The perioperative setting is one of the hospital areas with the highest prevalence of medication errors. Despite the wide experience of hospital pharmacists in developing medication safety programs and improvement initiatives, the perioperative setting has remained one of the areas in which there is less experience.
Clinical pharmacist should be integrated into the multidisciplinary care team so that they can be involved in the different surgical phases of care, which include from the preoperative assessment to inpatient stay, and finally discharge from hospital. Their work will consist of coordinating and implementing strategies that have been demonstrated to reduce medication errors during the perioperative process.
The aim of this paper is to introduce a specialized pharmaceutical care program to achieve excellence in the pharmaceutical care of surgical patients. This program is especially aimed at promoting the figure of the clinical pharmacist in the perioperative setting to guarantee the highest quality and safety in pharmacotherapeutic care throughout all the surgical phases of care.
El proceso quirúrgico es una de las áreas del hospital con más prevalencia de errores de medicación. A pesar de la amplia experiencia del farmacéutico en el desarrollo de prácticas seguras de utilización de medicamentos, el bloque quirúrgico ha sido una de las áreas en las que menos experiencia existe.
El farmacéutico especialista debe integrarse en el equipo multidisciplinar, de tal forma que pueda estar presente en todas las etapas de atención al enfermo (prehospitalización, precirugía, intracirugía, postcirugía y alta). Su función será coordinar y diseñar la puesta en marcha de diferentes estrategias que han demostrado reducir el riesgo de errores de medicación durante todo el proceso perioperatorio.
El objetivo del presente trabajo es presentar un programa de atención farmacéutica especializada para alcanzar la excelencia en la atención farmacéutica del paciente quirúrgico. Este programa está dirigido especialmente a visibilizar la figura del farmacéutico en el entorno perioperatorio, para que pueda colaborar en garantizar una atención farmacoterapéutica de máxima calidad y seguridad en todas las etapas.
In 1999, the Institute of Medicine published a report titled “To Err is Human: Building a safer health system”, which underscored the significant problem created by the clinical errors in the healthcare system, particularly those errors associated with the use of medicines, which are the most frequent and best-known ones. The report concluded that the most severe medication errors occurred in operating rooms (ORs), emergency wards and intensive care units.1
The perioperative setting presents with characteristics that distinguish the OR room from other areas or departments in a hospital, making medication errors more likely to occur.2–5 ORs tend to be the scene of high volumes of activity and constant patient turnover; the same anesthesiologist usually prescribes and administers the medication, without there being any other professional or technology to verify the appropriateness of the decisions made;6,7 patients are subject to a high number of care transitions over a short period of time, which is associated with a higher risk of mortality, morbidity and adverse events;and, a large proportion of the drugs used in the OR are considered high risk, i.e. medication errors related to these drugs are more likely to cause patients significant damage.8–11
For all these reasons, many organizations, both in Spain and internationally, have developed safety strategies aimed at minimizing avoidable medication errors in surgery and anesthesia. In this regard, the World Health Organization has launched, the initiative “Safe Surgery Saves Lives” as one of its global challenges aimed at enhancing the safety of surgical procedures.12 In Spain, the Ministry of Health, within its Patient Safety Strategy and in collaboration with the country's different autonomous regions, has promoted multiple safe practices aligned with international recommendations. The safe practices included in these strategies are basically addressed to promoting the safe use of medicines, preventing surgery-associated infections and optimizing patient care.13–17 All of these initiatives consider hospital pharmacists to be one of the key healthcare providers for the implementation of the different recommendations given their vast experience in developing safe practices for the use of medicines.18–21
In 2019, the American Society of Health-System Pharmacists published its guidelines on Perioperative Pharmacy Services, which specify what role should be played by pharmacists in the surgical setting.22 Nonetheless, evidence on the functions and the role played by perioperative pharmacists is still scarce. Consequently, it is essential to define the role played by pharmacists as members of the surgical team with a view to improving the standard of care provided to patient and ensuring a top-quality and highly-safe pharmacotherapeutic care throughout the surgical process.
The main goal of the present study is to introduce a Specialized Pharmaceutical Care Program (SPCP) intended to promote excellence in perioperative pharmaceutical care and underscore the important role played by pharmacists in the perioperative setting.
Design, development and implementation of the programThe SPCP program has been implemented in a third-level hospital in the Madrid region, which serves a population of 350,000 inhabitants. The hospital has over 1200 beds and 39 operating theaters, 34 for elective and 5 for emergency procedures. In 2019 a total of 32,618 surgeries were performed in the hospital and a new surgical block will be inaugurated sometime along 2022, which will bring together all the existing operating theaters and will be equipped with state-of-the-art technology to optimize efficiency.
Phases of the program- 1.
