Define consensus recommendations to improve care coordination between Hospital Pharmacy, Hematology and Nursing, inter- and intra-center, in the care of hemophilia patients.
MethodRecommendations for the improvement of care coordination in the management of hemophilia patients were identified and assessed by a multidisciplinary panel of professionals with experience in this field (Hospital Pharmacy, Hematology and Nursing) and supported by scientific evidence. The identified recommendations were assessed by Rand/UCLA consensus methodology (Delphi-adapted) based on their appropriateness and, subsequently, on their necessity. In both cases, it was used ordinal Likert scale. Data were statistically analyzed through different metrics.
ResultsFifty-three recommendations for the improvement of care coordination between Hospital Pharmacy, Hematology and Nursing in the management of hemophilia patients were identified, grouped into eight areas of action: i) Hemophilia units, reference centers and multidisciplinary care; ii) Role of Hematology, Hospital Pharmacy and Nursing in the patient journey of hemophilia patients; iii) Telepharmacy and telemedicine; iv) Pharmacokinetic monitoring; v) Transition to adult patient regimen; vi) Patient health education; vii) Surgery, emergency room and hospital admission; and viii) Outcome evaluation. All recommendations were assessed as appropriate and necessary by the external expert panel.
ConclusionsHemophilia patient journey is complex and depends on different variables. It also requires the involvement of different healthcare professionals who must act in a coordinated and integrated manner at all stages of the patient's life, adapted to their individual needs. On this matter, the identified and agreed recommendations may improve continuity and quality of care, as they facilitate the integration and coordination of the professionals involved in the management of this pathology, especially Hospital Pharmacy, Hematology and Nursing.
Definir recomendaciones consensuadas para mejorar la coordinación asistencial entre Farmacia Hospitalaria, Hematología y Enfermería, inter e intracentros, en la atención a los pacientes con hemofilia.
MétodoSe identificaron y valoraron recomendaciones para la mejora de la coordinación asistencial en el abordaje de los pacientes con hemofilia, por parte de un panel multidisciplinar de profesionales con experiencia en este campo (farmacia hospitalaria, hematología y enfermería) y apoyado en la evidencia científica. La valoración de las recomendaciones identificadas se realizó por metodología de consenso Rand/UCLA (Delphi-adaptado) en base a su adecuación y, posteriormente, a su necesidad. En ambos casos, se empleó la escala ordinal de Likert. Los datos se analizaron estadísticamente a través de diferentes métricas.
ResultadosSe identificaron 53 recomendaciones para la mejora de la coordinación asistencial entre farmacia hospitalaria, hematología y enfermería en el manejo del paciente con hemofilia, agrupadas en 8 ámbitos de actuación: i) unidades de hemofilia, centros de referencia y abordaje multidisciplinar; ii) papel de la hematología, la farmacia hospitalaria y enfermería en el recorrido asistencial de los pacientes con hemofilia; iii) telefarmacia y telemedicina; iv) monitorización farmacocinética; v) transición al régimen de paciente adulto; vi) educación sanitaria al paciente; vii) cirugía, urgencias e ingreso hospitalario; y viii) evaluación de los resultados. Todas las recomendaciones fueron valoradas por el panel de expertos externos como adecuadas y necesarias.
ConclusionesEl recorrido asistencial del paciente con hemofilia es complejo y depende de diversas variables. Además, requiere la implicación de distintos profesionales sanitarios que deben actuar de manera coordinada e integrada en todas las etapas de la vida del paciente, de manera adaptada a sus necesidades individuales. Las recomendaciones identificadas y consensuadas pueden suponer una mejora para la continuidad y calidad asistencial, pues facilitan la integración y coordinación de los profesionales implicados en el abordaje de esta enfermedad, especialmente de farmacia hospitalaria, hematología y enfermería.
Hemophilia is an uncommon chronic bleeding disorder that is inherited in an X-linked recessive pattern. This disorder is caused by a deficiency in the activity of coagulation factor VIII (hemophilia A) or IX (hemophilia B), due to mutations in their encoding genes. Hemophilia can be mild, moderate or severe, based on the levels of the deficient factor in the blood of the individual1.
