To design a homogeneous methodology for the registration and analysis of pharmaceutical interventions performed in spanish intensive adults care units (ICUs).
MethodObservational, prospective, and multicentre study.
In the first stage, a national registry of pharmaceutical interventions will be agreed upon and subsequently, all the pharmaceutical interventions performed on adult patients admitted to Spanish ICUs during 8 weeks will be recorded. Variables related to the type of ICU, the drug involved in the intervention, type of intervention (indication, effectiveness, safety), recommendation made by the pharmacist, and the degree of acceptance will be evaluated. Risk and incidence will be calculated for each of the medication errors detected. The χ2-squared test or Fisher exact test will be used for categorical variables and Mann–Whitney U or Kruskal–Wallis test for continuous variables. All tests will be performed with a significance level α=0.05 and confidence intervals with confidence 1-α.
DiscussionThe results obtained from this project will make it possible to obtain a homogeneous classification of the pharmaceutical interventions performed in ICUs, a national registry record, and an evaluation of the weak points with the aim of developing strategies for improvement in the pharmaceutical care of the critically ill patient.
diseñar una metodología homogénea para el registro y análisis de intervenciones farmacéuticas realizadas en unidades de cuidados críticos de adultos españolas.
Metodologíaestudio observacional, prospectivo y de carácter multicéntrico. En una primera etapa se consensuará un registro nacional de intervenciones farmacéuticas y posteriormente se registrarán las intervenciones farmacéuticas realizadas sobre pacientes adultos ingresados en UCC españolas durante ocho semanas. Se evaluarán variables relacionadas con el tipo de UCC, el fármaco implicado en la intervención, tipo de intervención (indicación, efectividad, seguridad) y recomendación realizada por el farmacéutico, así como el grado de aceptación. Se calculará el riesgo y la tasa de incidencia para cada uno de los errores de medicación detectados. Se empleará el test χ2-cuadrado o test exacto de Fisher para variables categóricas y U de Mann–Whitney o test de Kruskal-Wallis para variables continuas de acuerdo a la normalidad. Todos los test se realizarán con un nivel de significación α = 0.05 y los intervalos de confianza con una confianza 1- α.
Discusiónlos resultados del proyecto permitirán obtener una clasificación homogénea de las intervenciones farmacéuticas realizadas en UCC, un registro nacional y una evaluación de los puntos débiles con el objetivo de desarrollar estrategias de mejora en la atención farmacéutica del paciente crítico.
Patients admitted to intensive critical care units (ICUs) are at a high risk of medication errors (MEs) due to the severity of their condition and the numerous interventions they undergo during monitoring and treatment. This population is more vulnerable to MEs or medication-related problems due to pharmacokinetic-pharmacodynamic changes caused by ongoing pathophysiological changes (altered volume of distribution, organ dysfunction), as well as medication-related factors (polymedication, frequent use of high-risk drugs, and parenteral drugs).1,2
Multicentre studies conducted in various countries have investigated adverse event (AE) rates in hospitals and reported rates ranging from 4% to 17%.3 MEs were one of the most common types of AE. In Spain, the National Study of Adverse Events found that 10% of patients treated in hospitals experience an AE. Medications were the most common cause of AEs (37.4%), while 34.8% of these AEs were preventable.4
In addition, a Spanish multicentre study (SYREC) investigated AEs in 79 ICUs. The study included 1017 patients, finding that 591 experienced at least 1 incident (58%). The overall risk of an ME per ICU admission was 22%, with a rate of 1.13 ME per 100 patients/day. The majority of MEs occurred during the prescription (34%) and administration (28%) stages. Furthermore, 16% of these MEs caused harm to the patient, while 82% were classified as “certainly unavoidable”.5
ME management focuses on prevention. Measures are designed to reduce the likelihood of errors, detect them before they reach the patient or minimise the severity of consequences. Various interventions have been shown to reduce the rate of MEs. One such intervention is the inclusion of clinical pharmacists in ICUs to manage drug-related AEs, improve processes to reduce and/or prevent them, and report any that do occur.6
In 2001, an AE notification system—the ICU Incident Safety Reporting System—was developed by the Society of Critical Care Medicine, the Australian Patient Safety Foundation, and the Agency for Healthcare Research and Quality. The system included 23 adult and paediatric ICUs and reported 2075 events in 24 months. Of these, 42% resulted in harm and 0.8% contributed to patient death. The AEs were mainly related to medication, care, and equipment. Harmful AEs were most frequently associated with catheters, tubes, and drains, as well as other medical equipment or devices. Staff training and teamwork were also identified as contributing factors. Two or more contributing factors were involved in 42% of AEs, with a greater number of factors associated with a higher risk of failure.7
Despite the importance of having a common ME registry, 95.4% of hospitals in Spain use their own ME notification registry or independent regional platforms. Only 66.7% of these registries allow for consultation and follow-up by the notifier or safety managers.8 Most registries (46.4%) are internal registries maintained by individual hospitals. There is currently no unified methodology for evaluating and recording pharmaceutical interventions (PIs) in ICUs.8,9 Furthermore, some hospitals still use paper prescriptions, and even those that have clinical history or electronic prescription software rarely have systems capable of recording, classifying, and analysing PIs to improve the pharmacotherapeutic process.9 The aim of the FARMACRITIC study is to create a unified registry to record, classify, and analyse the PIs conducted by hospital pharmacists (HPs) in ICUs. This registry will help to determine strategies to enable the safer use of medicines in these units.
