The main purpose of this study was to analyze and compare three different medication delivery methods used by the outpatient care unit of a hospital pharmacy, namely health center collection, community pharmacy collection and home delivery. The secondary purpose was to compare the economic cost of those methods for the Spanish health service.
MethodA failure mode and effects analysis was carried out to attain the primary objective. For the secondary objective, an in-depth analysis was performed of the economic costs associated with each program using a cost-minimization analysis.
ResultsThe failure mode and effects analysis resulted in scores of 184, 170 and 126 points for the health center collection, home delivery and community pharmacy collection programs, respectively. The economic evaluation, for its part, rendered estimated costs of €18,434.52, €11,417.08 and €7,986.52 for home delivery, health center collection and community pharmacy collection services, respectively.
ConclusionsThe results of the study indicated that collection at the community pharmacy was the program associated to the lowest risk, most likely due to the crucial role of the pharmacist regarding the custody and preservation of medicines. As regards cost, dispensation at the community pharmacy was also associated with the lowest cost. Nevertheless, this finding was biased by the fact that, given the generous collaboration of pharmaceutical distributors during the COVID-19 pandemic, the cost of transport and delivery to the pharmacy during the study period was zero. Further economic analyses are required to evaluate the costs of community pharmacy delivery and determine their impact on the public health system in cases where transport costs are different from zero.
El objetivo principal fue evaluar y comparar tres programas de entrega de medicamentos requeridos por los pacientes atendidos en las consultas externas de farmacia hospitalaria: mediante centros de salud, empresa de mensajería externa y oficinas de farmacia. El objetivo secundario fue analizar el coste económico desde la perspectiva del sistema público de salud.
MétodoSe utilizó el análisis modal de fallos y efectos para el objetivo principal. El análisis económico se realizó mediante un estudio de minimización de costes.
ResultadosLos resultados en índice de probabilidad de riesgo fueron 184 puntos para la entrega mediante centros de salud, 170 mediante mensajería y 126 mediante oficina de farmacia. El estudio económico mostró que actualmente el programa con menor coste económico fue la dispensación mediante oficina de farmacia respecto a mensajería y centros de salud (7.986,52 € versus 18.434,52 € y 11.417,08 €).
ConclusionesLa entrega mediante oficina de farmacia tiene el menor índice de probabilidad de riesgo debido en gran parte al papel del farmacéutico en la custodia y conservación del medicamento. Respecto al estudio económico, también la dispensación mediante oficina de farmacia obtuvo el menor coste pero con una importante limitación: fue asignado un coste cero relativo a la empresa distribuidora y a la entrega del medicamento en las oficinas de farmacia por la colaboración altruista durante la pandemia. Si el coste fuese distinto de cero, serán necesarios nuevos estudios para evaluar el impacto económico el sistema público de salud.
Nowadays, the use of telemedicine in medical consultations and in the outpatient care unit of hospital pharmacies is becoming increasingly widespread due to the need to reduce the risk of infection by SARS-CoV-21,2.
The term telepharmacy has recently been consensually defined by the Spanish Society of Hospital Pharmacists (SEFH) as the delivery of pharmaceutical services at a distance through the use of information and telecommunication technologies. It is considered to have four main applications: pharmacotherapeutic follow-up; training of and information to patients; coordination between the members of the care team; and dispensation and informed delivery of drugs to make them more accessible to patients. The traditional pharmaceutical care model, centered mainly on medications themselves, has been all but replaced by a new model based on capacity, motivation, and opportunity (CMO model). By virtue of this model, interactions between the pharmacist, other healthcare providers and the patient revolve around the latter's needs and the attainment of specific pharmacotherapeutic goals and the incorporation of such new technologies as may allow continuous interaction with the patient and an improvement of health outcomes, with due consideration to the system's overall efficiency. At present, the dispensation of medicines onsite at the outpatient hospital pharmacy is being restricted by many hospitals as a result of the increasing influx of patients following the COVID 19 healthcare emergency, which has led to the overcrowding of many pharmacy departments. The crisis has indeed made it necessary to implement a series of alternative drug delivery programs3–5.
Against this background, the Serrania de Malaga health area has seen the need to reformulate the drug dispensing and delivery model used by the outpatient care unit of its hospital pharmacy departments (HPDs) in an attempt to enhance patient safety and minimize the epidemiologic risk associated with onsite dispensing programs. The failure mode and effects analysis (FMEA) methodology has been widely used as a generic risk analysis tool and, more specifically, as a way to determine the risks inherent in different drug dispensing programs. This method, designed to allow a systematic and prospective evaluation of complex processes, is capable of preventively identifying failure modes and anticipating their effects based on their likelihood of occurrence, the potential severity of the damage caused, and their detectability. In the context of drug dispensation, FMEA helps anticipate the potential risks that different delivery strategies could entail for both patients and healthcare providers and select the one associated with the lowest risk6,7.
The main goal of this study was to apply the FMEA methodology to determine the risks associated with three programs used by HPDs to dispense medications. The secondary goal was to analyze economic costs from the point of view of the public health system, specifically Andalusia's regional health system.
