The expression level of programmed death ligand 1 (PD-L1) is the only approved biomarker for predicting response to immunotherapy, yet its efficacy is not always consistent. Lactate dehydrogenase (LDH) has been associated with tumor aggressiveness and poorer prognosis across various cancer types and may serve as a useful biomarker for monitoring treatment response. The objective of this study is to analyze the relationship between LDH levels prior to the start of treatment with immune checkpoint inhibitors (ICIs) and clinical outcomes in patients with non-small cell lung cancer (NSCLC).
MethodA retrospective study was conducted including patients diagnosed with NSCLC who were treated with at least 3 cycles of immunotherapy. Data on demographics, clinical and pathological characteristics, treatment received, pretreatment LDH levels, and clinical outcomes such as treatment response and overall survival (OS) were analyzed.
ResultsA total of 181 patients diagnosed with NSCLC were included. Elevated pretreatment LDH levels (>244 U/L) were associated with significantly reduced OS. The median survival was 548 days in patients with LDH ≤ 244 U/L, compared to 332 days in those with LDH > 244 U/L (P = .037). Among men, OS was greater in the LDH ≤ 244 U/L group (623 days) versus 332 days in the LDH > 244 U/L group (P = 0.043). In patients with metastatic disease, OS was higher in those with LDH ≤ 244 U/L (474 days) compared to 249 days in those with LDH > 244 U/L (P = .023). In patients receiving both immunotherapy and chemotherapy, OS was greater in those with LDH ≤ 244 U/L (623 days) compared to 281 days in the LDH > 244 U/L group (P = .042).
ConclusionsHigh levels of LDH prior to the start of treatment with ICIs are associated with lower treatment efficacy and a worse prognosis of the disease, especially in male, metastatic patients with a PD-L1 expression level <1%.
El nivel de expresión del ligando 1 de muerte programada (PD-L1) es el único biomarcador aprobado para predecir la respuesta a la inmunoterapia, pero su eficacia no siempre es consistente. La lactato deshidrogenasa (LDH) se ha asociado con la agresividad tumoral y un peor pronóstico en varios tipos de cáncer, y podría ser un biomarcador útil para monitorear la respuesta al tratamiento. El objetivo de este estudio es analizar la relación entre los niveles de LDH previos al inicio del tratamiento con inhibidores del punto de control inmunitario (ICIs) y los resultados clínicos en pacientes con cáncer de pulmón no microcítico (CPNM).
MétodoSe realizó un estudio retrospectivo de pacientes diagnosticados de CPNM tratados con al menos tres ciclos de inmunoterapia. Se analizaron datos demográficos, características clínicas y patológicas, tratamiento recibido, niveles de LDH antes del tratamiento y resultados clínicos como respuesta al tratamiento y la supervivencia global (SG).
ResultadosUn total de 181 pacientes diagnosticados de CPNM fueron incluidos. Los niveles elevados de LDH (>244 U/L) antes del tratamiento con inmunoterapia se asociaron con una SG significativamente menor. La mediana de supervivencia fue de 548 días en pacientes con LDH ≤ 244 U/L, comparado con 332 días en aquellos con LDH > 244 U/L (p = 0,037). En hombres, la supervivencia global fue mayor en el grupo con LDH ≤ 244 U/L (623 días) frente a 332 días en aquellos con LDH > 244 U/L (p = 0,043). En pacientes con enfermedad metastásica, la supervivencia global fue mayor en aquellos con LDH ≤ 244 U/L (474 días) comparado con 249 días en aquellos con LDH > 244 U/L (p = 0,023). En pacientes tratados con inmunoterapia y quimioterapia, la supervivencia global fue mayor en aquellos con LDH ≤ 244 U/L (623 días) frente a 281 días en el grupo con LDH > 244 U/L (p = 0,042).
ConclusionesNiveles elevados de LDH previo al inicio del tratamiento con ICIs se asocian con una menor eficacia al tratamiento y un peor pronóstico de la enfermedad, especialmente en pacientes varones, metastásicos y con un nivel de expresión de PD-L1 < 1%.
