acquisition to compounding.
As secondary objetives, to analyze the number and type of medicines implicated classifying them between oral and parenteral. Also, to analyze the type of patients who would beneficiate from these measures dividing them into hospitalized or outpatients and to analyze which of the initial proposals for waste reduction in each of the process phases are incorporated into the work procedures of the different areas of the pharmacy service.
MethodsThis is a prospective observational study of the sustainability of the PTP in a PS.
The study has been carried out by pharmacists of the Hospital Universitario La Paz (HULP), which is a 1350-bed tertiary hospital. The researchers were selected from each of the areas involved in the study and they were responsible for coordinating and evaluating the degree of implementation of the different SS. The total of researchers were 15 pharmacists including 4 residents and 11 specialists, from the: purchase and management, dispensation, validation, clinical trials, oncology, outpatients, parenteral nutrition, and quality and safety pharmacy departments. All of them reported sustainability interventions regarding their area of expertise and based on the activities and needs of the hospital service, following a structure questionnaire that included:
- -
The action proposed
- -
Type of patient who would benefit from it: outpatient, hospitalized patient or both
- -
Phase of the pharmacotherapeutic process that would be affected: purchase, validation, dispensation, or compounding.
- -
Administration route that would be affected: oral, parenteral or both
- -
Feasibility of the action from 1 to 3
- -
Impact of the action from 1 to 3
To evaluate feasibility, it was considered 3 points (high) if the intervention was highly feasible due to its relevance, resource availability and acceptability, 2 points (moderate) if it was feasible, although it presented some difficulties in terms of resource availability and/or acceptability and 1 point (low) if it was not feasible because of carrying it out.
To evaluate impact, it was considered 3 points if the intervention had a very relevant impact for the hospital and results in very significant improvements when talking about sustainability, 2 points if it had a moderate impact and some improvements and 1 point if the intervention had a low impact for the hospital and did not involve significant improvements.
These questionnaires were delivered to the responsible of each area in October 2022 and were collected in November 2022 for analysis.
As inclusion criteria: any sustainability intervention related to each of the phases of the pharmacotherapeutic process.
As data sources: the working procedures of the pharmacy service, the FarmaTools® program (version 5.0) and the electronic medical record (HCIS®) were used to obtain the type of patient that would be affected by the proposals as well as the medication that is likely to limit its duration in time and the possibility of switching to another route of administration. Also interviews with the health professionals were involved.
To analyze the number of drugs involved in the study, the hospital's computer technicians used the Farmatools program to analyze all the active ingredients available in the hospital. Subsequently, all drugs whose administration was neither oral nor intravenous were eliminated.
Prior to implementation, this study was approved by the hospital's Clinical Research Ethics Committee, and each pharmacist gave consent to participate in the study.
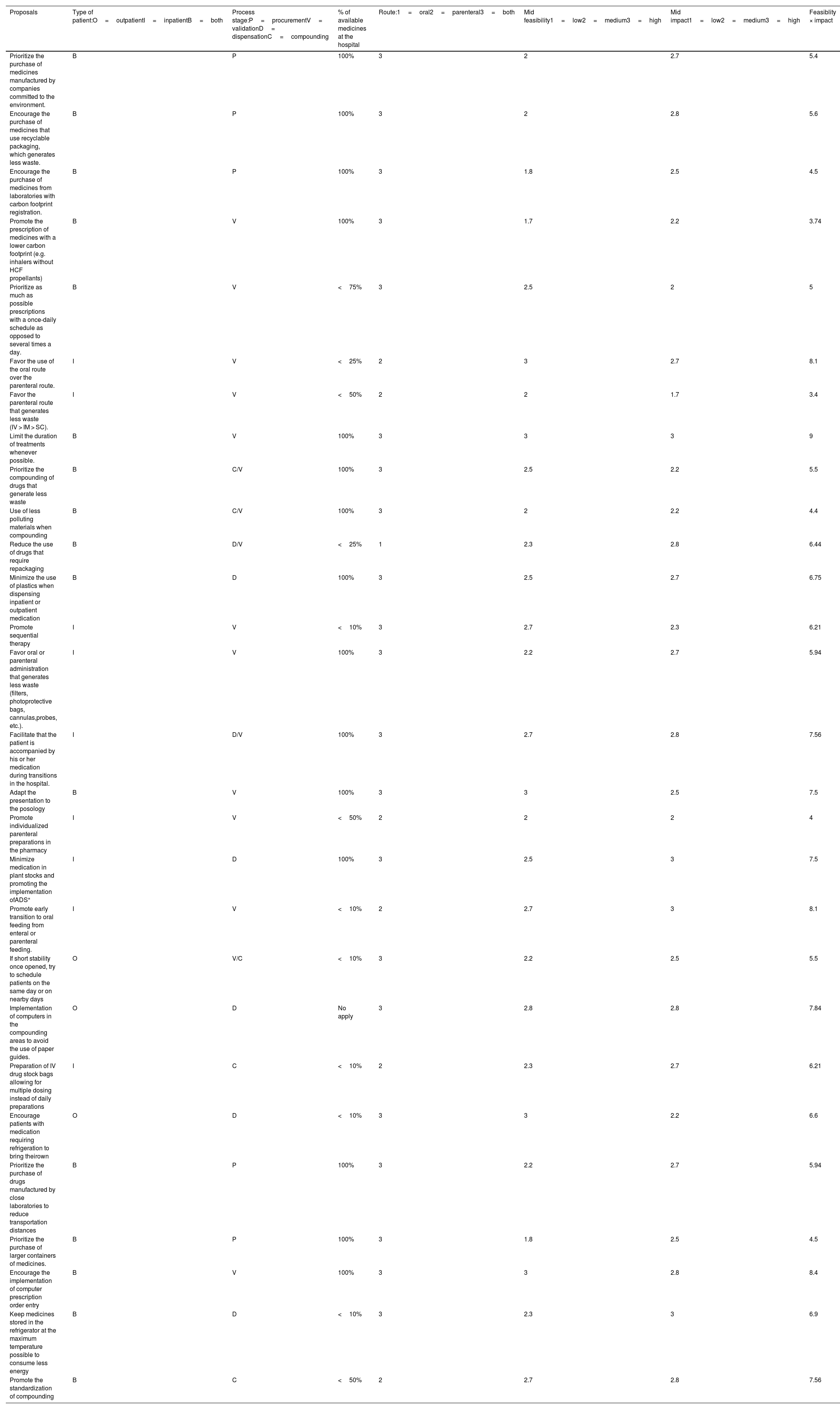
ResultsAs it shown in Table 1, 28 ideas were proposed to improve the sustainability of PFP in the hospital, which could affect to more than 1200 drugs. 57,1% of these proposals would affect both outpatients and hospitalized patients, 32,1% only hospitalized and 10,7% only outpatients.
Sustainability proposals.
