Several studies quantitatively described patients with Chronic Myeloid Leukemia on active treatment with tyrosine kinase inhibitors, however there are few qualitative studies that focus their results on how to accompany patients in the course of the disease over time. The objective of this review is to find out what are the expectations, information needs and experiences that determine adherence to treatment with tyrosine kinase inhibitors in patients with Chronic Myeloid Leukemia in qualitative research articles published in the scientific literature.
MethodsA systematic review of qualitative research articles published between 2003–2021 was carried out in PubMed/Medline, Web of Science and Embase databases. Main keywords used were: “Leukemia, Myeloid” and “Qualitative Research”. Articles on the acute phase or blast phase were excluded.
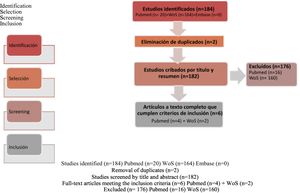
Results184 publications were located. After elimination of duplicates, 6 (3%) were included and 176 (97%) publications were excluded. Studies show that the illness is a turning point in patients' lives, and they develop their own strategies for managing the adverse effects. The factors that determine medication experiences with tyrosine kinase inhibitors should be addressed by implementing personalized strategies: this would result in early detection of problems, reinforce education at each stage and promote open discussion about complex causes underlying the treatment failure.
ConclusionsThis systematic review provides evidence that implementation personalized strategies must be done to address the factors that determine the illness experience with Chronic Myeloid Leukemia and receiving treatment with tyrosine kinase inhibitors.
Diversas investigaciones cuantitativas generan evidencia sobre los pacientes con leucemia mieloide crónica y el tratamiento activo con inhibidores tirosina cinasa, pero son escasas las investigaciones cualitativas que orienten sus resultados a cómo acompañar a los pacientes a lo largo de su enfermedad. El objetivo es conocer las expectativas, las necesidades de información y las experiencias condicionantes al usar inhibidores tirosina cinasa en los pacientes con leucemia mieloide crónica en los estudios cualitativos publicados en la literatura científica.
MétodosSe revisaron sistemáticamente investigaciones cualitativas publicadas entre 2003 y 2021 en Pubmed/ Medline, Web of Science y Embase de pacientes con leucemia mieloide crónica tratados con inhibidores tirosina cinasa. Las palabras clave fueron «Leukemia, Myeloid» y «Qualitative Research». Se excluyeron artículos sobre la fase aguda o blástica.
ResultadosSe localizaron 184 publicaciones. Eliminando los duplicados, se incluyeron 6 (3%) y excluyeron 176 (97%). Los estudios muestran la enfermedad como inflexión en la vida de los pacientes, quienes desarrollan sus propias estrategias para controlar los efectos adversos. Los factores que determinan la experiencia farmacoterapéutica con inhibidores tirosina cinasa deben abordarse mediante estrategias personalizadas: esto permitiría la detección temprana de problemas, reforzaría la educación en cada etapa y promovería la discusión abierta sobre las causas complejas que subyacen al fracaso del tratamiento.
ConclusionesEsta revisión sistemática evidencia que abordar los factores que determinan la experiencia de enfermar de leucemia mieloide crónica y recibir el tratamiento con inhibidores tirosina cinasa debe realizarse implementando estrategias personalizadas teniendo en cuenta las necesidades de los pacientes.
Chronic myeloid leukemia (CML) is a specific kind of cancer that originates in bone marrow cells. Clinical guidelines have defined it1 as “a clonal malignant hematologic neoplastic disease of pluripotent stem cells, which belongs to the chronic myeloproliferative neoplasm category.” CML is induced by a reciprocal translocation between the long arms of chromosomes 9 and 22, generating the so-called aberrant Philadelphia chromosome which, in turn, translates into a BCR-ABL oncoprotein with tyrosine kinase function.
According to the literature, CML typically develops asymptomatically, “with no signs of splenomegaly and lower levels of leukocytosis in patients with better prognosis”2. The condition is often diagnosed following a routine medical examination or blood test. Treatment should begin immediately after diagnosis3. The disease usually develops in three phases: chronic, accelerated and blast (acute leukemia). For patients at the chronic phase, tyrosine kinase inhibitors (TKIs) have unseated chemotherapeutic agents and interferon as standard of care. TKIs have become the gold standard treatment of choice for CML.