Hemophilia mainly affects males and is inherited from the mother. Notably, near 30% of cases are caused by spontaneous mutations in individuals without a familial history of hemophilia1–7, while some authors suggest a proportion as a high as 50%8–10.
The global prevalence of this disease is estimated to be 1,125,000 in males, of whom 418,000 suffer from severe hemophilia11. Hemophilia A is significantly more frequent than hemophilia B12. In Spain, the disease affects near 3000 patients, with a hemophilia A-to-B ratio of 5:113.
The most frequent manifestation of hemophilia is tendency to bleeding, which appears at an early age1. Hemorrhages can be internal or external, and they can occur either spontaneously or as a result of trauma. Although 70–80% of hemorrhages occur within the joints or muscles1, they may also affect other organs and mucosa and is potentially life-threatening1.
Diagnosis of hemophilia is based on screening tests, analysis of coagulation factors, and genetic tests, with the latter providing a more specific diagnóstico. Once diagnóstico has been established, the therapeutic regimen for hemophilia can be administered either on-demand or for prophylaxis. The management of hemophilia traditionally involves intravenous administration of concentrates of the deficient coagulation factor (replacement therapy). Concentrations and frequency of administration will depend on the severity of the disease1. The emergence of new therapies (i.e. monoclonal antibodies) has led to a paradigm shift in the treatment and management of hemophilia. When treatment and prevention of bleeding are indicated, virtually all treatments for hemophilia are dispensed in the hospital setting1.
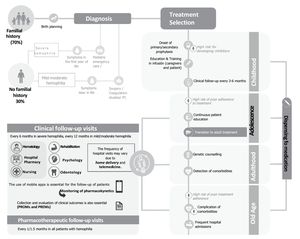
Since hemophilia is chronic, it requires lifelong, integral, close, individualized follow-up. The management of hemophilia is complex (Fig. 1), as it depends on variables such as age, lifestyle, familial situation, development of inhibitors against the deficient factor, presence of comorbidities, need for surgical procedures, and hospital admissions, among other factors. A diversity of health professionals from different specialties and levels of healthcare are involved in the healthcare journey of hemophilic patients (i.e. hematologists, specialist nurses, hospital pharmacists, musculoskeletal health professionals, psychologists, hemostasia laboratory specialists, and social workers, among others1). Hence, according to the World Federation of Hemophilia, these patients require integral, coordinated, multidisciplinary care1. Consequently, Hemophilia Units are acknowledged as an optimal organization model1.
Hospital pharmacists (HPs), in coordination with other members of the multidisciplinary team, play a relevant role in the management of patients with hemophilia. HPs are responsible for dispensing individualized treatments in personalized pharmaceutical care visits. Pharmacotherapeutic monitoring is also performed during these visits. HPs are also involved in the establishment of the therapeutic approach and monitoring of pharmacokinetics.
The purpose of this paper is to provide recommendations for improving inter and intra-center coordination between hospital pharmacists, hematologists and nursing professionals in the management of hemophilic patients at critical points of the healthcare journey.
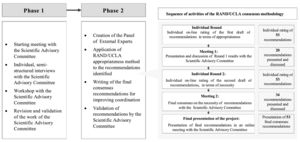
MethodsThe methodology was developed in two phases (Fig. 2).
In the first phase, a Multidisciplinary Advisory Committee (MAC) was created, composed of eight professionals with extensive experience in the management of hemophilia, including three HPs, two hematologists and three nurses. The healthcare journey of patients with hemophilia was identified and established. The MAC also defined the roles and scope of action of each professional throughout the healthcare journey. Also, semi-structured interviews and meetings were conducted to identify the aspects of coordination that needed to be improved. Finally, the MAC prepared the first draft of recommendations structured by areas of action.
Then, a Panel of External Experts (PEE) was created, involving 11 professionals of the areas of hospital pharmacy, hematology and nursing. The PEE and the MAC participated in the appropriateness rating rounds, following the Rand/UCLA appropriateness method14 (adapted Delphi) (Fig. 2). This method involves two individual rating rounds and two meetings to determine the appropriateness and necessity of recommendations by using a 9-point Likert's scale. During the two rounds, the panelists provided comments and explanatory opinions about each of the recommendations and added suggestions or other observations to improve the writing of recommendations. The data obtained was analyzed using statistical metrics: median; interquartile range (IQR); panelists that rated recommendations within the range of the median; level of appropriateness (A); level of necessity (N); and level of agreement or concordance(C).