MethodologyDesignObservational, prospective, and multicentre study.
ObjectivesThe main objective is to reach a consensus on a methodology for the registration of PIs performed in Spanish ICUs.
The secondary objectives are to analyse the PIs conducted by clinical pharmacists in Spanish ICUs, evaluate and classify these PIs according to the scientific evidence provided by clinical practice guidelines for critically ill patients, and identify the highest-risk points in the pharmacotherapeutic process to focus strategies and promote the rational and safe use of medicines in ICUs.
EnvironmentSpanish hospital pharmacy services in which pharmacists conduct pharmacotherapeutic reviews and validations of critically ill adult patients admitted to ICUs.
Study periodA timeframe of 8 weeks will commence following approval by the participating centres. The PIs performed in this period will be analysed within 10 days of the intervention.
Inclusion criteriaICUs that provide care for critically ill adults and have a clinical pharmacist specialised in pharmaceutical care for such patients who voluntarily agrees to participate in the study.
Exclusion criteriaPaediatric and neonatal ICUs, as well as hospitals that do not have a pharmacist available to review the patient's treatment during their admission to the ICU.
Variables- −
Variables of interest by hospital: adapted from the map of the current situation of pharmacists in Spanish ICUs9:
- •
(1) Description of the hospital and ICU; (2) hospital characteristics (primary, secondary, or tertiary); (3) number of hospital beds (less than 200, between 201 and 500, between 501 and 1000, more than 1000 beds); (4) type of ICU (general, medical, surgical, coronary, neurocritical, trauma, burns, other); (5) number of ICU beds; (6) pharmacists per ICU; (7) pharmacists' years of experience in ICUs; (8) assistance in patient rounds; (9) participation (full or part-time); (10) tasks performed (clinical pharmacokinetics, artificial nutrition, antimicrobial optimisation programme [PROA], safety and pharmacovigilance, pharmacotherapy); and (11) tasks performed in pharmacotherapy (pharmacotherapeutic validation and follow-up, conciliation, participation in therapeutic protocols, teaching, research, innovation activities, drug monitoring, etc).
- −
PIs:
- •
Firstly, the PIs to be included in the analysis were defined according to the study by Domingo-Chiva et al.10 and the third Granada consensus.11 Secondly, each type of PI was subsequently evaluated, and a consensus classification of actions relevant to ICUs was developed by the members of the Working Group on Pharmaceutical Care of Critically Ill Patients (FARMIC) of the Spanish Society of Hospital Pharmacy, using a Microsoft Forms survey. The resulting classification was reviewed and externally validated by intensivists experienced in quality and safety processes for critically ill patients.