| Proposals | Type of patient:O=outpatientI=inpatientB=both | Process stage:P=procurementV= validationD= dispensationC=compounding | % of available medicines at the hospital | Route:1=oral2=parenteral3=both | Mid feasibility1=low2=medium3=high | Mid impact1=low2=medium3=high | Feasiblity × impact |
|---|---|---|---|---|---|---|---|
| Prioritize the purchase of medicines manufactured by companies committed to the environment. | B | P | 100% | 3 | 2 | 2.7 | 5.4 |
| Encourage the purchase of medicines that use recyclable packaging, which generates less waste. | B | P | 100% | 3 | 2 | 2.8 | 5.6 |
| Encourage the purchase of medicines from laboratories with carbon footprint registration. | B | P | 100% | 3 | 1.8 | 2.5 | 4.5 |
| Promote the prescription of medicines with a lower carbon footprint (e.g. inhalers without HCF propellants) | B | V | 100% | 3 | 1.7 | 2.2 | 3.74 |
| Prioritize as much as possible prescriptions with a once-daily schedule as opposed to several times a day. | B | V | <75% | 3 | 2.5 | 2 | 5 |
| Favor the use of the oral route over the parenteral route. | I | V | <25% | 2 | 3 | 2.7 | 8.1 |
| Favor the parenteral route that generates less waste (IV > IM > SC). | I | V | <50% | 2 | 2 | 1.7 | 3.4 |
| Limit the duration of treatments whenever possible. | B | V | 100% | 3 | 3 | 3 | 9 |
| Prioritize the compounding of drugs that generate less waste | B | C/V | 100% | 3 | 2.5 | 2.2 | 5.5 |
| Use of less polluting materials when compounding | B | C/V | 100% | 3 | 2 | 2.2 | 4.4 |
| Reduce the use of drugs that require repackaging | B | D/V | <25% | 1 | 2.3 | 2.8 | 6.44 |
| Minimize the use of plastics when dispensing inpatient or outpatient medication | B | D | 100% | 3 | 2.5 | 2.7 | 6.75 |
| Promote sequential therapy | I | V | <10% | 3 | 2.7 | 2.3 | 6.21 |
| Favor oral or parenteral administration that generates less waste (filters, photoprotective bags, cannulas,probes, etc.). | I | V | 100% | 3 | 2.2 | 2.7 | 5.94 |
| Facilitate that the patient is accompanied by his or her medication during transitions in the hospital. | I | D/V | 100% | 3 | 2.7 | 2.8 | 7.56 |
| Adapt the presentation to the posology | B | V | 100% | 3 | 3 | 2.5 | 7.5 |
| Promote individualized parenteral preparations in the pharmacy | I | V | <50% | 2 | 2 | 2 | 4 |
| Minimize medication in plant stocks and promoting the implementation ofADS⁎ | I | D | 100% | 3 | 2.5 | 3 | 7.5 |
| Promote early transition to oral feeding from enteral or parenteral feeding. | I | V | <10% | 2 | 2.7 | 3 | 8.1 |
| If short stability once opened, try to schedule patients on the same day or on nearby days | O | V/C | <10% | 3 | 2.2 | 2.5 | 5.5 |
| Implementation of computers in the compounding areas to avoid the use of paper guides. | O | D | No apply | 3 | 2.8 | 2.8 | 7.84 |
| Preparation of IV drug stock bags allowing for multiple dosing instead of daily preparations | I | C | <10% | 2 | 2.3 | 2.7 | 6.21 |
| Encourage patients with medication requiring refrigeration to bring theirown | O | D | <10% | 3 | 3 | 2.2 | 6.6 |
| Prioritize the purchase of drugs manufactured by close laboratories to reduce transportation distances | B | P | 100% | 3 | 2.2 | 2.7 | 5.94 |
| Prioritize the purchase of larger containers of medicines. | B | P | 100% | 3 | 1.8 | 2.5 | 4.5 |
| Encourage the implementation of computer prescription order entry | B | V | 100% | 3 | 3 | 2.8 | 8.4 |
| Keep medicines stored in the refrigerator at the maximum temperature possible to consume less energy | B | D | <10% | 3 | 2.3 | 3 | 6.9 |
| Promote the standardization of compounding | B | C | <50% | 2 | 2.7 | 2.8 | 7.56 |
39.3% of the proposals were suggested with reference to the validation process, 17.9% to procurement management, 17,9% to drug dispensing and 7.1% to the drug compounding process. In addition, 10,7% of the ideas could be applied to both the validation and compounding processes and 7,1% to the validation and dispensing processes.