Non-small-cell lung cancer (NSCLC) is one of the leading causes of cancer mortality worldwide.1 Despite significant advances in treatment strategies, including immune checkpoint inhibitors (ICIs), patient response remains variable and often unpredictable. Currently, programmed death-ligand 1 (PD-L1) is the only approved biomarker for predicting response to ICIs in NSCLC.2,3 However, correlations between PD-L1 levels and the efficacy of ICIs are inconsistent, highlighting the need for new biomarkers to better predict treatment response and disease prognosis.4,5
Lactate dehydrogenase (LDH) is an enzyme involved in anaerobic metabolism and has been associated with inflammatory processes and cell proliferation. Associations have been found between elevated serum LDH levels and greater tumor aggressiveness and worse prognosis in several types of cancer, including NSCLC.6,7 Recent studies have suggested that LDH may serve as a valuable biomarker for monitoring response to ICIs due to its association with tumor microenvironments and systemic inflammation.8,9
LDH is an intracellular enzyme involved in the glycolytic pathway, facilitating the conversion of pyruvate to lactic acid under anaerobic conditions. This enzyme exhibits increased glycolytic activity in tumor cells, leading to increased acidosis and a hypoxic microenvironment, which favors angiogenesis, immunosuppression, and tumor aggressiveness.10 This phenomenon highlights the importance of LDH as a marker of tumor burden and as a potential modulator of the immune response.11
In the context of NSCLC, studies have shown that elevated pretreatment LDH levels are associated with decreased overall survival (OS) and increased incidence of metastases, particularly in patients treated with ICIs.12,13 The literature suggests that LDH is not only useful as a biomarker of response to antineoplastic treatment, but may also be involved in the antitumor response itself.14 In vitro studies have confirmed that LDH inhibition is closely related to increased memory T-cell production and decreased immune evasion by tumor cells.15,16
Thus, the results of this analysis may have significant clinical implications by providing an additional tool for patient stratification and the personalization of treatment in patients with NSCLC. LDH could serve as a practical and cost-effective alternative biomarker, facilitating routine monitoring and therapeutic decision-making in clinical practice.
This study analyzed the relationship between pretreatment LDH levels and clinical outcomes in patients with NSCLC undergoing ICI therapy. The primary hypothesis was that elevated pretreatment LDH levels would be associated with lower ICI efficacy and worse disease prognosis.
MethodsA single-center retrospective study conducted at the Hospital Universitario de la Ribera (Alzira, Valencia) from August 2021 to February 2024. We selected patients diagnosed with NSCLC who received at least 3 cycles of immunotherapy with one of the following agents: nivolumab, pembrolizumab, atezolizumab, ipilimumab, or cemiplimab, either as monotherapy or in combination with chemotherapy. Inclusion criteria were as follows: a confirmed diagnosis of NSCLC at any stage; at least 3 cycles of treatment with the specified agents; and availability of clinical data including pretreatment LDH levels.
Data were collected from inpatient electronic medical records, including those registered in the outpatient prescription program of the Valencian Community (Abucasis) and the medical prescription program of the Hospital de la Ribera (NouSIS). Subsequently, the data were entered into an anonymized database.
The following variables were collected and analyzed: (1) demographic data (age, sex); (2) clinical and pathological characteristics (NSCLC stage, PD-L1 expression, tumor histology, and metastasis location); (3) treatment details (type of ICI as monotherapy or combined with chemotherapy); (4) LDH levels (pretreatment serum LDH levels using a cut-off upper limit of 244 U/L as established in our laboratory; and (5) clinical outcomes (survival based on LDH levels and treatment response, categorized as complete response, partial response, or disease stabilization, assessed according to RECIST v1.1 criteria).
LDH levels were measured using standard assays in blood samples obtained before initiating treatment with ICIs. PD-L1 expression was determined by immunohistochemistry in tumor tissue samples.
All statistical analyses were performed using SPSS v25.0 (IBM Corp., Armonk, NY). Continuous variables were expressed as means and standard deviations or medians and interquartile ranges, depending on their distribution, while categorical variables were expressed as frequencies and percentages. LDH groups were compared using t-tests for continuous variables, and chi-square tests for categorical variables. Survival curves were estimated using the Kaplan–Meier method and the log-rank test. In addition, Cox regression analyses were performed to identify independent factors associated with OS.
The study was approved by the hospital's Clinical Research Ethics Committee following the guidelines of the Declaration of Helsinki (reference code: HULR 22022022).
ResultsThe study included 181 patients diagnosed with NSCLC. Median age was 69 years (95% confidence interval [95%CI]: 64–76 years); the majority of patients were male (80.7%) and smokers (85.6%). Adenocarcinoma was the most common histology, accounting for 61.0% of patients, while 29.8% were classified as having epidermoid or squamous cell carcinoma. The remaining 9.4% had other NSCLC histologies (Table 1).
Baseline and demographic characteristics of the study patients.
| Variable | n (%) |
|---|---|
| Age (y), median ± 95%CI | 69 ± 64–76 y |
| Men | 146 (80.7) |
| Smokers | 155 (85.6) |
| Adenocarcinoma histology | 110 (61.0) |
| Squamous cell/epidermoid histology | 54 (29.8) |
| Other NSCLC histology | 17 (9.4) |
| Metastatic NSCLC | 130 (71.8) |
| PD-L1 expression | 171 (94.5) |
| First-line immunotherapy | 105 (58.0) |
| Immunotherapy (monotherapy) | 95 (52.5) |
| Immunotherapy + chemotherapy | 86 (47.5) |
NSCLC, non-small-cell lung cancer; 95%CI, 95% confidence interval; PD-L1, programmed death ligand 1.