MethodsThis is a prospective, analytical cohort study of three different drug dispensing programs implemented by an HPD: delivery by courier (COU), health center collection (HCC) and delivery at a community pharmacy (PHA).
A literature search was performed in Pubmed and Embase of the following keywords: “Failure Mode and Effects Analysis”, “dispensing”, “pharmaceutical service” and “delivery of health care.” The idea was to find studies that looked into the dispensing and delivery of medications to the patients’ doorstep, community pharmacies and health centers. No time filter was applied. Articles in both English and Spanish were analyzed.
The FMEA method was used to evaluate and compare the three medication dispensing methods considered in the study. This required setting up a well-trained team with experience in the field. The team was made up of five seasoned pharmacists, two of them with a community pharmacy background. The target population of the study corresponded to patients who were potential candidates for inclusion in the different medication dispensing programs. After conducting a brainstorming exercise to identify the critical steps in the dispensing programs under analysis, the potential modes of failure as well as the potential causes and effects of failure were determined. No corrective measures were defined as the goal was not to make improvements to any specific dispensing program but to evaluate and compare the risks associated to them. The risk priority number (RPN) for each failure mode was calculated by multiplying the values of the following three parameters: “P” (probability of failure), “S” (severity of the effect of a potential failure); and “D” (failure detectability) (RPN=PxSxD). Each parameter was assigned a score between 1 and 4, which means that the RPN for each failure mode ranged between a minimum of 1 and a maximum of 64. Probability of failure measured the likelihood that the currently existing controls might fail, a score of 1 denoting a remote probability and a score of 4 denoting a high probability. Severity of the effect of a potential failure measured the negative consequences the failure would have for the patient or the healthcare system, a score of 1 indicating l a low impact and a score of 4 indicating a catastrophic effect. Failure detectability measured the likelihood of failure detection, a score of 1 indicating ease of detection and a score of 4 indicating undetectability. For each of the three programs, the members of the group consensually assigned a score to the different parameters corresponding to the failure modes associated with each critical step and calculated the RPN of the different failure modes in each program. Subsequently, the RPN for each critical step was calculated. Finally, the RPNs of the different critical steps in each program were added up to allow a comparison across the three programs. The median of the differences between the higher and the lower RPN value was used to establish a cutoff point to determine whether the risk of failure differences observed were significant for each of the critical steps in the three programs.
The economic assessment was made through a cost minimization analysis based on the methodology proposed by López Bastida et al.8 It was estimated that one-third of all patients seen to at the outpatient care unit of an HPD could benefit from being included in a medications delivery program. The analysis was carried out from the point of view of Andalusia's public health system.
- 1.
Resources used.
- 1.1.
Human resources: a specialist hospital pharmacist, a community pharmacist, a hospital pharmacy technician, an administrative clerk, and an orderly/driver.
- 1.2.
Material resources:
- 1.2.1.
Packaging material consisting in sealed 180 x 260 mm padded envelopes, 35 x 89 mm labels, thermometers, and medicine refrigerators.
- 1.2.1.
- 1.1.
- 2.
Costs. The estimated cost of the three medication delivery programs was calculated based on a frequency of 4 shipments per patient/year. It was estimated that 60% of patients required treatment with cold-stored medicines (between 2 and 8 °C) and 40% required treatment with medicines stored at room temperature (between 8 and 25 °C). It was estimated that 5% of all drugs shipped would be returned.
- 2.1.
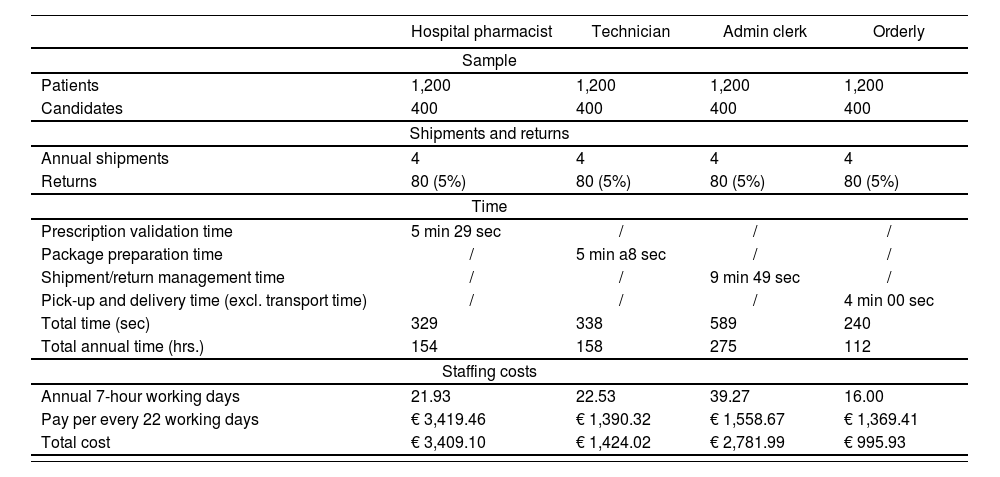
Cost of human resources. These costs were estimated as a function of the time dedicated by each person involved. For this purpose, a simulation was put together consisting in the preparation, shipment, and collection of 5 drug treatments corresponding to five patients randomly selected from all the patients seen to at the outpatient care unit. Subsequently, the arithmetic mean of the time consumed by each process was calculated. The time dedicated by each staff member to manage potential returns was also considered. Finally, time units were transformed into cost units (expressed in euros), using the pay scales stipulated in Resolution 0004/2020, which establishes the remuneration of the staff working for Andalusia's health system.
