To determine persistence of treatment with secukinumab across its different indications.
MethodThis is a retrospective descriptive observational study including adult patients treated with secukinumab in its different indications from the drug's introduction in November 2015 to October 2019. The variables included were sex; age; diagnosis; initiation date; line of treatment; number of patients who discontinued treatment and reason for discontinuation; overall persistence at 12 months; distribution of patients; and persistence according to indication, line of treatment and reason for suspension.
ResultsOne-hundred forty-three patients were started on secukinumab, but only patients who had been in treatment at least 12 months before the end of the study were included. Mean patient age was 49.8 years (±12.6); 52.9% were men. Fifty-six patients (53.8%) had discontinued treatment by the end of the study, with a mean duration of treatment of 12.7 months (±10.2). The other patients (n = 48) continued with their therapy. Mean duration of treatment in these patients was 25.7 months (±9.9). Overall persistence at 12 months was 10.0 months (±3.3) with a discontinuation rate at 12 months of 31.7%. Persistence at 12 months was 10.7 months (±2.9) for patients with psoriasis, 9.7 months (±3.4) for patients with psoriatic arthritis, and 8.8 months (±3.8) for those with ankylosing spondylitis. Of the 48 patients who continued with their treatment after completion of the study, 22 (45.8%) received the drug as first-line treatment. Of the 56 discontinuations, 15 (26.8%) were due to primary failure (persistence: 3.8 months [±1.1]) and 27 (48.2%) were due to secondary failure (persistence: 18.6 months [±9.6]). Persistence in patients who continued treatment was higher in psoriasis (28.8 months [±10.3]). In those who discontinued due to secondary failure it was higher in the group with ankylosing spondylitis (28.0 months [±4.2]). Persistence among patients on first-line secukinumab was higher than for other patients: 21.2 months (±7.2) if they stayed on treatment, 3.5 months (±0.5) if they presented with primary treatment failure, and 8.3 months (±2.5) in those with secondary treatment failure.
ConclusionsOur data show slightly higher persistence levels in patients with psoriasis and lower discontinuation rates in those without previous exposure to biological therapy. Long-term studies are needed to confirm these findings and to gain a better understanding of the factors that can influence persistence of secukinumab.
Determinar la persistencia del tratamiento con secukinumab en sus diferentes indicaciones.
MétodoEstudio descriptivo, observacional, retrospectivo donde se incluyeron los pacientes adultos tratados con secukinumab en sus diferentes indicaciones desde su comercialización en noviembre de 2015 hasta octubre de 2019. Las variables recogidas fueron sexo, edad, diagnóstico, fecha de inicio, línea de tratamiento, número de pacientes que habían suspendido el tratamiento y motivo de suspensión, persistencia global a los 12 meses, distribución de pacientes y persistencia según indicación, línea de tratamiento y motivo de suspensión.
ResultadosHan sido tratados con secukinumab 143 pacientes, de los que 104 llevaban en tratamiento 12 o más meses. La media de edad fue 49,8 ± 12,6 años; 52,9% fueron hombres. Suspendieron el tratamiento 56 pacientes (53,8%) con una media de duración del mismo de 12,7 ± 10,2 meses. El resto (n = 48) continuaban con una media de duración de 25,7 ± 9,9 meses en el momento del corte del estudio. La persistencia global a los 12 meses fue de 10,0 ± 3,3 meses con una tasa de discontinuación a los 12 meses del 31,7%. La persistencia por patología a los 12 meses fue 10,7 ± 2,9 para los pacientes con psoriasis, 9,7 ± 3,4 meses para los pacientes con artritis psoriásica y 8,8 ± 3,8 para los pacientes con espondilitis anquilosante. De los 48 pacientes que continuaban en tratamiento, 22 (45,8%) están recibiendo el fármaco en primera línea. De los 56 pacientes que discontinuaron, 15 (26,8%) lo hicieron por fallo primario (persistencia 3,8 ± 1,1 meses) y 27 (48,2%) por fallo secundario (persistencia 18,6 ± 9,6 meses). La persistencia en los pacientes que continuaban en tratamiento fue superior en psoriasis (28,8 ± 10,3 meses) y en los que suspendieron por fallo secundario fue superior en espondilitis anquilosante (28,0 ± 4,2 meses). En los pacientes de primera línea, la persistencia fue inferior al resto, siendo 21,2 ± 7,2 meses, 3,5 ± 0,5 meses y 8,3 ± 2,5 meses, si continuaban en tratamiento, presentaron fallo primario o fallo secundario, respectivamente.
