To evaluate rate and type of errors in inhalation technique of patients seen in hospitals at the observation area in the emergency department, as well as patients seen in the outpatients clinic at the primary care pharmaceutical consultation, and at the community pharmacy.
MethodDescriptive observational study carried out by a hospital pharmacist, along with a primary care pharmacist and a community pharmacist. An anonymous survey was performed in order to collect different analyzed data. Each patient was asked to execute a complete demonstration on how they used their inhalers, to actively check the inhalation technique. Two checklists regarding the type of inhaler were established in order to assess said technique. Results were tabulated through Microsoft Excel® 2010 software and analyzed through R 3.5 statistical program.
ResultsA total of 66 patients (42 male, 24 female; mean age 67) were recruited. Out of all patients, 48.5% used more than one inhaler, which 34.4% used different types of inhaler, and 65.6% used different systems. A total of 39 patients were under dry powder inhaler therapy, and 38 were using pressurized metered dose inhalers. The most frequent errors –both in dry powder inhalers and pressurized metered dose inhalers– were: not performing a 10 second apnea and not slowly expelling air from the lungs. Around 50% of patients needed new learning after assessing their inhalation technique, even though 88.5% had already received previous training. Older aged patients performed a worse inhalation technique.
ConclusionsThere is a high rate of errors in the use of inhaled therapy, being even higher among older aged patients. The inhalation technique training by the medical staff seems inadequate, as it is crucial to raise awareness about the importance of health education for patients and their use of inhalers, to which a scheduled follow up and a technical and feedback obtained from the patient assessment is required.
Analizar la tasa y los tipos de errores en la técnica de inhalación de pacientes atendidos a nivel hospitalario en el área de observación del servicio de urgencias y a nivel ambulatorio en la consulta farmacéutica de atención primaria y en la farmacia comunitaria.
MétodoEstudio observacional de tipo descriptivo realizado por un farmacéutico hospitalario en colaboración con un farmacéutico de atención primaria y un farmacéutico comunitario. Se realizó una entrevista anónima para registrar los distintos datos analizados y se solicitó a cada paciente que ejecutara una demostración completa de cómo utilizaba su inhalador habitualmente para comprobar de forma activa la técnica de inhalación. Para evaluar dicha técnica se establecieron dos checklist en función del tipo de inhalador. Los resultados fueron tabulados mediante el software Microsoft Excel® 2010 y analizados mediante el programa estadístico R 3.5.
ResultadosSe reclutaron 66 pacientes (42 varones y 24 mujeres; edad media 67 años). El 48,5% usaban más de un inhalador, de ellos el 34,4% utilizaban distintos tipos de inhalador y el 65,6% diferentes sistemas. Un total de 39 pacientes estaban en tratamiento con inhaladores de polvo seco y 38 con inhaladores de cartucho presurizado. Los errores más frecuentes, tanto con inhaladores de polvo seco como con inhaladores de cartucho presurizado, fueron: no realizar la apnea de 10 segundos y no expulsar lentamente el aire de los pulmones. En torno al 50% precisaron nuevo aprendizaje tras la evaluación de la técnica de inhalación, a pesar de que el 88,5% ya habían recibido formación previa. Los pacientes de edad más avanzada realizaban peor la técnica inhalatoria.
ConclusionesExiste una elevada tasa de errores en el empleo de la terapia inhalada, siendo mayor en los pacientes de edad más avanzada. La instrucción en la técnica inhalatoria por parte del personal sanitario parece inadecuada, por lo que es preciso sensibilizar al mismo sobre la importancia de la educación sanitaria a los pacientes en el empleo de los inhaladores, realizando un seguimiento programado y una evaluación de la técnica y del feedback obtenido por el paciente.
Respiratory system diseases, such as asthma and chronic obstructive pulmonary disease, are very common and have a high impact on our health, social and economic environment. According to the Spanish Society of Pneumology and Thoracic Surgery (SEPAR in its Spanish acronym), these diseases represent the first reason for medical consultation and the third leading cause of hospitalization and mortality in Spain1.