- 2.2.
Cost of the packaging materials. To calculate this cost, we used the retail prices contemplated in the Integrated Logistics Management System of Andalusia's health system (SIGLO).
- 2.3.
Specific cost of each dispensing program.
- 2.3.1.
The cost of shipping the medication through a courier service was estimated using the mean price charged by two different courier firms for shipping packages under 2 kg within our health area, making a distinction between room-temperature and refrigerated shipments. An additional 5% cost was included for returns.
- 2.3.2.
To estimate the cost of shipping the medication by means of an orderly/driver, we considered the cost of fuel as a function of the number of kilometers traveled by a transport vehicle within our health area. This required the calculation of the mean annual fuel consumption. The cost of two 25 L portable medicine refrigerators and two thermometers was also included, using the prices listed in the SIGLO system.
- 2.3.3.
The cost of shipping the medication to a community pharmacy through a pharmaceutical distributor was obtained from the hospitals in Andalusia's health system that use the PHA delivery program.
- 2.3.1.
- 2.1.
No FMEA analyses of the dispensing and delivery of medicines from an HPD to the patient's home, a community pharmacy or a health center were found in the literature.
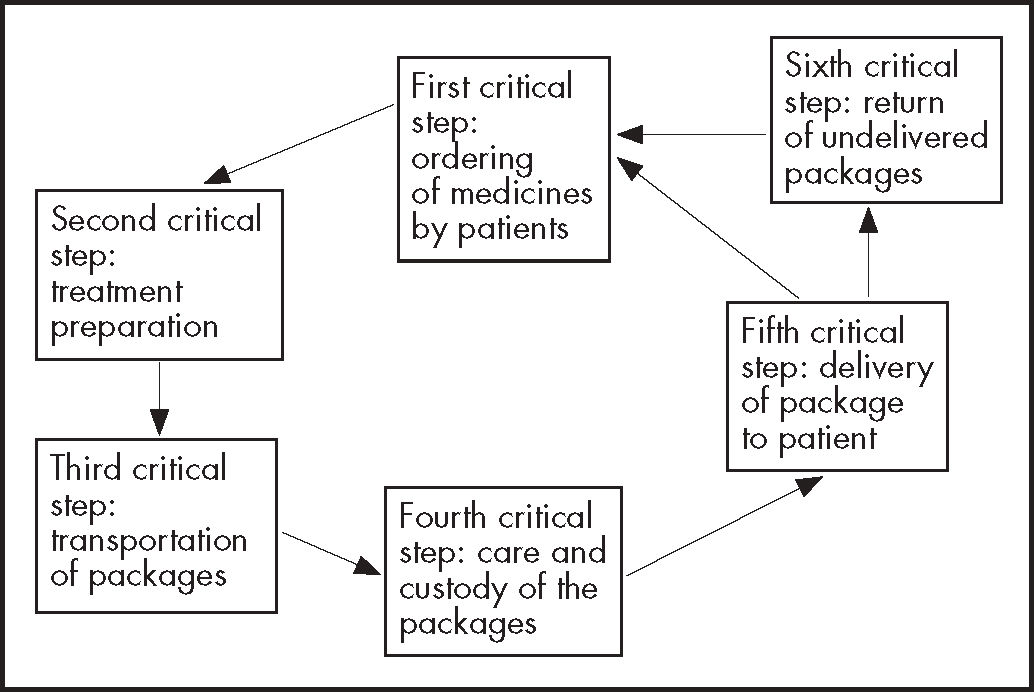
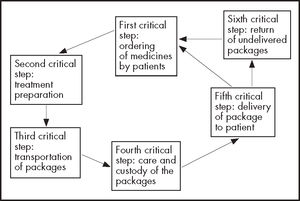
The evaluating team identified six critical steps, common to the three dispensing and delivery programs, namely: 1) ordering of the medicines by patients from the pharmacist responsible for the HPD; 2) insertion of each patient's treatment in clearly identified envelopes; 3) transportation of packages containing each patient's medicines from the HPD to the patient's home, community pharmacy or health canter, using a courier company, a pharmaceutical distributor, or an orderly/driver, respectively; 4) care and custody of packages at intermediate logistics platforms; 5) delivery of the packages to patients; and 6) return of undelivered packages (Figure 1).