ConclusionesNuestros datos muestran una persistencia ligeramente superior en pacientes con psoriasis y una menor tasa de discontinuación en aquellos pacientes sin exposición previa a un tratamiento biológico. Se necesitan estudios a largo plazo que lo confirmen y conocer los factores que pueden influir en la persistencia del secukinumab.
Adherence to medication is the process by which patients take their medication as prescribed by a healthcare provider1. Lack of adherence affects the effectiveness of treatment and may result in an upward dose adjustment or in switching patients to more aggressive treatments, which could represent higher drug-related risks and increased costs2. It is estimated that half of chronic patients in Spain do not adhere to the treatments prescribed to them, which tends to lead to poorer disease control and increased complications3.
When applied to biological therapies, adherence is associated with a great variety of methods and definitions. Most studies measure adherence in terms of the medication possession ratio4,5, although other methods have been described such as proportion of days covered, or infusions missed over a given period. Some authors have even resorted to qualitative methods. This plethora of different methods has resulted in a huge variability of adherence rates across different studies6–9.
In the last few years, the term persistence has come to be used as a complement to the concept of adherence. Therapeutic persistence is defined as the time elapsed from initiation of treatment to long-term or definitive discontinuation10, i.e. the time during which a given drug is considered a valid option for a given patient. It is a concept related to both the effectiveness and the safety of the drug, as well as to the patient's satisfaction with it. It could therefore be said that it reflects the patient's real-life attitude to their treatment, constituting a useful tool to measure the success of such treatment.
According to the Therapeutic Adherence Group of the Spanish Society of Hospital Pharmacists, the persistence of biological agents is defined as the number of days during which uninterrupted treatment is administered, generally calculated using dispensation databases. Such administration periods may allow for certain treatment-free breaks (treatment gaps) which, according to different studies, tend to range from 30 to 90 days, and may require 2, 6 or 12-month-long intervals of uninterrupted admi-nistration2.
As a result of the foregoing, an analysis of persistence should take into consideration whether discontinuations correspond to actual cessations of treatment, generally resulting from remission; lack of efficacy, adverse events; or breaks in treatment promoted by pregnancy or a wish to become pregnant, remission, the patient's wishes, mild infection, or a surgical procedure. It is essential to analyze the reasons for discontinuation to avoid erroneous interpretations of the data.
Lastly, it should not be forgotten that persistence has a favorable impact on the cost of treatment, the importance of which cannot be overstated when it comes to selecting a biological therapy.
Secukinumab is a monoclonal antibody that selectively binds to and neutralizes interleukin 17A (IL-17), inhibiting its interaction with the IL-17 receptor. As a result, secukinumab prevents the release of proinflammatory cytokines, chemokines and the tissue damage mediators that participate in the development of autoimmune or inflammatory disease. It is indicated in cases of plaque psoriasis, psoriatic arthritis, and ankylosing spondylitis11. During the maintenance phase, it is administered monthly which makes it a very convenient drug from the patient's point of view. However, as it has been on the market for a relatively short period of time, there are still few reports on its persistence.
The purpose of this study is to determine the persistence of treatment with secukinumab across its different indications in a third-level hospital.
MethodsA retrospective descriptive observational study was conducted between November 2015 and October 2019 to analyze adult patients treated with secukinumab in its different indications since the drug was first introduced. Only patients who had started treatment at least 12 months before the end of the study were included.
Variables analyzed included sex, age, diagnosis, date of initiation, line of treatment, number of patients who discontinued treatment and reason for discontinuation (primary failure, secondary failure, therapeutic window, intolerance, poor adherence, death for other reasons, loss to follow up and others), overall persistence at 12 months (defined as months of uninterrupted treatment), patient distribution, and persistence per indication.
Persistence was calculated based on dispensations of the drug from the hospital's Pharmacy Department. We also took into consideration the date of the latest dispensation and the patients’ medical data to determine the date of treatment discontinuation. Delays in dispensing medications of up to 30 days were regarded as transient discontinuations.
To analyze persistence per indication and per line of treatment we considered patients who continued with their treatment as well as primary and secondary failures. This allowed us to determine how many patients responded and for how long.
The data were obtained from Savac®, the Pharmacy Department's dispensing management system, and the patients’ electronic medical record (Selene®).
The statistical analysis was carried out using the SPSS Statistics® software package v23. Continuous variables were expressed as means or medians ± standard deviation (interquartile range). Categorical variables were expressed as percentages.