During the first Delphi rating round, 18 panelists (8 members of the MAC and 10 of the PEE) were asked to rate electronically the appropriateness of a list of 53 recommendations. A recommendation was considered appropriate when its expected clinical benefits largely outbalanced the potential negative effects/risks of failing to provide a service. A recommendation was considered inappropriate when its potential negative effects outweighed the expected benefits. Finally, a recommendation was considered uncertain when there was a balance between its risks and benefits and there was no agreement or disagreement on it.
Each recommendation was analyzed and classified according to its level of appropriateness.
(median rating) and level of agreement of responses (Table 1).
Later, the MAC held the first meeting to discuss the recommendations rated as appropriate, on which there was agreement, and which had been suggested to be rewritten or clarified or on which there was some disagreement.
During the second Delphi rating round, 19 panelists (8 members of the MAC and 11 of the PEE) rated the appropriateness of a list of 53 recommendations. A recommendation was considered necessary when it met the following four criteria: (i) the recommendation is appropriate i.e., its clinical benefits exceed the risks by a sufficiently wide margin and make the service worth doing; (ii) failing to offer it to the patient would be inappropriate or considered malpractice; (iii) there is a reasonable possibility that the patient benefits from the key factor, and the magnitude of the expected benefit is not small. Each recommendation was analyzed and classified according to their level of appropriateness (median rating) and level of agreement of responses (table S1).
Following this rating round, the final recommendations were established, classified and prioritized according to their level of appropriateness and necessity. Then, the MAC and the PEE held a second meeting to discuss the recommendations that were considered necessary and with an indeterminate or uncertain level of agreement. The recommendations that had been suggested to be rewritten or clarified or on which there was disagreement were also discussed.
As a result, validated consensus recommendations were developed for the inter and intracenter coordination of the management of hemophilia.
ResultsAs a starting point in the identification of the recommendations to be promoted, the MAC firstly identified eight critical areas of coordination, based on the scientific evidence available and their professional experience (Fig. 3 and table S2).
For each of these eight areas of action, the MAC members identified opportunities for improvement, recommendations and roles of hospital pharmacists, hematologists and nurses in the healthcare journey of patients with hemophilia. A total of 53 recommendations were identified and rated, and level of agreement was assessed in Delphi rounds.
During the first Delphi round, 53 recommendations were rated as appropriate (median within the 7–9 range) and with agreement (>77.77% of panelists rated the recommendation within the range containing the median) and none of the recommendations was rated as inappropriate or uncertain, or as appropriate with indeterminate or uncertain agreement (table S1). Although there was no disagreement on any of the recommendations, some clarifications, suggestions and observations were incorporated to improve them. A total of 20 recommendations were discussed during the first meeting held with the MAC.
In the second Delphi rating round, panelists evaluated and rated all recommendations. A total of 53 recommendations were rated as necessary (median within the 7–9 range) and none was considered inappropriate or uncertain. With respect to the level of agreement, 51 recommendations were rated as necessary (median within the 7–9 range) and with agreement (>77.77% of panelists rated them within the range that contained the median). Two recommendations were rated as necessary with an undetermined or uncertain level of agreement. There was no disagreement on any of the recommendations (see table S1). The panelists also provided observations, explanatory opinions and comments to improve some recommendations. A total of 34 recommendations were discussed during the second meeting held with the MAC.
As a result, the final list of recommendations for the coordination of HPs, hematologists and nurses in the management of patients with hemophilia includes 53 recommendations structured into eight areas of action (Fig. 3 and table S2).
DiscussionA multidisciplinary approach, added to coordination of the health professionals involved in the management of patients with hemophilia, have been identified as key factors in the integral and specialized management of the disease1,15,16. It is crucial to identify the areas where coordination of the different professionals is critical for the management of hemophilia. This must be done considering the individual situation and needs of the patient, and promoting the involvement of patients in decision-making and disease control1. In specific settings such as elective surgery on hemophilic patients, a panel of experts has designed a set of practical consensus recommendations for its multidisciplinary management17.