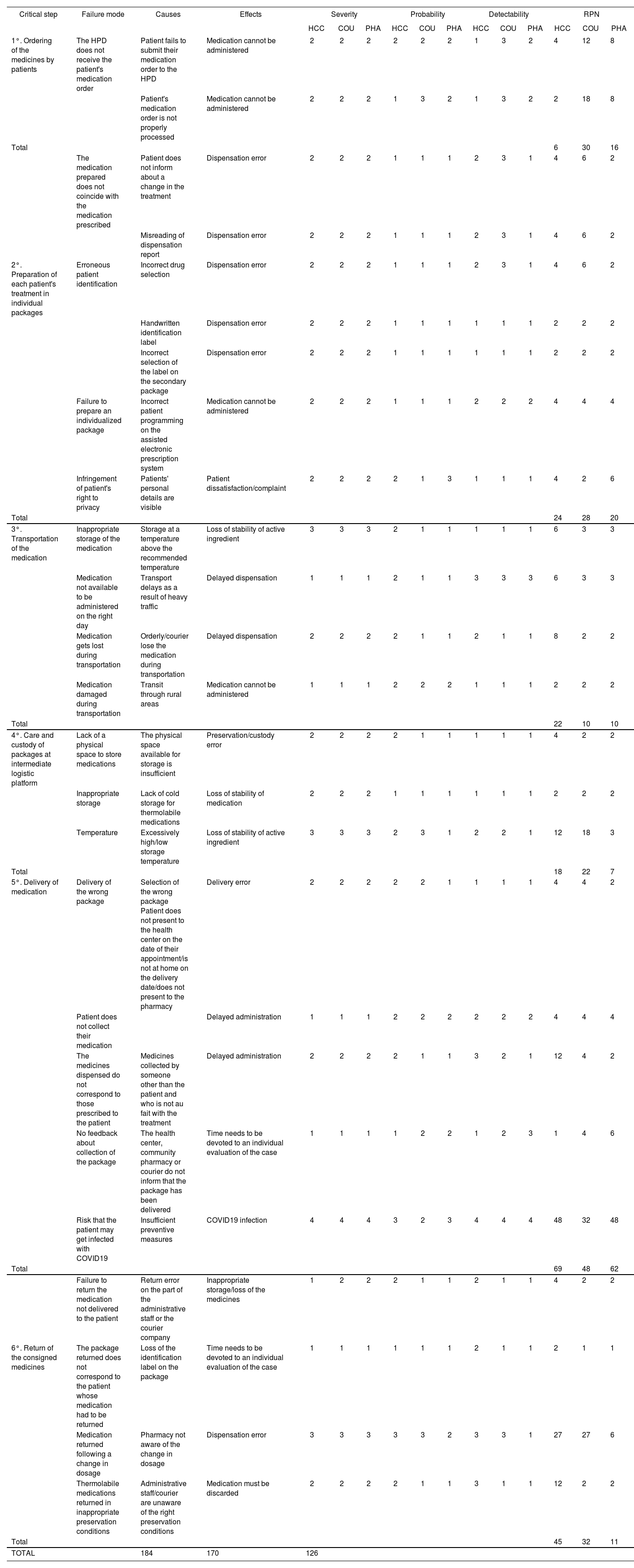
The FMEA analysis revealed that the three dispensing programs (HCC, COU, PHA) had a cumulative RPN of 184, 170 and 126 points, respectively (Table 1), i.e. absolute RPN differences were 58, 14 and 44. For each critical step, an RPN cut-off point of 18 was obtained above which failure risk differences between the programs were to be regarded as significant. This means that the three dispensing programs were set significantly apart by the risk of failure of critical steps 1, 5 y 6, with RPN differences between the highest and the lowest scores of 24, 12, 15, 21 and 34 points, respectively (see Table 1).
Failure Mode and Effects Analysis of the COU, HCC and PHA programs
| Critical step | Failure mode | Causes | Effects | Severity | Probability | Detectability | RPN | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HCC | COU | PHA | HCC | COU | PHA | HCC | COU | PHA | HCC | COU | PHA | ||||
| 1°. Ordering of the medicines by patients | The HPD does not receive the patient's medication order | Patient fails to submit their medication order to the HPD | Medication cannot be administered | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 3 | 2 | 4 | 12 | 8 |
| Patient's medication order is not properly processed | Medication cannot be administered | 2 | 2 | 2 | 1 | 3 | 2 | 1 | 3 | 2 | 2 | 18 | 8 | ||
| Total | 6 | 30 | 16 | ||||||||||||
| The medication prepared does not coincide with the medication prescribed | Patient does not inform about a change in the treatment | Dispensation error | 2 | 2 | 2 | 1 | 1 | 1 | 2 | 3 | 1 | 4 | 6 | 2 | |
| Misreading of dispensation report | Dispensation error | 2 | 2 | 2 | 1 | 1 | 1 | 2 | 3 | 1 | 4 | 6 | 2 | ||
| 2°. Preparation of each patient's treatment in individual packages | Erroneous patient identification | Incorrect drug selection | Dispensation error | 2 | 2 | 2 | 1 | 1 | 1 | 2 | 3 | 1 | 4 | 6 | 2 |
| Handwritten identification label | Dispensation error | 2 | 2 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 2 | 2 | ||
| Incorrect selection of the label on the secondary package | Dispensation error | 2 | 2 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 2 | 2 | ||
| Failure to prepare an individualized package | Incorrect patient programming on the assisted electronic prescription system | Medication cannot be administered | 2 | 2 | 2 | 1 | 1 | 1 | 2 | 2 | 2 | 4 | 4 | 4 | |
| Infringement of patient's right to privacy | Patients' personal details are visible | Patient dissatisfaction/complaint | 2 | 2 | 2 | 2 | 1 | 3 | 1 | 1 | 1 | 4 | 2 | 6 | |
| Total | 24 | 28 | 20 | ||||||||||||
| 3°. Transportation of the medication | Inappropriate storage of the medication | Storage at a temperature above the recommended temperature | Loss of stability of active ingredient | 3 | 3 | 3 | 2 | 1 | 1 | 1 | 1 | 1 | 6 | 3 | 3 |
| Medication not available to be administered on the right day | Transport delays as a result of heavy traffic | Delayed dispensation | 1 | 1 | 1 | 2 | 1 | 1 | 3 | 3 | 3 | 6 | 3 | 3 | |
| Medication gets lost during transportation | Orderly/courier lose the medication during transportation | Delayed dispensation | 2 | 2 | 2 | 2 | 1 | 1 | 2 | 1 | 1 | 8 | 2 | 2 | |