PD-L1 expression was observed in 94.5% of patients and 71.8% had metastatic NSCLC. ICI was the first-line treatment in 58.0% of patients; 52.5% received monotherapy, while 47.5% received combination therapy with ICI and chemotherapy (Table 1).
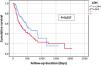
Kaplan–Meier survival analysis showed that patients with LDH levels above 244 U/L had a significantly shorter median survival (Fig. 1). Patients with LDH levels below 244 U/L had a median survival of 548 days (95%CI: 242–854), compared to 332 days (95%CI: 147–517) in patients with LDH levels above 244 U/L (P = .037) (Table 2). In addition, patients with LDH levels below 244 U/L had a statistically nonsignificant higher treatment response rate compared to patients with LDH levels above 244 U/L (P = .062) (Table 3).
Survival according to lactate dehydrogenase levels (244 U/L cut-off).
| LDH ≤244 U/L | LDH >244 U/L | P | ||||
|---|---|---|---|---|---|---|
| n | Median survival (d) | n | Median survival (d) | |||
| Total sample | 108 | 548 (95%CI: 242–854) | 73 | 332 (95%CI: 147–517) | .037 | |
| Sex | Male | 87 | 623 (95%CI: 222–1023) | 59 | 332 (95%CI: 121–543) | .043 |
| Female | 21 | 548 (95%CI: 50–1046) | 14 | 435 (95%CI: 244–626) | .550 | |
| Tumor histology | Adenocarcinoma | 66 | 548 (95%CI: 355–741) | 44 | 393 (95%CI: 119–667) | .209 |
| Epidermoid | 30 | 851 (95%CI: 266–1436) | 24 | 249 (95%CI: 4–494) | .252 | |
| Adenosquamous | 4 | 338 (95%CI: 260–416) | 1 | 441 (95%CI: -) | .362 | |
| Other NSCLCs | 7 | 234 (95%CI: 36–422) | 6 | 212 (95%CI: 28–396) | .087 | |
| Tumor stage | Locally advanced | 34 | 568 (95%CI: 389–624) | 17 | 605 (95%CI: 137–1073) | .771 |
| Metastatic | 72 | 474 (95%CI: 363–585) | 58 | 249 (95%CI: 111–387) | .023 | |
| PD-L1 expression | <1% | 38 | 497 (95%CI: 339–655) | 26 | 190 (95%CI: 13–367) | .033 |
| 1–49% | 29 | 361 (95%CI: 59–663) | 24 | 435 (95%CI: 154–716) | .884 | |
| >50% | 36 | 861 (95%CI: 303–1419) | 18 | 700 (95%CI: 133–1267) | .794 | |
| Unknown | 6 | – | 4 | – | – | |
| Immunotherapy | Monotherapy | 54 | 548 (95%CI: 210–886) | 41 | 435 (95%CI: 173–697) | .299 |
| Combined with chemotherapy | 54 | 623 (95%CI: 246–1000) | 32 | 281 (95%CI: 185–377) | .042 | |
| Type of ICI | Pembrolizumab | 64 | 548 (95%CI: 314–782) | 38 | 512 (95%CI: 237–787) | .417 |
| Atezolizumab | 14 | 474 (95%CI: 44–900) | 6 | 155 (95%CI: 53–257) | .091 | |
| Nivolumab + ipilimumab | 20 | 874 (95%CI: -) | 27 | 244 (95%CI: 27–461) | .093 | |
| Cemiplimab | 10 | – | 2 | 97 (95%CI: -) | .471 | |
NSCLC, non-small-cell lung cancer; 95%CI, 95% confidence interval; ICI, immune checkpoint inhibitor; LDH, lactate dehydrogenase; PD-L1, programmed death ligand 1.
Response to immunotherapy according to lactate dehydrogenase levels (244 U/L cut-off).
| Response to immunotherapy | LDH ≤244 U/Ln (%) | LDH >244 U/Ln (%) | P | |
|---|---|---|---|---|
| Type of response | Complete response | 10 (9.5) | 5 (7.6) | .062 |
| Partial response | 36 (34.3) | 18 (27.3) | ||
| Stabilization | 32 (30.5) | 13 (19.7) | ||
| Progression | 27 (25.7) | 30 (45.5) | ||
| Mortality rate at end of study | 45 (41.7) | 49 (67.1) | .001 | |
LDH, lactate dehydrogenase.