Inhalation is preferred for treating these diseases, as it has certain advantages over systemic therapies, such as fast access to the bronchial tree and a lower incidence rate of systemic side effects. Its main drawback is the difficulty that patients show in properly using inhalation devices, which may result in a lack of therapeutic efficacy and suboptimal control of the disease2,3.
In a recent systematic review, Sanchís et al.4, which includes studies published between 1975 and 2014 carried out among children and adults who received inhaled therapy, indicate that the misuse of inhalers is common, and has not improved in recent years. This fact points to an urgent need of new approaches to health education.
Aerosol Drug Management Improvement Team (ADMIT)5, conducted a literature review at a European level in 2006, from six European countries. The data obtained were similar to those offered in the systematic review of Sanchís et al.4.
There is currently an important variety of inhalation systems6 with different characteristics that hinders the knowledge of each, both for patients and healthcare professionals. That is of course a challenge for the pharmacists who work directly with patients in the different areas of healthcare.
The solution to the problem is complex and, among other measures that can be carried out, promoting and providing health education by professionals is critical.
A systematic review published in 2017, Klijn et al.7 analyzed the effectiveness of educational programs for inhalation technique (IT). It was noted that these programs (written brochures, verbal instruction, live demonstrations, videos…) are effective, as improvements in IT were reached by more than 90% of cases.
Considering the literature published to date, the aim of the study is to describe rate and most frequent error types in IT for patients under inhaler therapies in a population of similar characteristics of those in the province of Lugo (Galicia, Spain).
MethodsDescriptive, observational and cross-sectional study, conducted in Lugo between September and November 2018.
The study was conducted by a hospital pharmacist, along with a primary care pharmacist and a community pharmacist, who performed, each in their healthcare area, reconciliation of in-home medication, paying particular attention to inhaled therapy.
Patients who were treated with inhalers and who were admitted to the observation area of the Emergency Department at the University Hospital Lucus Augusti, as well as those who were treated at the primary care consultation and community pharmacy within the outpatients clinic, were included in the study.