| Medication damaged during transportation | Transit through rural areas | Medication cannot be administered | 1 | 1 | 1 | 2 | 2 | 2 | 1 | 1 | 1 | 2 | 2 | 2 | |
| Total | 22 | 10 | 10 | ||||||||||||
| 4°. Care and custody of packages at intermediate logistic platform | Lack of a physical space to store medications | The physical space available for storage is insufficient | Preservation/custody error | 2 | 2 | 2 | 2 | 1 | 1 | 1 | 1 | 1 | 4 | 2 | 2 |
| Inappropriate storage | Lack of cold storage for thermolabile medications | Loss of stability of medication | 2 | 2 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 2 | 2 | |
| Temperature | Excessively high/low storage temperature | Loss of stability of active ingredient | 3 | 3 | 3 | 2 | 3 | 1 | 2 | 2 | 1 | 12 | 18 | 3 | |
| Total | 18 | 22 | 7 | ||||||||||||
| 5°. Delivery of medication | Delivery of the wrong package | Selection of the wrong package Patient does not present to the health center on the date of their appointment/is not at home on the delivery date/does not present to the pharmacy | Delivery error | 2 | 2 | 2 | 2 | 2 | 1 | 1 | 1 | 1 | 4 | 4 | 2 |
| Patient does not collect their medication | Delayed administration | 1 | 1 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 4 | 4 | 4 | ||
| The medicines dispensed do not correspond to those prescribed to the patient | Medicines collected by someone other than the patient and who is not au fait with the treatment | Delayed administration | 2 | 2 | 2 | 2 | 1 | 1 | 3 | 2 | 1 | 12 | 4 | 2 | |
| No feedback about collection of the package | The health center, community pharmacy or courier do not inform that the package has been delivered | Time needs to be devoted to an individual evaluation of the case | 1 | 1 | 1 | 1 | 2 | 2 | 1 | 2 | 3 | 1 | 4 | 6 | |
| Risk that the patient may get infected with COVID19 | Insufficient preventive measures | COVID19 infection | 4 | 4 | 4 | 3 | 2 | 3 | 4 | 4 | 4 | 48 | 32 | 48 | |
| Total | 69 | 48 | 62 | ||||||||||||
| Failure to return the medication not delivered to the patient | Return error on the part of the administrative staff or the courier company | Inappropriate storage/loss of the medicines | 1 | 2 | 2 | 2 | 1 | 1 | 2 | 1 | 1 | 4 | 2 | 2 | |
| 6°. Return of the consigned medicines | The package returned does not correspond to the patient whose medication had to be returned | Loss of the identification label on the package | Time needs to be devoted to an individual evaluation of the case | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 2 | 1 | 1 |
| Medication returned following a change in dosage | Pharmacy not aware of the change in dosage | Dispensation error | 3 | 3 | 3 | 3 | 3 | 2 | 3 | 3 | 1 | 27 | 27 | 6 | |
| Thermolabile medications returned in inappropriate preservation conditions | Administrative staff/courier are unaware of the right preservation conditions | Medication must be discarded | 2 | 2 | 2 | 2 | 1 | 1 | 3 | 1 | 1 | 12 | 2 | 2 | |
| Total | 45 | 32 | 11 | ||||||||||||
| TOTAL | 184 | 170 | 126 | ||||||||||||
COU: delivery by courier; HCC: health center collection; HPD: hospital pharmacy department; PHA: delivery at a community pharmacy; RPN: risk priority number.