- −
Variables related to pharmacist activity:
- •
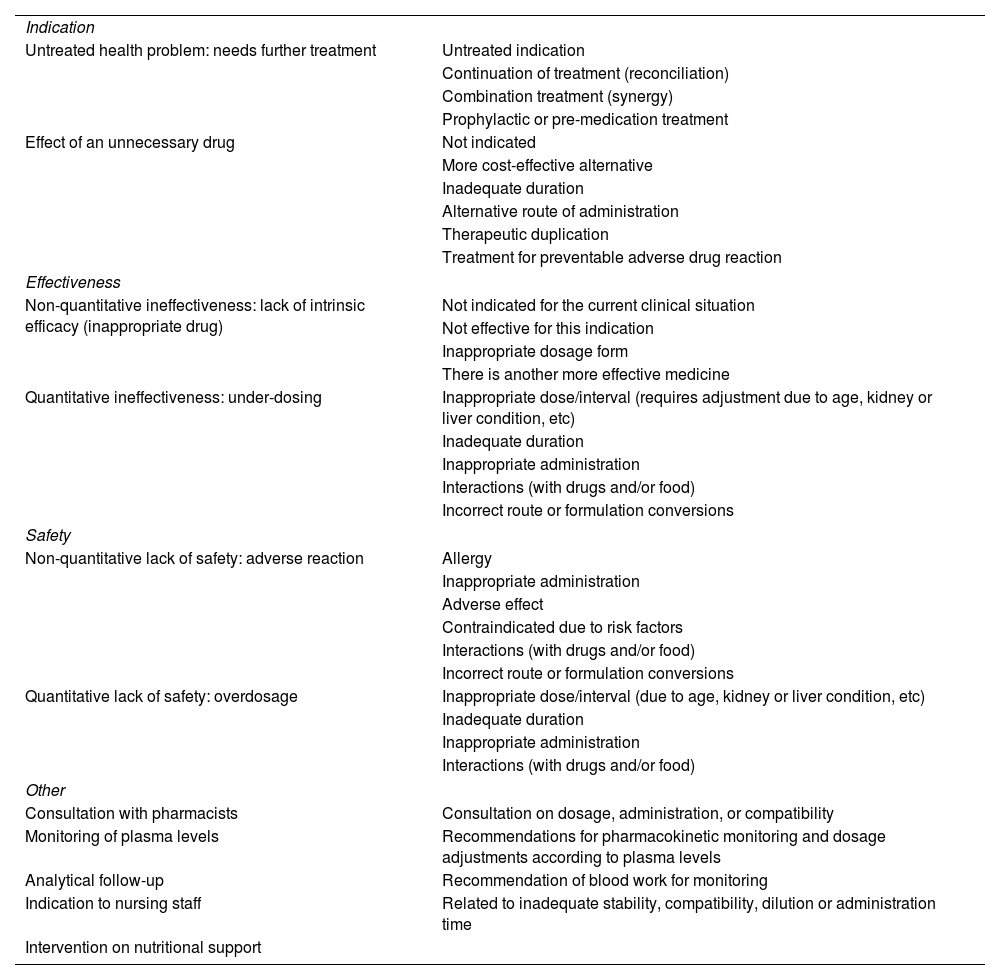
PI: a qualitative polytomous variable defined as a recommendation made by pharmacists to the physician or nurse responsible for each patient. The type of intervention (proactive or reactive) will be recorded. Reasons for intervention are defined as situations that may prompt pharmacists to issue a recommendation when they detect deviations from clinical practice in prescribing, drug administration, and/or transcription errors. The interventions were classified based on the incidents that prompted the pharmacists' actions (Table 1).
Table 1.Classification of pharmaceutical interventions.