An anonymous interview was conducted in order to collect demographic data: age, gender, about the inhalation devices –type of inhaler, inhalation system used, number of devices used and perception by the patient on the comfort of the technique– and IT data –whether they received previous training on inhaler's proper administration, and whether they needed or not new learning–.
Two types of inhaler were determined: pressurized metered dose inhalers (pMDI) and dry powder inhalers (DPI).
As for IT perception, the patient graded the technique's comfort from 1 to 10, where 1 was very simple and 10 very difficult.
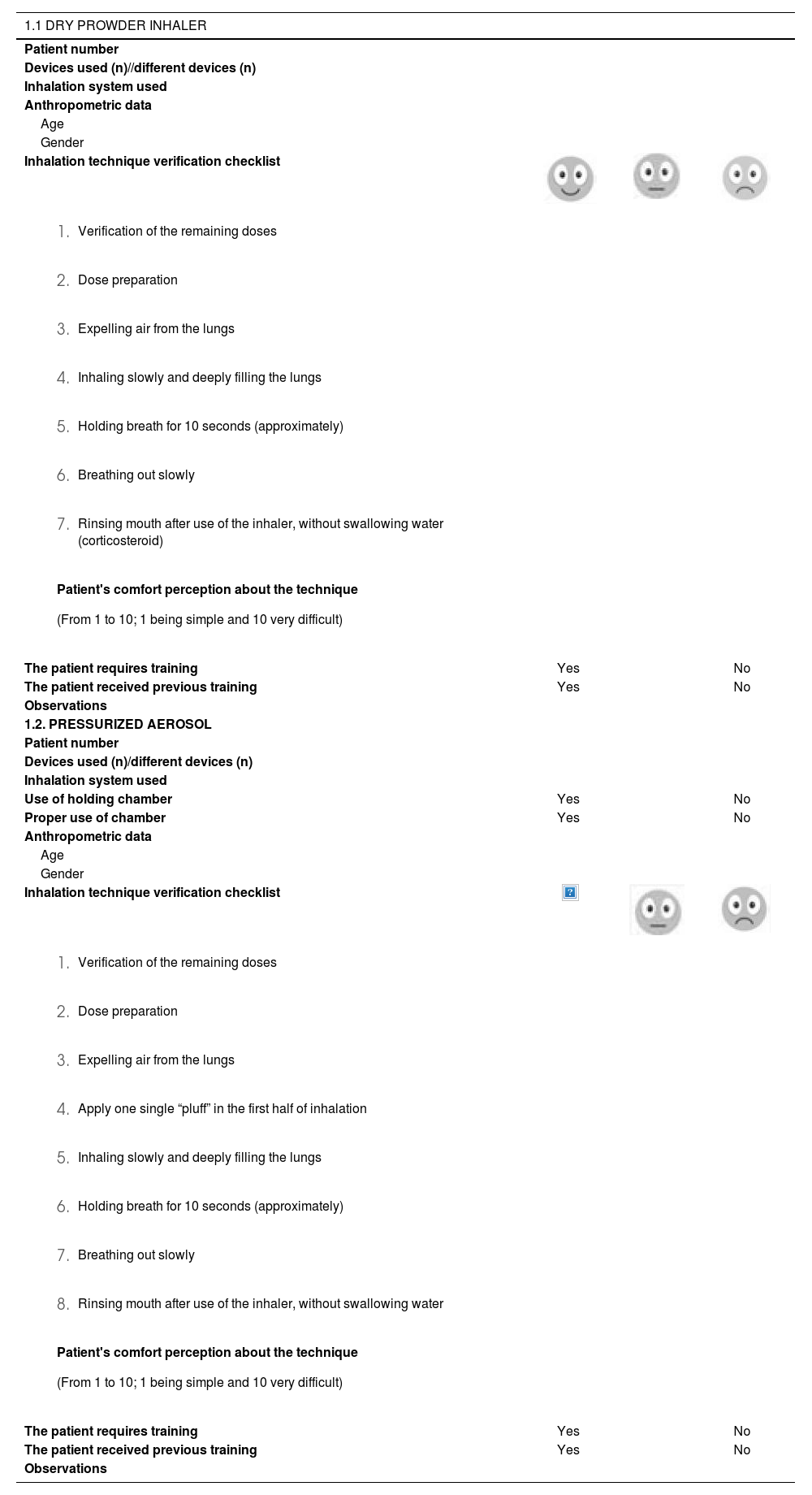
Without conferring any prior information, each patient was asked to execute a complete demonstration of how they used their inhaler regularly to actively check the IT. To evaluate the administration technique, two checklists regarding the type of inhaler were established. Those were modified following Melani8 A.’s protocol, as these steps slightly differ from the IT's protocol (Table 1). Each checklist item was graded as either good (2), average (1) or bad (0). Patients using more than one type of inhalation device followed the technique with each, and results were independently analyzed for every type of inhaler.
Survey on the correct use of dry powder inhaler (1.1) and pressurized metered dose inhalers (1.2)
| 1.1 DRY PROWDER INHALER | |||
|---|---|---|---|
| Patient number | |||
| Devices used (n)//different devices (n) | |||
| Inhalation system used | |||
| Anthropometric data | |||
| Age | |||
| Gender | |||
| Inhalation technique verification checklist | |||
| |||
| |||
| |||
| |||
| |||
| |||
| |||
| |||
| The patient requires training | Yes | No | |
| The patient received previous training | Yes | No | |
| Observations | |||
| 1.2. PRESSURIZED AEROSOL | |||
| Patient number | |||
| Devices used (n)/different devices (n) | |||
| Inhalation system used | |||
| Use of holding chamber | Yes | No | |
| Proper use of chamber | Yes | No | |
| Anthropometric data | |||
| Age | |||
| Gender | |||
| Inhalation technique verification checklist | |||
| |||
| |||
| |||
| |||
| |||
| |||
| |||
| |||
| |||
| The patient requires training | Yes | No | |
| The patient received previous training | Yes | No | |
| Observations | |||
For the analysis of obtained data, a descriptive statistics was performed. All parameters studied were continuous. For its analysis, the median and interquartile range were used. Bivariant comparisons were analyzed with the U Mann-Whitney test. To determine the correlation between variables, the Pearson test was used. Results were tabulated through Microsoft Excel® 2010 software and analyzed through R 3.5 statistical program.