The study was approved by the hospital's Clinical Research Ethics Committee in accordance with the guidelines of the Helsinki Declaration.
ResultsA total of 143 patients were analyzed of whom 104 (72.7%) started their treatment at least 12 months before completion of the study and therefore met the inclusion criteria established. Mean patient age was 49.8 years (± 12.6). A total of 52.9% of the study sample (n = 55) were male patients. The baseline characteristics of the population evaluated and the details of individual indications and lines of treatment of secukinumab are given in table 1.
Demographic characteristics, indication and line of treatment of patients treated with secukinumab
| Patients studied (n = 104) | Patients still on treatment (n = 48) | Patients who discontinued treatment by the end of the study (n = 56) | p value | |
|---|---|---|---|---|
| Mean age ± SD, years | 49.81 ± 12.56 | 48.71 ± 13.12 | 50.75 ± 12.10 | 0.414 |
| Male sex (%) | 55 (52.88) | 26 (54.16) | 29 (51.79) | 0.808 |
| Condition (%) | ||||
| Psoriasis | 54 (51.92) | 27 (56.25) | 27 (48.21) | 0.674 |
| Psoriatic arthritis | 30 (28.85) | 12 (25.00) | 18 (32.14) | |
| Ankylosing spondylitis | 20 (19.23) | 9 (18.75) | 11 (19.64) | |
| Line of treatment (%) | ||||
| First | 34 (32.69) | 22 (45.83) | 12 (21.43) | |
| Second | 13 (12.50) | 7 (14.58) | 6 (10.71) | 0.028 |
| Third | 24 (23.08) | 9 (18.75) | 15 (26.79) | |
| Fourth or further | 33 (31.73) | 10 (20.83) | 23 (41.07) |
SD: standard deviation.
Patients were classified according to the line of treatment they received: 34 patients were on first- line treatment [22 with psoriasis (64.7%), 8 with psoriatic arthritis (23.5%) and 4 with ankylosing spondylitis (11.8%)], 13 were on second-line treatment [9 with psoriasis (69.2%), 2 with psoriatic arthritis (15.4%) and 2 with ankylosing spondylitis (15.4%)], 24 were on third-line treatment [9 with psoriasis (37.5%), 8 with psoriatic arthritis (33.3%) and 7 with ankylosing spondylitis (29.2%)]; and 33 were on fourth-line treatment or further [14 with psoriasis (42.4%), 12 with psoriatic arthritis (36.4%) and 7 with ankylosing spondylitis (21.2%)]. No statistically significant differences were found in the distribution of patients according of the line of treatment they received (p = 0.261).
First-line treatments were initiated in September 2016. Five patients were started on secukinumab in the course of that year, 8 patients in 2017 and 21 patients in 2018. Given that most patients receiving second or further lines of treatment started taking secukinumab earlier than 2018, it can be said that that the follow-up of patients treated first-line was shorter than that of patients on further lines of treatment.
A total of 53.8% of patients (n = 56) discontinued treatment during the study period; mean duration of treatment in these patients was 12.7 months (± 10.2). The other patients (n = 48) were still being treated when the study came to an end, having received a total of 25.7 months (± 9.9) of treatment at that moment. No statistically significant differences were found between the two groups in terms of age, sex or condition. Nevertheless, 45.8% of patients treated until completion of the study were on first-line treatment while the majority of those who discontinued secukinumab had been receiving more advanced lines of treatment (p = 0.028) (Table 1).
Overall persistence at 12 months was 10.0 months (± 3.3). Of the 104 patients studied, 33 discontinued secukinumab during the first year, with a mean duration of treatment of 5.7 months (± 2.6). This means that the discontinuation rate at 12 months was 31.7%.
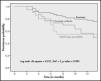
Persistence at 12 months per condition was as follows: 10.7 months (± 2.9) for patients with psoriasis, 9.7 months (± 3.4) for patients with psoriatic arthritis, and 8.8 months (± 3.8) for patients with ankylosing spondylitis, without any statistically significant differences between these groups (p = 0.085) (Figure 1).
As regards the reasons for discontinuation, 15 (26.8%) of the 56 patients who discontinued treatment experienced a primary failure and 27 (48.2%) a secondary failure, with a persistence of 3.8 months (± 1.1) and 18.6 months (± 9.6) respectively. Table 2 shows the specific reasons for discontinuation of the studied patients as well as their persistence details.