Indication Untreated health problem: needs further treatment Untreated indication Continuation of treatment (reconciliation) Combination treatment (synergy) Prophylactic or pre-medication treatment Effect of an unnecessary drug Not indicated More cost-effective alternative Inadequate duration Alternative route of administration Therapeutic duplication Treatment for preventable adverse drug reaction Effectiveness Non-quantitative ineffectiveness: lack of intrinsic efficacy (inappropriate drug) Not indicated for the current clinical situation Not effective for this indication Inappropriate dosage form There is another more effective medicine Quantitative ineffectiveness: under-dosing Inappropriate dose/interval (requires adjustment due to age, kidney or liver condition, etc) Inadequate duration Inappropriate administration Interactions (with drugs and/or food) Incorrect route or formulation conversions Safety Non-quantitative lack of safety: adverse reaction Allergy Inappropriate administration Adverse effect Contraindicated due to risk factors Interactions (with drugs and/or food) Incorrect route or formulation conversions Quantitative lack of safety: overdosage Inappropriate dose/interval (due to age, kidney or liver condition, etc) Inadequate duration Inappropriate administration Interactions (with drugs and/or food) Other Consultation with pharmacists Consultation on dosage, administration, or compatibility Monitoring of plasma levels Recommendations for pharmacokinetic monitoring and dosage adjustments according to plasma levels Analytical follow-up Recommendation of blood work for monitoring Indication to nursing staff Related to inadequate stability, compatibility, dilution or administration time Intervention on nutritional support - •
Medication involved in the PI: a qualitative polytomous variable. The active ingredient will be recorded. It will include both drugs listed in each hospital's pharmacotherapeutic guide and those not listed. It will also include the ATC classification for each drug, as described by the Nordic Council in collaboration with the World Health Organisation.12 High-risk medicines will be recorded according to the Institute for Safe Medication Practices.13
- •
Acceptance of PI: a qualitative dichotomous variable. The pharmacists' recommendations may be accepted/rejected by the prescribing physician or responsible nurse within 24 h of the recommendation.
- •
Method of communication: a trichotomous qualitative variable showing how pharmacists communicated their recommendations: in person during patient visits, by telephone, or by registering a note in the patient's medical record.
- •
Target of the intervention: a qualitative dichotomous variable (doctor/nurse). Communication of the problem to the medical or nursing team based on the type of PI.
- •
Clinical evaluation of accepted PIs: an ordinal categorical variable evaluating the influence and added value of the intervention in terms of potential efficiency. Of note, the impact of the intervention can only be measured if the intervention is accepted. If it is not accepted, it cannot be measured.
- •
Pharmaceutical care: coronary patients, neurocritical patients, sepsis/septic shock, sedoanalgesia/delirium, fluid therapy/electrolyte disturbance management, blood products, gastrointestinal disturbances or enteral/parenteral nutrition, solid organ transplantation or haematopoietic transplantation, extracorporeal support therapies (mechanical ventilation, continuous renal replacement techniques, extracorporeal membrane oxygenation system), training/health education aimed at medical staff (meetings, literature review), nursing staff, auxiliary staff, patients, and/or relatives.
Once the structure and methodology of the registry are defined, HPs working in ICUs will be invited to participate voluntarily via the mailing list of the Spanish Society of Hospital Pharmacy (SEFH).
Data sourcesParticipating clinical pharmacists will review the clinical histories and prescriptions of patients admitted to ICUs.
Data collectionA data collection notebook will record the variables using the Research Electronic Data Capture platform. Each research member will be able to log in using a password and record their PIs. The data will be anonymised prior to entry. A data collection protocol will be distributed to researchers and collaborators. For quality control purposes, PIs will be reviewed by the lead investigator, and any discrepancies will be evaluated by consensus among the main investigators of the project.
Patient safetyIf an investigator detects a suspected adverse reaction related to any drug, he/she shall notify the Regional Centre for Pharmacovigilance using the yellow card (www.notificaRAM.es), and may also notify the marketing authorisation holder of the drug under suspicion in parallel.
Sample sizeThe final sample size will depend on the number of participating hospitals. Clinical pharmacists who are members of the FARMIC group will be asked to confirm their voluntary participation in writing. We estimate that from 40 to 45 pharmacy services will participate.
Statistical methodsAll statistical analyses will be performed using STATA v. 14.1. The statistical analysis plan will describe all statistical tests to be used for analysing the collected data based on the study's stated aims. Any deviations from the original statistical plan will be described and justified in the final results report. The median and interquartile range will be calculated for continuous variables and relative and absolute frequencies for discrete variables. Risk (cumulative incidence) and rate (incidence density) will be calculated for each of the MEs and PIs. For research variables, the chi-squared test or Fisher's exact test will be used for categorical variables, while the Mann–Whitney U or Kruskal–Wallis test will be used for continuous variables, depending on the normality of the data. All tests will be conducted at a significance level of α=0.05, with confidence intervals corresponding to a confidence level of 1α.