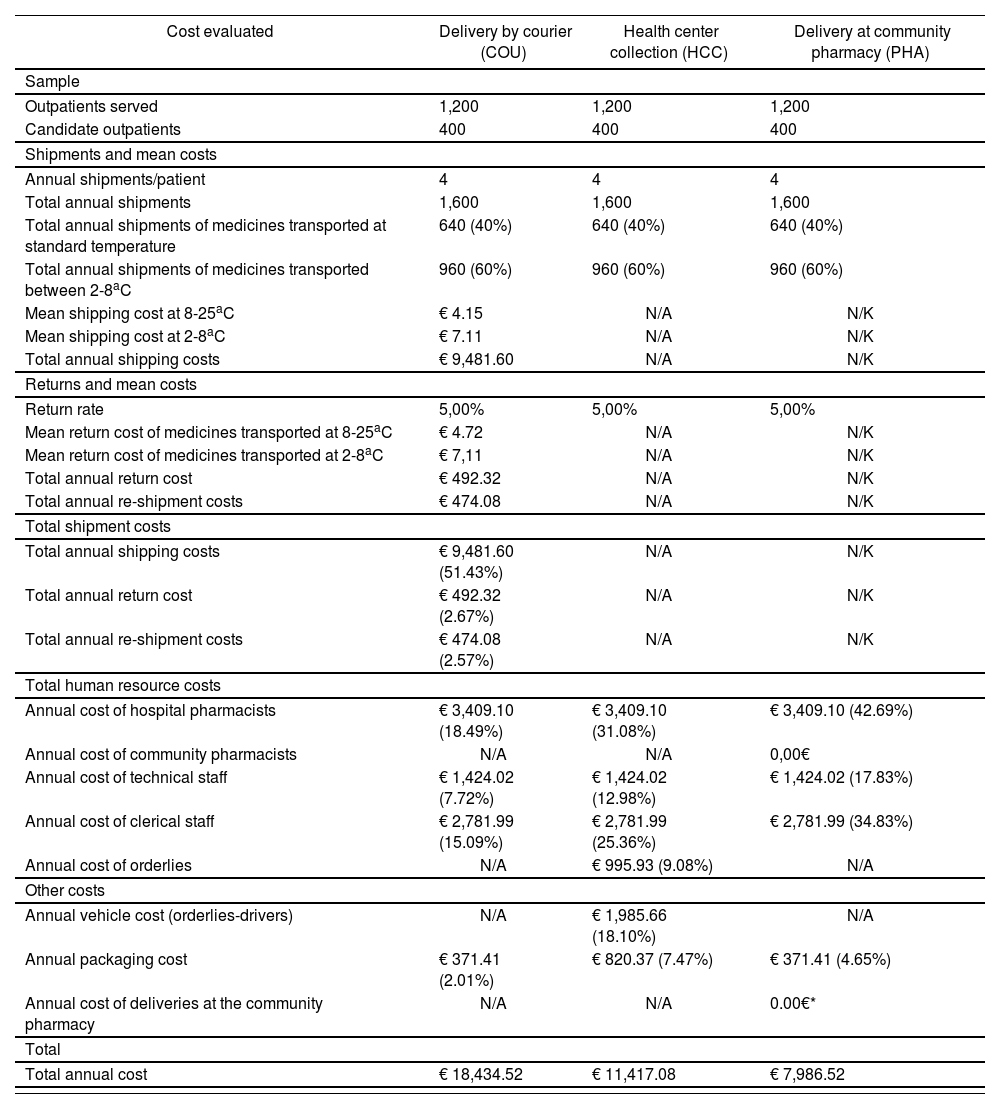
Tables 2 and 3 show the results of the economic evaluation. The most costly delivery program was COU, followed by HCC and PHA (€18,434.52, €11,417.08 and €7,986.52, respectively). The cost of the pharmacist and the pharmaceutical distributor in the PHA program was 0 because of their altruistic collaboration during the COVID-19 pandemic. Packaging costs were higher in the HCC program than in COU and PHA because the latter two programs did not include refrigerators or thermometers.
Overall costs
| Cost evaluated | Delivery by courier (COU) | Health center collection (HCC) | Delivery at community pharmacy (PHA) |
|---|---|---|---|
| Sample | |||
| Outpatients served | 1,200 | 1,200 | 1,200 |
| Candidate outpatients | 400 | 400 | 400 |
| Shipments and mean costs | |||
| Annual shipments/patient | 4 | 4 | 4 |
| Total annual shipments | 1,600 | 1,600 | 1,600 |
| Total annual shipments of medicines transported at standard temperature | 640 (40%) | 640 (40%) | 640 (40%) |
| Total annual shipments of medicines transported between 2-8aC | 960 (60%) | 960 (60%) | 960 (60%) |
| Mean shipping cost at 8-25aC | € 4.15 | N/A | N/K |
| Mean shipping cost at 2-8aC | € 7.11 | N/A | N/K |
| Total annual shipping costs | € 9,481.60 | N/A | N/K |
| Returns and mean costs | |||
| Return rate | 5,00% | 5,00% | 5,00% |
| Mean return cost of medicines transported at 8-25aC | € 4.72 | N/A | N/K |
| Mean return cost of medicines transported at 2-8aC | € 7,11 | N/A | N/K |
| Total annual return cost | € 492.32 | N/A | N/K |
| Total annual re-shipment costs | € 474.08 | N/A | N/K |
| Total shipment costs | |||
| Total annual shipping costs | € 9,481.60 (51.43%) | N/A | N/K |
| Total annual return cost | € 492.32 (2.67%) | N/A | N/K |
| Total annual re-shipment costs | € 474.08 (2.57%) | N/A | N/K |
| Total human resource costs | |||
| Annual cost of hospital pharmacists | € 3,409.10 (18.49%) | € 3,409.10 (31.08%) | € 3,409.10 (42.69%) |
| Annual cost of community pharmacists | N/A | N/A | 0,00€ |
| Annual cost of technical staff | € 1,424.02 (7.72%) | € 1,424.02 (12.98%) | € 1,424.02 (17.83%) |
| Annual cost of clerical staff | € 2,781.99 (15.09%) | € 2,781.99 (25.36%) | € 2,781.99 (34.83%) |
| Annual cost of orderlies | N/A | € 995.93 (9.08%) | N/A |
| Other costs | |||
| Annual vehicle cost (orderlies-drivers) | N/A | € 1,985.66 (18.10%) | N/A |
| Annual packaging cost | € 371.41 (2.01%) | € 820.37 (7.47%) | € 371.41 (4.65%) |
| Annual cost of deliveries at the community pharmacy | N/A | N/A | 0.00€* |
| Total | |||
| Total annual cost | € 18,434.52 | € 11,417.08 | € 7,986.52 |
N/A: not applicable. N/K: not known.