Reasons for discontinuation and persistence
| Patients who discontinued treatment (n = 56) | Persistence (in months)d | |
|---|---|---|
| Primary failure (%) | 15 (26.79) | 3.80 ± 1.11 |
| Secondary failure (%) | 27 (48.21) | 18.56 ± 9.57 |
| Therapeutic window (%) | 2 (3.57) | 7.75 (7.00-8.50) |
| Death from other reasons (%)a | 2 (3.57) | 20.00 (4.00-36.00) |
| Intolerance (%)b | 2 (3.57) | 6.50 (6.00-7.00) |
| Poor adherence (%) | 1 (1.79) | 6 |
| Loss of follow-up (%) | 1 (1.79) | 13 |
| Other causes (%)c | 6 (10.71) | 8.75 (3.00-26.00) |
Table 3 shows the distribution of patients in the sample as well as the persistence exhibited by those who stayed on secukinumab until the end of the study, those who discontinued as a result of a primary failure, and those who stopped their therapy because of a secondary failure, classified by indication and line of treatment. No significant differences were found in patient distribution as a function of their condition (p = 0.306). With regard to line of treatment, the differences observed proved statistically significant (p = 0.010), with higher persistence in patients receiving secukinumab as second-line treatment. Moreover, no significant differences were observed in the distribution of patients experiencing primary failure; 40% of patients with secondary failure were switched to third-line treatment and 44% to fourth or further lines of treatment.
Distribution of patients and persistence depending on whether they are still on treatment or whether they presented with primary or secondary failure, classified by indication and line of treatment
| Patients on treatment (n = 48) | Patients with primary failure (n = 15) | Patients with secondary failure (n = 27) | p value | |
|---|---|---|---|---|
| Indication (%) | ||||
| Mean persistence ± SD, months | ||||
| Psoriasis |
|
|
| |
| Psoriatic arthritis |
|
|
| 0.306 |
| Ankylosing spondylitis |
|
|
| |
| Line of treatment (%) | ||||
| Mean persistence ± SD, months | ||||
| First line |
|
|
| |
| Second line |
|
|
| 0.010 |
| Third line |
|
|
| |
| Fourth and further lines |
|
|
| |
SD: standard deviation.
Persistence of secukinumab was found to be comparable to that reported by other studies, with a 12-month persistence of 10 months and a 12-month discontinuation rate of 31.7%12. In line with previous work on the subject13,14, the reason for discontinuation in almost half of the patient sample was secondary failure. However, our mean persistence rate was higher than that reported by other authors.
In a study of over 1,500 patients with psoriatic arthritis treated with adalimumab, certolizumab, etanercept, golimumab and secukinumab aimed at evaluating adherence, persistence and discontinuation over a 12-month period, the lowest discontinuation rate corresponded to secukinumab (36.5%), which was also associated with the longest mean persistence (9.4 months)12. These results are similar to those observed in our sample for patients with psoriatic arthritis (32.1% discontinuation rate and 9.7-month persistence at 12 months).
In an Italian study including patients with psoriasis treated with secukinumab, 9.5% of subjects discontinued their treatment. As was also the case in our study, the majority of patients in the Italian cohort discontinued their treatment because of secondary failure, with 54.8% of patients exhibiting a 12-month persistence of 10.2 months13.
A French study that analyzed the discontinuation rate in patients with psoriasis on treatment with secukinumab found that 24.2% of patients abandoned their treatment, 15.0% of them because of secondary failure. In contrast to that, 48.2% of patients in our study discontinued their treatment, 59.3% of them because of secondary failure. Persistence in these patients was 20.9 months14. Accordingly, although our study was characterized by a higher discontinuation rate, the onset of primary failure occurred later than in the French study. In our study, patients who suspended treatment because of primary failure were evenly distributed across the three conditions considered.
A 76-patient study evaluating administration of secukinumab in patients with ankylosing spondylitis observed that 21.1% of patients discontinued treatment due to inefficacy15. Results of that study are similar to those of our own, where discontinuation due to primary failure stood at 27.3% in that group of patients. However, only 7.4% of patients with secondary failure in that study presented with ankylosing spondylitis. Moreover, persistence in those patients was longer than two years, which means that the patients with ankylosing spondylitis who experienced secondary failure did so later than patients with psoriasis or psoriatic arthritis. In our study, patients with ankylosing spondylitis who continued with their treatment exhibited lower persistence rates than those with psoriasis or psoriatic arthritis. This may have been due to the fact that the ankylosing spondylitis indication was obtained after the other two.