DiscussionThis project will create a homogeneous PIs registry methodology adapted to the critical care setting, enabling consensus-based evaluation and classification. It will help identify intervention-prone areas and support the development of strategies to improve the pharmacotherapeutic process and reduce budgetary strain. It will also provide health education for both patients and professionals, ultimately promoting the rational and safe use of medicines in ICUs.
The integration of HPs into multidisciplinary care teams has been shown to significantly reduce the incidence of AEs due to MEs, thereby reducing healthcare costs.10,14,15 The clinical impact of HPs increases significantly if PIs are performed proactively at the time of prescription, resulting in greater efficacy and efficiency while reducing MEs.10 A 42-month prospective descriptive study evaluated the integration of HPs into a multidisciplinary team in a Spanish ICU. A total of 2399 PIs were performed with a 97% acceptance rate. The PIs were primarily related to dosage (36.8%) and pharmacist consultations (25.7%). Of the accepted PIs, 53.7% influenced the efficacy of the drug treatment, 35.1% affected tolerance, and 10.2% impacted costs alone.10 Bearing this in mind, we propose creating a homogeneous and standardised working methodology designed by HPs working in ICUs. One of the strengths of this study is the use of a standardised methodology and the evaluation of validation adequacy. This approach aims to improve the pharmacotherapeutic process, generate economic savings, and optimise health outcomes. Each of these factors supports the demand for more specialists and the expansion of pharmacy services.
The main limitations of the study arise from the lack of a systematic classification of PIs for ICU patients, along with the challenges of adapting PIs to different types of patients and ICUs, and the varying methodologies used in each hospital. These challenges will be addressed by having FARMIC members determine PIs in the initial stage, followed by a consensus process and the publication of a standardised national classification. This classification will then be externally validated by intensivist physicians. On the other hand, as this is an anonymous, voluntary reporting study, there may be underreporting of MEs due to a lack of knowledge or awareness of their occurrence, or fear of repercussions. However, with the involvement of national pharmacy services and the validation of the records by the coordinating group, we expect to obtain a representative sample of the overall situation of ICUs across Spain.
In conclusion, the results of this project will enable us to analyse a unified registry and classify the PIs performed by pharmacists in ICUs. Additionally, it will facilitate the establishment of a consensus on a standardised methodology to optimise the pharmacotherapy of critically ill patients.
Ethical responsibilitiesThe study was evaluated and approved as a prospective observational study involving medications by the Medicines Research Ethics Committee (CEIM) of the Hospital Universitari i Politècnic La Fe on 25 October 2023 (promoter code FARMACRITIC). All collaborating researchers signed an agreement to adhere to the Standards of Good Clinical Practice and the Declaration of Helsinki. A waiver of informed consent was approved due to the observational nature of this non-interventional study. The confidentiality and anonymity of the patients, staff, and participating ICUs will be guaranteed at all times, in compliance with Organic Law 3/2018, of 5 December, on the Protection of Personal Data and Guarantee of Digital Rights. Since the results of the study will not be binding for professionals or patients directly, we are committed to publishing both positive and negative results.
FundingThis study was funded by the Fundación Española de Farmacia Hospitalaria (FEFH) via the 2022–2023 Call for Grants for Working Groups.
Declaration of authorshipAll authors are members of the FARMIC Working Group. All authors participated in the study design and reached a final consensus on the interventions under analysis. María Martín-Cerezuela, Esther Domingo-Chiva, and Fernando Becerril-Moreno were responsible for writing the manuscript. All authors reviewed and approved the final version of the manuscript for publication.
CRediT authorship contribution statementMaría Martín Cerezuela: Writing – review & editing, Writing – original draft, Validation, Project administration, Methodology, Investigation, Data curation, Conceptualization. Fernando Becerril Moreno: Writing – review & editing, Writing – original draft, Resources. Miguel Ángel Amor García: Investigation, Conceptualization. Carla Bastida Fernández: Investigation. Irene Aquerreta González: Investigation. Sara Cobo Sacristán: Investigation. Amaia Egüés Lugea: Investigation. Marta Albanell Fernández: Investigation. Laura Doménech Moral: Investigation. Aurora Fernández Polo: Investigation. Tatiana Betancor García: Investigation. Sara Ortiz Pérez: Investigation. Esther Domingo Chiva: Writing – review & editing, Writing – original draft, Project administration, Methodology, Investigation, Conceptualization.
None declared.