ResultsA total of 66 patients were enrolled with a mean age of 67 years (16-94), being 24 women (36.4%) and 42 men (63.6%).
48.5% (32) of patients were treated with more than one inhaler, 34.4% (11) of these, used different types of inhaler, and 65.6% (21) used different inhalation systems.
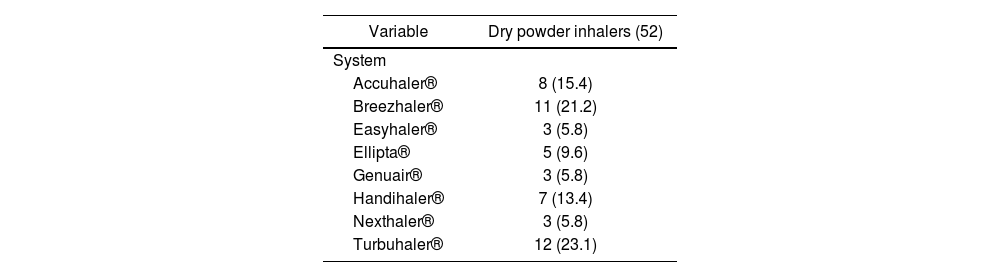
A total of 39 patients were treated with DPI and 38 with pMDI. The majority of DPI inhalation systems were Turbuhaler® (23.1%) and Breezhaler® (21.2%) (Table 2). To differentiate types of systems in pMDI has not been considered.
Among patients using DPI, 88.5% confirmed to have received prior training, and despite this, 44.2% needed new learning. In the case of patients using pMDI, these data were 42.5% and 57.5% respectively.
As for the perception of comfort by the patient regarding IT, it was similar for both inhalation devices, with a median of 3.5 (1.75 to 7) for DPI and 2 (1 to 5.2) for pMDI. Therefore, generally it was perceived as easy by the patient.
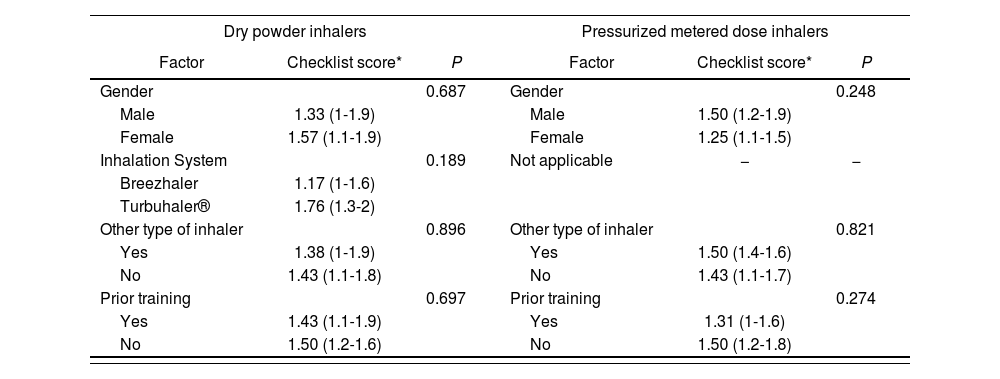
The IT's active assessment total score obtained from the checklist was 1.43 (1.1 to 1.9) for DPI, and 1.5 (1.1-1.7) for pMDI.