Most first- and second- line treatments in our study corresponded to patients with psoriasis, whereas patients with psoriatic arthritis and ankylosing spondylitis used secukinumab at more advanced lines of treatment. This difference may be attributable to the existence of an official consensus document (issued by the Pharmacy and Therapeutics Committee of the Murcia Region) on the use of biological therapies in patients with psoriasis, but not in those with the other two conditions. In patients who did not discontinue their treatment, persistence of first-line secukinumab was lower than persistence of the drug in the second or further lines of treatment. These data, however, may conceal a potential bias as most patients treated in the first-line context started their treatment in the course of 2018, which means that the observation time was much shorter than for the rest (20 vs. 38 months). This happened because the Pharmacy and Therapeutics Committee did not authorize the use of secukinumab for first-line treatment of psoriasis until May 201716. It is to be expected that these results will change as the follow-up of these patients increases.
It should be noted that of the 34 patients started on first-line treatment, only 2 (7.4%) experienced secondary failure, whereas 22 (45.8%) continued with their treatment. Patients on first-line secukinumab were the most numerous among those who stayed on treatment. On the other hand, of the 24 patients started on third-line treatment and the 33 started on fourth-line treatment and further, 40.7% and el 44.4%, respectively, experienced secondary failure. This means that patients on first-line secukinumab showed a better response, and those exposed to previous biological therapy exhibited a higher rate of secondary failures.
Similar findings were obtained by Williams et al.15, who reported a 16.7% discontinuation rate among their first-line patients vs. 25.0% and 21.4% for their second- and third-line patients, respectively. These data are in contrast with those published by Megna et al.13 and Ferrières et al.14, who did not find any connection between previous exposure to biological therapy and persistence of secukinumab.
A paper presented at the Annual Meeting of the Valencia Society of Rheumatology evaluated 12-month persistence in patients with psoriatic arthritis and ankylosing spondylitis treated with secukinumab. Of the 36 patients included in the study, 30 continued with their secukinumab treatment for a mean of 12.8 months (± 8.7). Six discontinuations were reported, attributed to primary failure (n=3), secondary failure (n=1), skin reaction (n=1) and loss of follow-up (n=1)17. A comparison of these results with those of our study reveals that, although the baseline characteristics of the subjects were similar, persistence of treatment in our patients was slightly lower (10.0 vs 12.8 months). Discontinuations due to primary failure were fewer (26.8% vs 50.0%) but the number of secondary failures was higher (48.2% vs 16.0%). These differences could be explained by the fact that our patients received secukinumab in more advanced lines of treatment. Moreover, this paper analyzes patients with psoriatic arthritis and ankylosing spondylitis but not with psoriasis, a disease present in over half the patients in our sample.
Our results should be interpreted within the context of the limitations associated with this study. Indeed, this is a retrospective analysis carried out in one single hospital with a limited number of patients. Furthermore, the evidence that the agent was prescribed and dispensed does not guarantee that it was actually used, which could result in a potential overestimation of persistence.
In short, our data attest to slightly higher persistence rates in patients with psoriasis and lower discontinuation rates in those without previous exposure to biological therapy. The latter finding is of particular interest as the use of secukinumab in the first-line setting would seem to lead to more effective results than its administration in more advanced lines of treatment.
This study broadens the current understanding of the real-life use of secukinumab. However, it is vital to conduct longer-term studies to confirm the results presented here as persistence could in the future come to be used as a decision-making criterion for placing secukinumab in the therapeutic algorithm for psoriasis, psoriatic arthritis and ankylosing spondylitis. Further research should also de dedicated to gaining a better understanding of the factors that may play a role in treatment persistence.
FundingNo funding.
Conflict of interestNo conflict of interest.
Contribution to the scientific literature
Data on the persistence of secukinumab being scarce in the literature, this study seeks to broaden the current understanding of its persistence in patients with psoriasis, arthritis psoriasis and ankylosing spondylitis. Our results provide information on the real-life performance of the drug as persistence is a concept that heavily depends on the drug's effectiveness and safety and on patient satisfaction. Our data show that persistence is slightly higher in patients with psoriasis and that discontinuation is less common in patients with no prior exposure to biological therapy.
These data could certainly prove very useful for our daily practice as they could be instrumental in our day-to-day decision-making processes regarding the prescription of biological therapies for patients with the stated conditions, and in the subsequent validation of secukinumab by the hospital pharmacist.
We believe that use of secukinumab as first-line biological treatment could be beneficial for patients suffering from any of the conditions analyzed in the study. Moreover, optimizing biological treatment in accordance with persistence is likely to favorably impact treatment costs and enhance the sustainability of the healthcare system.