Personnel costs
| Hospital pharmacist | Technician | Admin clerk | Orderly | |
|---|---|---|---|---|
| Sample | ||||
| Patients | 1,200 | 1,200 | 1,200 | 1,200 |
| Candidates | 400 | 400 | 400 | 400 |
| Shipments and returns | ||||
| Annual shipments | 4 | 4 | 4 | 4 |
| Returns | 80 (5%) | 80 (5%) | 80 (5%) | 80 (5%) |
| Time | ||||
| Prescription validation time | 5 min 29 sec | / | / | / |
| Package preparation time | / | 5 min a8 sec | / | / |
| Shipment/return management time | / | / | 9 min 49 sec | / |
| Pick-up and delivery time (excl. transport time) | / | / | / | 4 min 00 sec |
| Total time (sec) | 329 | 338 | 589 | 240 |
| Total annual time (hrs.) | 154 | 158 | 275 | 112 |
| Staffing costs | ||||
| Annual 7-hour working days | 21.93 | 22.53 | 39.27 | 16.00 |
| Pay per every 22 working days | € 3,419.46 | € 1,390.32 | € 1,558.67 | € 1,369.41 |
| Total cost | € 3,409.10 | € 1,424.02 | € 2,781.99 | € 995.93 |
To the best of our knowledge, this is the first study in the literature to apply the FMEA methodology to three different programs used by an HPD to dispense medications to outpatients. The study also analyses the economic impact of such programs from the point of view of Andalusia's public health system.
The study shows that the three medication dispensing programs are very similar in terms of their associated risk of failure, with absolute differences between the programs of 58, 14 and 44 points. In the hypothetical case that all modes of failure under a given program were extremely likely to occur (4/4), with maximum severity (4/4) and maximum detectability (4/4), the cumulative RPN would be 1,600 points whereas, at the opposite end of the spectrum, a perfect program would be assigned a 1/4 score across all failure modes, which would give a total of 25 points. This means that the 58, 14 and 44-point differences mentioned above can be considered negligible if compared with the maximum 1,600 points that could hypothetically be scored by the programs, with HCC and COU obtaining very similar RPNs. From the point of view of each critical step, relevant differences were obtained in steps 1, 5 and 6.
As regards the first critical step, as shown in table 1, a patient's failure to place an order for their required medications was most likely to occur in the COU program, followed by PHA and HCC, and was more easily detectable in the HCC program, followed by PHA and COU, probably because of the continuous interaction between health centers and the HPD under the HCC program through the patients’ electronic medical records. Unfortunately, as our health area does not possess a tool that connects patients with courier companies and pharmaceutical distributors, patients’ failures to place their medication orders were less easy to detect in our COU and PHA programs.
With respect to the fifth critical step, RPN differences were due to several failure modes. Firstly, the medicines dispensed do not correspond to those prescribed to the patient failure mode was easier to detect in the PHA program as community pharmacists are qualified to provide information about the drug whereas couriers and the transportation staff in charge of the deliveries under the COU and HCC programs, respectively, are not. Secondly, the information flow regarding collections from the HPD is more likely to be more efficient and more easily detectable in the HCC program than in the COU and PHA programs, as health centers and the HPD can collaborate through the electronic medical record. Reducing the RPN of the COU and PHA programs in this respect will require the introduction of common technological tools that facilitate the exchange of information, which would probably result in increased costs. Lastly, the evaluating team found that after the outbreak of the COVID-19 pandemic, many HPDs started consigning drugs to patients’ homes and community pharmacies as they considered that this would reduce the risk of COVID-19 infection3. It must be pointed out, however, that regardless of the delivery program used the measures used to prevent COVID-19 infection must always be those recommended by the health authorities9.