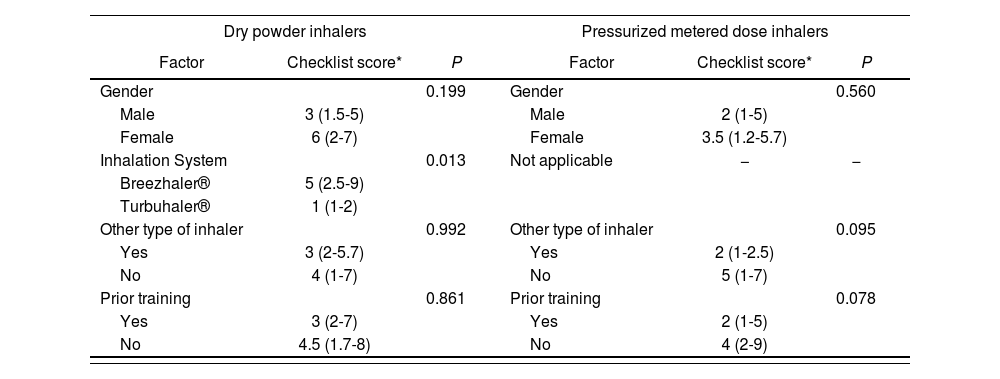
In order to detect possible connections between the studied variables, a bivariate statistical analysis study was carried out, regarding gender, inhalation system –considering only Turbuhaler® and Breezhaler® systems, and Breezhale® systems as they are the most common among DPI–, use of different types of inhalers, whether patients received prior training, total score and patient's perception. There were no statistically significant differences found (Tables 3 and 4).
Bivariate with regard to the score obtained from the checklist
| Dry powder inhalers | Pressurized metered dose inhalers | ||||
|---|---|---|---|---|---|
| Factor | Checklist score* | P | Factor | Checklist score* | P |
| Gender | 0.687 | Gender | 0.248 | ||
| Male | 1.33 (1-1.9) | Male | 1.50 (1.2-1.9) | ||
| Female | 1.57 (1.1-1.9) | Female | 1.25 (1.1-1.5) | ||
| Inhalation System | 0.189 | Not applicable | − | − | |
| Breezhaler | 1.17 (1-1.6) | ||||
| Turbuhaler® | 1.76 (1.3-2) | ||||
| Other type of inhaler | 0.896 | Other type of inhaler | 0.821 | ||
| Yes | 1.38 (1-1.9) | Yes | 1.50 (1.4-1.6) | ||
| No | 1.43 (1.1-1.8) | No | 1.43 (1.1-1.7) | ||
| Prior training | 0.697 | Prior training | 0.274 | ||
| Yes | 1.43 (1.1-1.9) | Yes | 1.31 (1-1.6) | ||