The purpose of chronic CML treatment with TKIs is to obtain and maintain a hematologic, cytogenetic and molecular response, prevent progression to the acute or blast phase and minimize toxicity. TKIs indicated for newly-diagnosed CML include imatinib, dasatinib, nilotinib and bosutinib.4 To ensure a satisfactory response, patients must maintain strict adherence and take their prescribed treatment every day, following the recommendations of their physician, as the success of treatment is heavily dependent on compliance5.
The ADAGIO6 trial showed that only 14.2% of patients took their prescribed dose of imatinib and strictly followed the recommendations of their physician. In cases of optimal response, the percentage of non-adherent patients was 7.3%. The percentage on non-adherence was higher (23.2%) among patients with a suboptimal response. In this regard, Marín et al.7 suggested that the inability to obtain satisfactory molecular responses in CML patients treated with imatinib for a few years may be related to difficulties in achieving adherence. For this reason, the aim of this systematic review is to go beyond adherence and focus on understanding the patients' experience with their medication, analyzing how they strive to cope with their disease and their treatment. We believe that gaining an understanding of the patients' experiences, beliefs and preferences, which play an essential role in determining their attitudes vis-à-vis their medication, is key for optimizing adherence, enhancing therapeutic results8, and improving what has come to be called the patients' medication experience9.
During the chronic phase, patients are typically seen to by their hospital's pharmacy department on the basis of the CMO pharmaceutical care model (Capacity, Motivation, Opportunity)10 within the framework of the Outpatient Care Strategic Map Project (MAPEX)11, according to which patients are followed up closely and receive personalized pharmaceutical care. During consultations, the hospital pharmacy staff evaluate the effectiveness of their treatment and assist them in preventing and minimizing adverse events. Moreover, great emphasis is laid on encouraging adherence and setting goals regarding the results to be expected from treatment9. In this regard, an in-depth analysis of patients' remarks is carried out to help pharmacists and the whole healthcare team adopt optimal shared decisions12, which invariably involve patients as active participants in their treatment and in the management of their chronic disease. An effort is also made to clarify patients' doubts and answer the questions that may come up during the disease process.
Multiple quantitative studies have been performed13–15 that report on the adherence of CML patients on active treatment with TKIs. However, not much qualitative work has been done to provide guidance on how to support patients throughout a long-term disease. The purpose of this review was to gain an understanding of CML patients' expectations, information needs and experiences when using TKIs, based on the qualitative studies published in the literature. We specifically sought to focus on:
- A.
CML patients' experience with their illness16 and their medication17
- B.
CML patients' information needs
- C.
CML patients' expectations about their treatment
- D.
CML patients' management of medication and potential adverse events
- E.
CML patients' relationship with the healthcare professionals taking care of them.
- F.
CML patients' experiences that may influence the way they manage their treatment.
A systematic review was carried out based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines18 to identify, select, analyze and summarize qualitative research articles published on the subject.
The search strategy for any systematic review of qualitative studies should reformulate the research question, translating it from a PICO (Population, Intervention, Comparison, Outcome) question into one aligned with the SPIDER (Sample, Phenomenon of Interest, Design, Evaluation, Research type) formula19 (Table 1):
Research question in SPIDER format and its equivalence in PICO format.
| P- Population | S - Sample | Patients with chronic myeloid leukemia treated with tyrosine kinase inhibitors |
| I- Intervention | PI-Phenomenon of Interest | Expectations, information needs and experiences with an impact on adherence |
| C-Comparison | D – Design | Studies using qualitative methods |
| O- Outcome | E- Evaluation | Studies related with the phenomenon of interest: opinions, perceptions, qualities, narratives, among others. |
| R - Research type | Qualitative methods: in-depth interviews, focus groups, etc. |
The search was conducted in the Pubmed/Medline, Web of Science (WoS) and Embase databases for articles published between 1 January 2003 and 3 October 2021. The MeSH (Medical Subject Headings) terms used were those regarded as the most appropriate descriptors. A restricted search strategy was employed, combining all the descriptors included in Table 2 by Boolean operations. Search strategy #6 (“Leukemia, Myeloid” [MeSH] AND “Qualitative Research”[MeSH]) was replicated in the WoS and Embase data bases.