Setting up of the surgical pharmaceutic group and the multidisciplinary group.
In 2019, the FAQUIR (a portmanteau that blends the Spanish terms for Pharmaceutical and Surgical), group was formed within the hospital's Pharmacy Department. It was made up of six hospital pharmacists specialized in perioperative patient care. Subsequently, a multidisciplinary working group was constituted, whose remit was to enhance the safety of the perioperative setting. This group, which comprised pharmacists, surgeons, anesthesiologists and nursing staff, is led and coordinated by the hospital's management.
- 2.
Analysis of the baseline situation. Two initiatives were carried out:
- a)
A retrospective descriptive observational study was conducted on the perioperative use of medicines. In high-risk patients (anticoagulated, antiaggregated, ASA-IV and chronic patients requiring intensive intervention) subjected to major surgery. The data was obtained from the patients' electronic medical records, the hospital's electronic prescription program, and the primary care single e-prescribing module. The goal was to analyze the medication errors occurred during the perioperative process. Overall, a total of 4.9 medication errors were detected per patient, the most common ones associated with antibiotic prophylaxis (52.9%), medication reconciliation on admission (41.2%) and preoperative management of chronic medication (39.7%).
- b)
Failure Mode & Effects Analysis (FMEA) of the pharmacotherapeutic process involving perioperative patients. A multidisciplinary group was constituted made up of surgeons, anesthesiologists, nurses and pharmacists. Twenty-five failure modes were identified, as well as their potential causes and effects. The criticality index was calculated and analyzed for each failure mode and a series of measures were designed to prevent each kind of failure.
- a)
- 3.
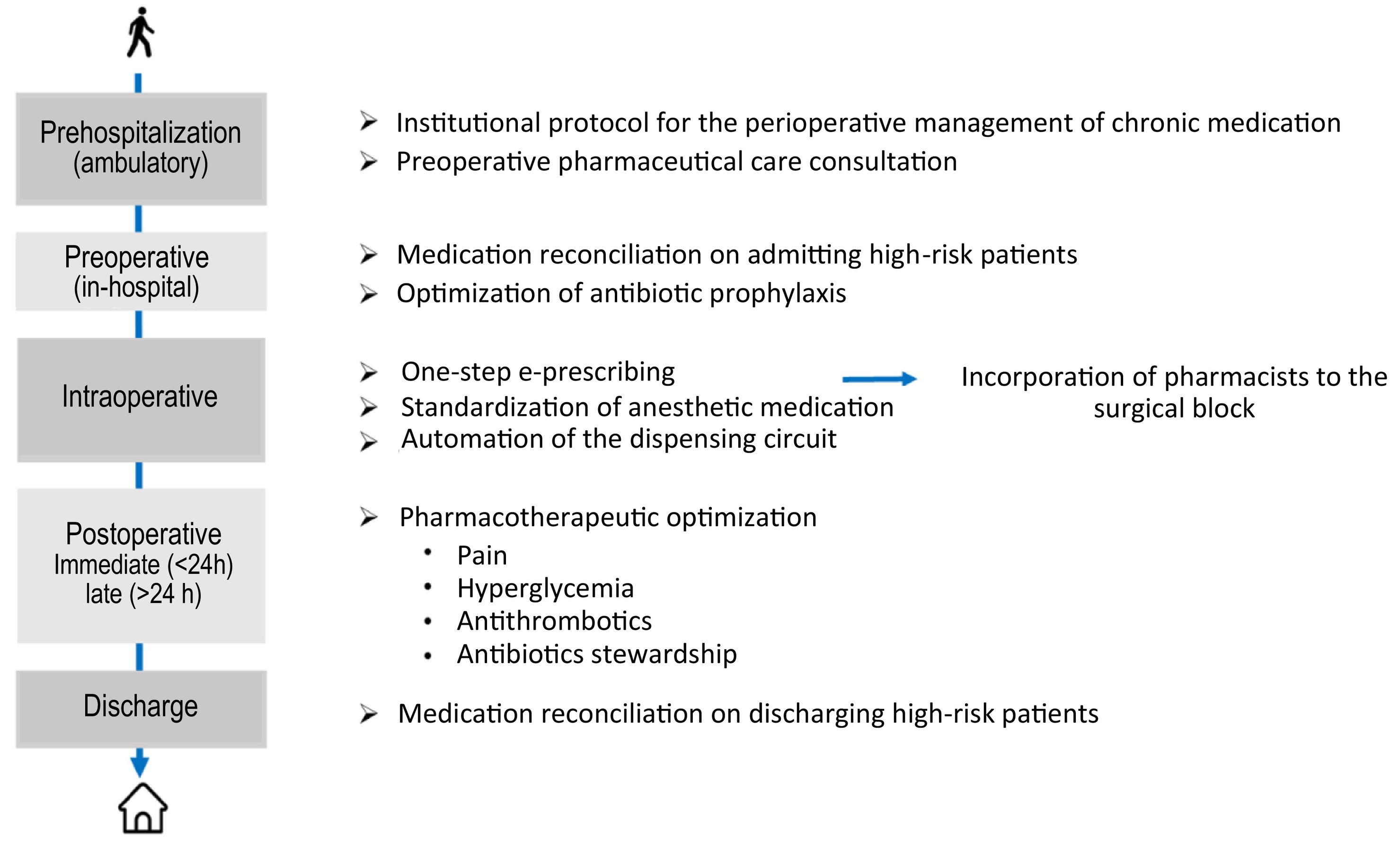
Based on the results of the study on the use of medication in perioperative patients and of the FMEA, the SPCP program was prepared, making sure it included activities covering the different phases associated with an elective procedure: prehospitalization, preoperative, intraoperative, postoperative, and discharge. The specific goals of the program are as follows:
- Coordinate the care provided to perioperative patients by developing new processes, implementing new technologies and designing an integral and multidisciplinary care.