Two remarks must be made regarding the sixth critical step (return of the consigned medicines). The first one has to do with the fact that hospital pharmacists may be unaware of changes in patients’ medication regimens. The risk associated with this failure mode was considered higher in the COU and HCC programs, which were assigned an RPN of 27 points each, than in the PHA program (RPN = 6) as it is believed that community pharmacists can act as vehicles to convey information about any dosage change given their specialization and the fact that they have a more regular and trust-based relationship with patients. The second is related to the return of thermolabile medicines. The HCC program obtained a higher RPN than PHA and COU (12 vs 2 vs 2) on this failure mode. Indeed, community pharmacists possess the required training regarding the ways to preserve the stability of drug and, under the COU program, medications are returned instantaneously in the same conditions as they were delivered, whereas returns under the HCC are processed by the health centers’ administrative staff without the supervision of a pharmacist.
Although RPN differences in the third and fourth critical steps were not considered significant, we believe that several aspects ought to be taken into consideration. As regards the third critical step, differences across programs lie in the higher likelihood of occurrence of modes of failure related to inappropriate medication storage conditions in the HCC program. This is because the PHA and COU programs avail themselves of pharmaceutical distributors and courier companies, respectively, which are able to transport refrigerated goods much more effectively than orderlies/drivers, even if the latter do make use of refrigerators and temperature-monitoring thermometers.
With respect to the fourth critical step, which corresponded to storage at the point of delivery, the main difference observed had to do with the likelihood that medications could suffer a loss of stability because of an excessively high/low storage temperature, and with the detectability of such a loss. In this regard, the PHA program had the lowest RPN given that community pharmacies are run by qualified pharmacists who carry out daily temperature checks and make use of refrigeration equipment. Although health centers also have standardized protocols aimed at minimizing any risks in their work processes, they often lack the automated continuous temperature monitoring equipment commonly used by community pharmacies, which contributes to increasing the likelihood and reducing the detectability of this failure mode in health centers. For their part, courier companies use intermediate distribution points where medicines are stored for a certain period of time before being delivered to the patient. These intermediate sites must meet a series of requirements, which are mandatorily included in the technical specifications of all tender processes for pharmaceutical transport services.
The economic analysis carried out as part of this study showed that the COU program was more costly to Andalusia's health system than HCC and PHA (€18,434.52 vs €11,417.08 and €7,986.52), which is probably attributable to the shipment rates used to calculate the cost of the COU program. In health areas with different geographic and demographic characteristics, lower shipment rates could be agreed with the courier company, which would reduce cost differences. Moreover, the cost of PHA was the lowest given the altruistic collaboration of community pharmacies and pharmaceutical distributors during the COVID-19 pandemic.
Lastly, our study presents with some limitations. With respect to FMEA, it must be pointed out that the identification of critical steps and modes of failure, as well as the determination of RPNs, were carried out subjectively by the evaluating team in the absence of any bibliographic references that could guide them as to how to best apply the FMEA methodology to home dispensing, health center dispensing and dispensing at a community pharmacy. As regards the economic evaluation, the limitations are related to the way the costs of the HCC and PHA programs were estimated. In the HCC program for example, the maintenance costs of the transport vehicle were not included as it had been acquired recently and no maintenance had as yet been necessary. Nor were the costs of storing the medicines in health centers included as the power, storeroom and cold-storage facility, and opportunity costs were part of the health center overheads, which made it possible to take advantage of existing economies of scale. Although the actual costs would probably come to a negligible amount, they should be included in future studies. In the PHA program, the cost of the pharmaceutical staff and the pharmaceutical distribution was zero given their altruistic collaboration during the COVID-19 pandemic.
The FMEA analysis applied to three medication dispensing programs (COU, HCC and PHA) awarded the lowest RPN score to the PHA program, followed by COU and HCC. Significant differences were observed in three of the six critical steps identified. These differences were due to aspects related to the exchange of information between patients and the HPD, where use of the electronic medical record played an important role. Moreover, the role of the community pharmacist was considered essential in terms of informed delivery, care, and custody of the medication at the community pharmacy, and of returns to the HPD. Participation of courier companies and pharmaceutical distributors was also key in ensuring proper preservation of the drugs during transportation.
A cost minimization analysis identified PHA as the least costly delivery program, followed by HCC and COU. However, it should be noted that the delivery and distribution costs in this case were estimated at zero given the altruistic collaboration of pharmacists and distributors during the COVID-19 pandemic. Lastly, it must be underscored that the economic differences obtained correspond to the Serrania de Malaga health area, characterized by a very specific demographic and geographic profile. Fresh economic studies should be undertaken for cases where there is no altruistic collaboration under the PHA program and/or the characteristics of the area under study are different from those of the Serrania de Malaga health area.
FundingNo funding.
AcknowledgementsWe would like to thank Sonia Hernández Valverde, from the Financial Management Unit of the Serranía de Málaga health care for performing a critical review of the manuscript and making important intellectual contributions, which were decisive for the approval of the final version submitted for publication.
Conflict of interestNo conflict of interests.
Contribution to the scientific literature
There being no studies evaluating the risks inherent in the dispensation and delivery of medicines by the outpatient care units of hospital pharmacies using the FMEA methodology, this work, which analyzes and compares the three most commonly-used medication delivery programs in the Spanish context, constitutes an original contribution. In addition, it includes an economic evaluation that may be replicated in other health areas of similar demographic and geographic characteristics to gain an appreciation of the economic burden that adopting each delivery program could entail for the public health system.