| No | 1.50 (1.2-1.6) | No | 1.50 (1.2-1.8) | ||
Bivariate with regard to the perception of IT by the patient
| Dry powder inhalers | Pressurized metered dose inhalers | ||||
|---|---|---|---|---|---|
| Factor | Checklist score* | P | Factor | Checklist score* | P |
| Gender | 0.199 | Gender | 0.560 | ||
| Male | 3 (1.5-5) | Male | 2 (1-5) | ||
| Female | 6 (2-7) | Female | 3.5 (1.2-5.7) | ||
| Inhalation System | 0.013 | Not applicable | − | − | |
| Breezhaler® | 5 (2.5-9) | ||||
| Turbuhaler® | 1 (1-2) | ||||
| Other type of inhaler | 0.992 | Other type of inhaler | 0.095 | ||
| Yes | 3 (2-5.7) | Yes | 2 (1-2.5) | ||
| No | 4 (1-7) | No | 5 (1-7) | ||
| Prior training | 0.861 | Prior training | 0.078 | ||
| Yes | 3 (2-7) | Yes | 2 (1-5) | ||
| No | 4.5 (1.7-8) | No | 4 (2-9) | ||
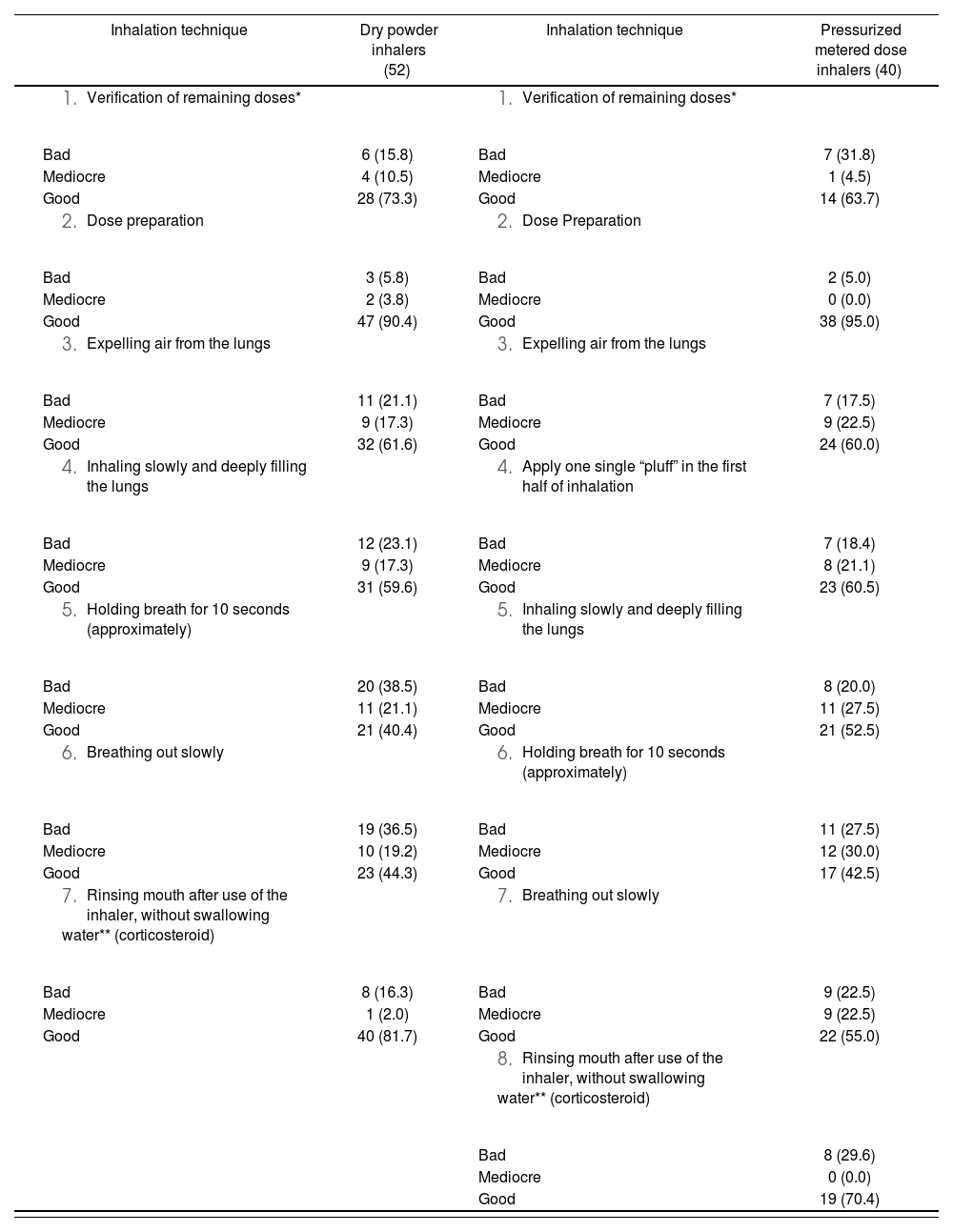
Regarding inhalation technique's active assessment, it should be noted that the most frequent errors found in both DPI and pMDI were not performing a 10 second apnea and not slowly expelling air from the lungs, asTable 1. Survey on the correct use of dry powder inhaler (1.1) and pressurized metered dose inhalers (1.2) well as not adequately inhaling in order to facilitate access for the medicine to the lungs (Table 5).
Frequency and error rate in the inhalation technique.