- Promote a new stratification model aimed at ensuring that high-risk patients can access pharmaceutical care.
- Reduce the prevalence of medication errors throughout the perioperative process.
- Improve the health outcomes of perioperative patients.
- Enhance patient experience.
Fig. 1 summarizes the main activities contemplated by the SPCP program at the different stages of the perioperative circuit.
Prehospitalization phaseAt this stage, the SPCP program is focused on preparing an institutional protocol for the perioperative management of chronic medication. To minimize the heterogeneity of perioperative management recommendations made by different healthcare providers, it is indispensable for hospitals to avail themselves of an institutional protocol. Such a document is essential to avoid unnecessary cancelations of procedures as a result of poor pharmacological preparation. The hospital's Committee for Care Protocols and Clinical Pathways adopted a protocol of this kind and, to aid in its implementation, it will design a mobile app that displays in a simple and intuitive way specific recommendations according to the characteristics of the patient, the procedure and the indicated treatment.
Preoperative pharmaceutical care consultationsAt the present time, the time between the pre-anesthesia consultation and the procedure could be as long as 6 months. As a result, patients may not remember the preoperative management recommendations given to them. Also, their pharmacological treatment may have changed during that period, making those recommendations obsolete. The pharmacist is the last healthcare provider to have an (onsite/offsite) consultation with the patient before their admission for surgery. To homogenize the information obtained during pharmaceutical consultations, a clinical interview protocol was designed as well as a template to facilitate the insertion of information into the patients' electronic medical record. Such tools are available to all the members of the multidisciplinary team. The goals are:
- To confirm the existence of medical conditions that could require the adoption of presurgical measures. In cases of anemia, for example, patients may require administration of iron; in cases of renal failure, they may require an adjustment of their dosing regimen.
- To determine any medication allergies.
- To make a full record of the medicines, medicinal plants and food supplements the patient takes at home.
- To ensure that patients have understood the recommendations on the preoperative management of their medication made to them by the members of the anesthesiology department and determine whether any additional recommendations are needed.
- To dispense preoperative medication as appropriate according to the type of surgery performed (bowel cleansing solutions, etc.).
- To determine whether the patient is a candidate to the patient education program.
Given the high number of patients operated in the hospital, a stratification model was developed to ensure that all high-risk patients would access pharmaceutical consultations. The characteristics of these patients were defined based on the two studies conducted during the previous phase (prevalence of errors and y FMEA). Initially, all anticoagulated and antiaggregated patients as well as complex chronic patients and those with an ASA IV score were considered high-risk patients. Depending on the resources available, other kinds of patient such as transplanted, diabetic, Parkinson's or epileptic patients may be included.
Preoperative phaseThis is the period that extends from the patient's admission to their arrival in the operating room. During this phase, the SPCP program focuses on reconciling the patients' chronic treatment, confirming that the patient has made the required modifications and that the fasting guidelines have been followed. The pharmacist should also ensure the appropriateness of antibiotic prophylaxis.
Intraoperative phasePharmacists have been at the forefront of the development and implementation of e-prescribing and e-administration systems adapted to the operative setting. Such systems, characterized by their one-step or straightforward nature, involve prescribing medicines and recording their administration in one single step, using barcodes and touchscreens. To minimize variability and ensure that the process runs smoothly, prescriptions based on protocols, standard concentrations and connection with smart infusion pumps with automatic alarm systems (e.g., to detect allergies and prevent overdosing) are prioritized in clinical practice.