In this work, a large group of health professionals used a robust methodology to identify a set of areas where coordination is critical. These areas include: providing health education and lifelong training to patients and caregivers; treatment policies (treatment selection and shifts); transition to adult treatment; monitoring of treatment adherence; coordination of clinical and pharmacotherapeutic monitoring visits; stock control during home dispensing; use of mobile applications; monitoring of pharmacokinetics; and performance of surgical or invasive procedures, and emergency care/ hospital admissions.
A total of 53 consensus recommendations grouped into critical areas of coordination are provided for improving coordination and communication between hematologists, HPs and nurses in the management of patients with hemophilia.
These recommendations could facilitate and promote, among others, the optimization of resources; coordination and communication between health professionals across the different levels of healthcare; clinical and pharmacotherapeutic monitoring; the establishment of an adequate relationship between the patient and the health professionals treating them, and the evaluation of clinical outcomes. These recommendations help define the differential role of the health professionals involved in the management of hemophilia, including hospital pharmacists.
They also consider it crucial that HPs are included as core members of the multidisciplinary team. This consideration is consistent with that given in previous studies defining the relevant role of hospital pharmacists in the management of patients with congenital coagulation disorders. These considerations acknowledge the benefits of involving HPs in the management of hemophilia18–21.
In this sense, the participation of HPs in the integral management of the disease (dispensing at 30–60 day intervals; decision making; onset, maintenance, and change of pharmacotherapeutic regimen; dosing and titration; selection of the types prepared based on their half-life; clinical and pharmacotherapeutic monitoring; monitoring of adherence; traceability; assessment of the cost-effectiveness of the treatment; medication use and stock control; and evaluation of clinical outcomes, among others). HPs also play a relevant role in the provision of health education to patients and caregivers, especially in terms of therapeutic regimen and (self)-administration of medication.
Evidence has also been provided of the benefits of the involvement of HPs in the detection of adverse events or medication-related events, as well as in the transition to adult treatments; the management of medications during invasive procedures and hospitalizations; and the promotion of telepharmacy and telemedicine initiatives, including the use of mobile applications. HPs should coordinate with other members of the multidisciplinary team on the basis of the resources available and local organization policies.
This document contributes to the identification of initiatives and actions that could potentially be implemented in centers treating patients with hemophilia in Spain in the context of each region and center.
Contribution to the scientific literatureIdentification of the areas of coordination of hospital pharmacists, hematologists and nurses in the management of patients with hemophilia.
Consensus recommendations can be implemented in these centers to improve healthcare quality.
FundingThis study was performed with the support of CSL-Behring.
AuthorshipAll patients included as authors participated in the conception and design of the study, defined its contents, and took part in the revision and writing of the paper. All authors approved the final version of the manuscript for submission for publication and meet the required conditions for submission. The list of author includes all persons involved in the study.
External panel of experts:
Antonio Palomero, Servicio de Farmacia Hospitalaria del Hospital Universitari Son Espases, Palma, Illes Balears.
Juan Carlos Juárez, Servicio de Farmacia Hospitalaria del Hospital Universitari Vall d'Hebrón, Barcelona, Cataluña.
Juan Eduardo Megías, Servicio de Farmacia Hospitalaria del Hospital Universitari i Politècnic La Fe, Valencia, Comunidad Valenciana.
Alberto Jiménez, Servicio de Farmacia Hospitalaria del Hospital Universitario Virgen de las Nieves, Granada, Andalucía.
José Pablo Quintero, Servicio de Farmacia Hospitalaria del Hospital Universitario Virgen del Rocío, Sevilla, Andalucía.
Olga Benítez, Servicio de Hematología del Hospital Universitari Vall d'Hebron, Barcelona, Cataluña.
María Teresa Álvarez, Servicio de Hematología del Hospital Universitario La Paz, Madrid, Comunidad de Madrid.
Violeta Martínez, Servicio de Hematología del Hospital Universitario de León, León, Castilla y León.
Carmen de Cos, Servicio de Hematología del Hospital Universitario Puerta del Mar, Cádiz, Andalucía.
Bolívar Díaz, Servicio de Hematología del Hospital General de Valdepeñas, Ciudad Real, Castilla-La Mancha.
María Estela Melado, enfermera del Hospital Universitari Vall d'Hebron, Barcelona, Cataluña.