| Inhalation technique | Dry powder inhalers (52) | Inhalation technique | Pressurized metered dose inhalers (40) |
|---|---|---|---|
|
| ||
| Bad | 6 (15.8) | Bad | 7 (31.8) |
| Mediocre | 4 (10.5) | Mediocre | 1 (4.5) |
| Good | 28 (73.3) | Good | 14 (63.7) |
|
| ||
| Bad | 3 (5.8) | Bad | 2 (5.0) |
| Mediocre | 2 (3.8) | Mediocre | 0 (0.0) |
| Good | 47 (90.4) | Good | 38 (95.0) |
|
| ||
| Bad | 11 (21.1) | Bad | 7 (17.5) |
| Mediocre | 9 (17.3) | Mediocre | 9 (22.5) |
| Good | 32 (61.6) | Good | 24 (60.0) |
|
| ||
| Bad | 12 (23.1) | Bad | 7 (18.4) |
| Mediocre | 9 (17.3) | Mediocre | 8 (21.1) |
| Good | 31 (59.6) | Good | 23 (60.5) |
|
| ||
| Bad | 20 (38.5) | Bad | 8 (20.0) |
| Mediocre | 11 (21.1) | Mediocre | 11 (27.5) |
| Good | 21 (40.4) | Good | 21 (52.5) |
|
| ||
| Bad | 19 (36.5) | Bad | 11 (27.5) |
| Mediocre | 10 (19.2) | Mediocre | 12 (30.0) |
| Good | 23 (44.3) | Good | 17 (42.5) |
|
| ||
| Bad | 8 (16.3) | Bad | 9 (22.5) |
| Mediocre | 1 (2.0) | Mediocre | 9 (22.5) |
| Good | 40 (81.7) | Good | 22 (55.0) |
| |||
| Bad | 8 (29.6) | ||
| Mediocre | 0 (0.0) | ||
| Good | 19 (70.4) |
Considering both the total score assigned in implementing the IT and the patient's perception, the correlation between these variables and age were examined. It was concluded that there is a statistically significant negative correlation (p < 0.001) between the patient's IT perception, the total IT score, and age. Therefore, patients within an older aged range perform a worse IT. Moreover, the comfort perception about its technique for these patients seem to be more difficult.
DiscussionThe results of the study correspond to those observed in other studies, where a high percentage of technical failures in the use of inhalers by patients4,9,10 was also found. This fact shows that these errors in the use of inhalers exist, despite having received prior training.
An erroneous IT contributes to poor control of symptoms, and is related to an increase of the need for rescue therapy, a greater use of emergency care services, and a deterioration of disease control. As a result, the economic cost related to the disease would increase along with the risk of suffering side effects, and the effectiveness of the therapy would be reduced.
It is observed that IT is performed worse by older aged patients, who in turn are aware of their limitations to do so, and they classify it as a difficult technique. This age-related difficulty was also observed in Van Beerendonk et al.’s study11.
Thus, these patients should be a priority when composing a more detailed training and a more thorough follow up. Note that the population between 20 and 40 years old is not represented in this sample.
Therefore, it would require further studies that include patients in this age range. The study underlines that among the most frequent errors observed include not performing a 10 second apnea and not slowly expelling air from the lungs. Interestingly, these errors are not directly linked with the device, as it exclusively depends on the patient's knowledge on the technique.
Therefore, regular education through active IT checking plays an irreplaceable role in health care for patients undergoing inhaler treatment. Written instructions are not enough for improving inhalation technique. They require complementary reinforced interventions where the scheduled follow up of this technique, as well as the obtained patient's assessment feedback is a priority, allowing amendments of the observed failures.
In this study's case, training was provided for almost 50% of patients, but the design of this study does not allow an analysis on the influence that said training could have had. Other authors have shown that interventions of any health professional improve both the use of inhalers and the diseases control for which they are used12–14.
It has been observed that 16.7% of patients combine DPI with pMDI, whose different techniques of use could lead to an increase of errors among patients. Hence, another key point to improve the use of inhalers is to ensure that the device used is the most suitable for the patient.
In conclusion, this study shows a high rate of errors in the use of inhaled medication among patients. The training offered by healthcare professionals seems inappropriately low, which requires raising awareness among professionals about the importance of this matter.
FundingNo funding.
AcknowledgementMaría Agustina Fernández Pérez, Primary Care Pharmacist, Villalba. Isabel Coira Nieto, Community Pharmacy pharmacist, Lugo. Spain.
Conflict of interestsNo conflict of interest.
Contribution to the scientific literatureInhalation therapy has evolved over the past few years, and it is essential to examine whether device improvements are also comfortable for the patient, as well as whether efficacy is reached.
The study shows a high percentage of errors in inhalation technique. This information is considerably relevant in order to examine and improve pharmaceutical care for these patients.