Of these ideas, 53.6% would affect the total number of drugs used in the hospital and 14.3% would affect more than 50% of them. Twenty-one of these proposals would affect both oral and parenteral drugs, 6 of them only parenteral drugs and 1 exclusively oral drugs.
To stratify the proposed measures, the feasibility and acceptability of implementation were scored from 1 to 3. Thus, after multiplying both, priority 1 (score 8–9), priority 2 (score 5–7), priority 3 (score 1–4) were established. Out of all the analyzed proposals, those with the greatest potential for feasibility and whose impact would be greatest (priority 1) were:
- Limit the duration of treatments whenever possible. For example, limiting the treatment with granulocyte-colony stimulating factor until the end of chemotherapy and recovery of neutropenia.
- Encourage the implementation of computer prescription order entry.
- Encourage the use of oral versus parenteral drugs. For example, sequential therapy with antibiotics or antifungals: intravenous voriconazole 4 mg/kg/12 h for oral voriconazole 200–300 mg/12 h or switching intravenous acetaminophen to oral acetaminophen when tolerated by the patient.
- Computer implementation in the preparation areas to avoid the use of paper guides.
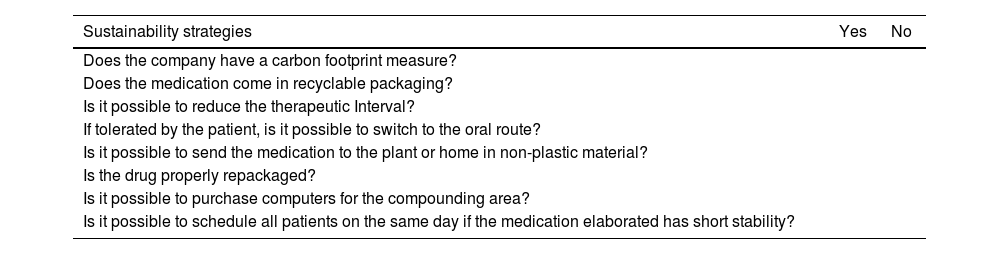
Taken into account the sustainability proposals we developed a checklist according to our results. This document could be useful to promote the PTP sustainability in hospital pharmacy departments (Table 2).
Sustainability strategies checklist.
| Sustainability strategies | Yes | No |
|---|---|---|
| Does the company have a carbon footprint measure? | ||
| Does the medication come in recyclable packaging? | ||
| Is it possible to reduce the therapeutic Interval? | ||
| If tolerated by the patient, is it possible to switch to the oral route? | ||
| Is it possible to send the medication to the plant or home in non-plastic material? | ||
| Is the drug properly repackaged? | ||
| Is it possible to purchase computers for the compounding area? | ||
| Is it possible to schedule all patients on the same day if the medication elaborated has short stability? | ||
Hospital pharmacists could undertake different activities to limit medication waste in all stages of the PTP.19
In our study, many ideas have been proposed by hospital pharmacists to improve the sustainability of the medication use process. When assessing these proposals by impact and feasibility, according to our results, shorten as much as possible the duration of treatments, computerization of the medication use process and oral administration over intravenous should be prioritized in order to reduce environmental impact.
Contribution to the scientific literatureThis research provides an analysis of different measures that hospital pharmacists can take to ensure a more sustainable PTP, as well as the feasibility of carrying them out. In addition, our article can serve as a reference for other hospitals interested in making the activities on different pharmacy departments more sustainable.
Authorship declarationAll the authors have contributed to the collection and analysis of the data in this study, as well as to the writing and critical review according to their area of reference. All have participated in the approval of the final version for publication.
FundingNone.
We would like to thank Sara Heinz, Leire Garcia, Elena Rodriguez, Natalia García, Francisco Ramos, Pilar Gómez-Salcedo, Gema Casado and all the pharmacy staff helping us to carry out this study.