On the other hand, recourse to ready-to-use medicines and standardized medication trays for specific procedures (prepared by the Pharmacy Department) has been encouraged. Moreover, the new surgical block is expected to be equipped with radiofrequency systems capable of stocks management, tray replenishment and automatic cost allocation.
Postoperative phaseThis phase comprises two stages: immediate post-surgery (throughout which the patient remains in the post-anesthesia recovery unit) and late post-surgery (the patient is transferred to a general ward). The pharmacotherapeutic goals to ensure satisfactory outcomes during these two stages are as follows:
a) Pain management: This is a priority for the National Health System and plays a key role in their humanization and safety plans. The prevalence of acute postoperative pain is still high. According to the literature,23–25 appropriate pain relief not only enhances patients' wellbeing and satisfaction, but also contributes to minimizing postoperative morbidity and reducing the length of hospital stays. In this regard, pharmacist have spearheaded the development of standardized multimodal analgesia protocols within the e-prescribing program. At the same time, thanks to the electronic registration of VAS scores in patients' clinical records, a smart adverse event management tool (HIGEA)available in the pharmacy department makes it possible to identify and treat patients with uncontrolled pain.
b) Glycemic control: Hyperglycemia hampers healing, increases the infection risk and prolongs hospital stays. The HIGEA tool mentioned above is also capable of detecting patients with out-of-range glucose levels so that the required pharmacotherapeutic interventions can be made.
c) Thromboembolic disease: This is a key sentinel indicator of severe, potentially avoidable, postoperative complications. To prevent such complications, it is essential to screen every patient and identify those at a high risk of developing thromboembolic disease. To this effect, a thromboprophylaxis leaflet has been developed, which has been distributed among the hospital's healthcare professionals.
d) Infections: They lead to an increase in morbidity and mortality among perioperative patients. For this reason, hospital pharmacists must, together with the rest of the multidisciplinary team, contribute to the optimization of antibiotic treatment.
DischargePatients are discharged home with a list of specific recommendations that they must follow as well as a prescription for their pharmacologic treatment.
As well as reconciling the patients' medicines on admission, the pharmacist is also in change of ensuring that medications have also been properly reconciled on discharge. They must also confirm that patients understand their new medication regimen and that the new drugs have been inserted into the e-prescribing system. They are also responsible for remotely following up on high-risk patients.
In the case of perioperative patients, it is important to ensure that patients can avail themselves of adequate pain control and, if needed, thromboembolic prophylaxis in their homes. These aspects must also be checked by the pharmacist on discharge.
Evaluation of resultsA dashboard has been created for the SCPC program, for which the following indicators have been defined:
- -
Accessibility indicators: number of patients taken care of as a proportion of the overall number of surgical procedures performed in the hospital.
- -
Activity indicators: number (%) of perioperative patients included on pharmaceutical care programs (overall and by type of surgery); number of first and successive consultations; number of on-demand consultations; number of telemedicine consultations.
- -
Effectiveness indicators: mean length of hospital stay; number (%) of patients readmitted within 30 days with surgery-related complications; number of canceled surgeries as a result of inappropriate management of chronic medication.
- -
Safety indicators: number of grade E or higher adverse drug events (ADEs) avoided per 1000 perioperative patients served (classified according to the NCCMERP scale); cumulative incidence of de surgical site infection (overall and by type of surgery); number of hospital admissions in perioperative patients with a secondary diagnosis of pulmonary thromboembolism or deep venous thrombosis (overall and by type of surgery).
- -
Care quality indicators: these are related with patient-reported experience (PREM) and patient-reported outcomes (PROMs)
- -
Teaching and research indicators.
To evaluate the impact of the SCPC program and of the continuous improvement achieved, a post-implementation FMEA will be carried our once the new surgical block is fully operational.
ConclusionsThe SPCP program for perioperative patient is un new integrative and multidisciplinary care model, which is the first of its kind in the perioperative setting. The model requires the participation pharmacists in every process involving the perioperative patient with a view to ensuring the implementation of safe pharmacological practices based on a consensus among members of a panel of experts and the best clinical evidence and technological innovation available.
In the last few decades, multiple publications have demonstrated the significant impact of pharmaceutical interventions on the minimization of medication errors and, therefore, on the improvement of patient safety in different fields and specialties. Perioperative care has been one of the last areas where hospital pharmacists have been integrated into multidisciplinary care teams. There is little evidence on the real impact that the pharmacist's active involvement in the care of perioperative patient may have. The SPCP program could be used as a basis for the development of similar projects by other hospitals and to bring to the fore the pharmacists' contribution to the management of perioperative patients. It will also contribute to the generation of evidence on the different measures conducive to systematizing the management of these patients.
FundingThis study received the 4th Redacción Médica Award “Visibility of hospital pharmacists in the healthcare setting.”