Table 2 shows the results divided into subpopulations with LDH levels above and below the 244 U/L cut-off. The results show significant differences by sex. In men, median survival was longer among those with LDH levels below 244 U/L, at 623 days (95% CI: 222–1023), compared to 332 days (95% CI: 121–543) in those with LDH levels above 244 U/L (P = .043). In women, the differences in survival were not statistically significant.
For patients with locally advanced disease, survival did not differ between those with different LDH levels. However, in the metastatic disease group, survival was significantly longer for patients with LDH levels below 244 U/L, with a median of 474 days (95% CI: 363–585), compared to 249 days (95% CI: 111–387) for those with LDH levels above 244 U/L (P = .023). The analysis of metastasis subtypes showed no significant differences between LDH levels in patients with central nervous system or liver metastases (P > .05). However, higher LDH levels were found in patients with bone metastases (P = .006) and adrenal metastases (P = .004).
In patients with PD-L1 expression below 1%, survival was longer in those with LDH levels below 244 U/L, with a median of 497 days (95% CI: 339–655), compared to 190 days (95% CI: 13–367) in patients with LDH levels above 244 U/L (P = .033). No significant differences in LDH levels were observed between subgroups with PD-L1 levels of 1%–49% and those with levels greater than 50%.
Finally, in patients treated with a combination of ICI and chemotherapy, median survival was significantly longer for those with LDH levels below 244 U/L, at 623 days (95% CI: 246–1000), compared to 281 days (95% CI: 185–377) for those with LDH levels above 244 U/L (P = .042). However, LDH levels did not significantly impact survival in patients treated with ICI monotherapy.
DiscussionThis study provides an accurate picture of the typical NSCLC patient population, with a predominance of male patients and smokers, with an advanced average age, and mostly diagnosed at advanced stages of the disease. The predominant histology was adenocarcinoma, which is the most common subtype of NSCLC.17
Our results are in line with other studies on various cancers, including NSCLC, where elevated LDH levels have been identified as a predictor of worse prognosis.18–20 Peng et al.21 and Sung et al.22 found decreased survival in patients with elevated LDH levels treated with PD-1 inhibitors. Meta-analyses by Zhang et al.13 and Deng et al.13 have shown that elevated pretreatment LDH levels are associated with survival in NSCLC patients treated with ICIs.
However, our Kaplan–Meier survival analysis showed that the survival curves of patients based on LDH levels crossed at the end of the study period. This may be due to patients receiving additional treatments after progression to immunotherapy, which could impact the survival of both groups to similar degrees. In addition, the patients' general health status and responsiveness to different treatments may change over time, potentially reducing the initial survival differences observed between the groups. These findings suggest the need for further analysis to better understand the factors affecting long-term survival in these patients.
The subgroup of patients with LDH levels below 244 U/L did not show a statistically significant difference in treatment response, likely due to the small sample size. However, by the end of the study period, there was a significant reduction in the mortality rate in patients with lower LDH levels (Table 3). This finding is consistent with the findings of previous studies.18–20
Our results suggest that LDH levels may have a more pronounced prognostic impact in men with NSCLC, which may be related to biological and hormonal differences that influence tumor progression and response to treatment.23 However, as women made up less than 20% of the study patients, these results should be interpreted with caution.
Pretreatment LDH levels significantly impacted patients with metastatic disease as well as those with PD-L1 expression below 1%, highlighting the potential of LDH as a predictive biomarker in NSCLC patients with poorer prognosis, where tumor burden and cancer aggressiveness are greater.24
Our data indicate that patients with high LDH levels undergoing ICI with chemotherapy have significantly lower survival rates than those with low levels. This further supports the potential role of LDH as a biomarker to identify patients who might derive less benefit from certain treatment regimens and may require alternative therapeutic strategies.24,25
However, this study has several limitations. The retrospective, single-center design introduces inherent bias and limits the generalizability of the findings to other clinical settings. In addition, the small sample size affects the consistency of the results and the ability to detect significant differences in smaller subgroups.
Our findings suggest that elevated LDH levels prior to ICI treatment are associated with reduced treatment efficacy and poorer prognosis, particularly in male patients with metastatic disease and PD-L1 expression below 1%. Therefore, measuring serum LDH levels prior to treatment initiation may provide valuable information regarding prognosis and response to ICIs in patients with NSCLC.
Contribution to the scientific literatureThese findings reinforce the relevance of LDH not only as a biomarker of tumor burden, but also as a modulator of the immune response, providing new insights into its role in clinical oncology.
In clinical practice, LDH measurement prior to ICI treatment could improve patient stratification and personalize treatment, providing a practical and cost-effective tool for therapeutic decision-making in NSCLC.
FundingWe have not received any funding for the completion of this research.
Declaration of funding interestNone declared.