Presence of numerical results on the references obtained by each descriptor or their combinations in Medline.
| Search | Descriptors | Results |
|---|---|---|
| #1 | “Leukemia, Myeloid, Chronic-Phase”[MeSH]) | 984 |
| #2 | “Leukemia, Myeloid, Chronic-Phase”[MeSH]) AND “Qualitative Research”[MeSH] | 0 |
| #3 | “Leukemia, Myeloid, Chronic-Phase”[MeSH]) AND “Narrative Medicine”[MeSH]) AND “Patient Medication Knowledge”[MeSH]) AND “Medication Therapy Management”[MeSH]) AND “Qualitative Research”[MeSH] | 0 |
| #4 | “Leukemia, Myelogenous, Chronic, BCR-ABL Positive”[MeSH] | 20.694 |
| #5 | “Leukemia, Myeloid” [MeSH] | 100.044 |
| #6 | “Leukemia, Myeloid” [MeSH] AND “Qualitative Research”[MeSH] | 20 |
MeSH:Medical Subject Headings.
The selection and review of the original articles was performed by applying the selection criteria listed in Table 3, on the basis of the articles' title and abstract. The process was carried out by two independent reviewers, both of them hospital pharmacists providing pharmaceutical care to hemato-oncological patients. Any discrepancies were resolved through a consensus discussion with one of the pharmacists on the research team. Methodological discrepancies were discussed with the anthropologist pharmacists, who evaluated the methodological quality of the present review by ensuring that it complied with the SRQR standards (Standards for Reporting Qualitative Research)20.
Article selection criteria.
| Selection criteria: |
|
| Exclusion criteria: |
|
CML: chronic myeloid leukemia; TKI: tyrosine kinase inhibitor.
A total of 182 publications were identified. As shown in Fig. 1, after application of the inclusion/exclusion criteria, only six studies were finally included. Table 4 shows the distribution and classification of the publications identified.
Studies included.
| Article, title | Author, year | Population, location | Patients included | InterventionResearch question | Data collection method | Analysis and processing of data |
|---|---|---|---|---|---|---|
| Needs for information and reasons for (non)adherence in chronic myeloid leukemia: Be aware of social activities disturbing daily routines. | Boons et al. 2018 | Patients treated in 9 hospitals.The Netherlands | N = 13Age:27–73Female:8Male:5 | Understand the reasons for nonadherence. Information and communication needs. | Questionnaire.Semi-structured interview | Mixed methodsAnalysis of the qualitative thematic framework |
| Disease acceptance and adherence to imatinib in Taiwanese chronic myeloid leukemia outpatients. | Chen et al. 2014 | Patients treated in a cancer center, Taiwan | N = 42Age: 20–80 yearsFemale:19Male:23 | Explore the experience of patients with imatinib as well as those attitudes that could impact their adherence | Semi-structured interview | Constant comparison method |
| Antes e depois da CML: experiências e dimensões da leucemia mieloide crônica como uma rotura biográfica. | Alzate et al. 2014 | Patients treated in a hematology referral center. Edgard Santos.University Hospital. Salvador de Bahía (Brazil). | N = 6Age:23–62 yearsFemale:3Male: 3 | Experiences of patients with CML about their disease | Interviews with a narrative approach | Narrative analysis based on an indexing of categories intended for text analysis |
| Lack of congruence between patients' and health professionals' perspectives of adherence to imatinib therapy in treatment of CML: A qualitative study. | Wu et al.2015 | Patients and HCPs. Specialized center in Australia (Peter MacCallum Cancer Center). | N = 16Age: 26–71Female:7Male:9,HCPs: N = 10 | Experience of the use of imatinib, adherence barriers and enablers according to the experience of patients and HCPs | Face-to-face interviews based on a standard semi-structured format. | Investigation-Participation-ActionPhenomenologic- interpretive analysis |
| The Patient Journey in Chronic Myeloid Leukemia Patients on Tyrosine Kinase Inhibitor Therapies: Qualitative Insights Using a Global Ethnographic Approach. | Guilhot et al. 2013 | Patients with CML from online individual or community clinical practice centers in Brazil, France, Germany, Russia and Spain. | N = 50Age: 21–80Unspecified gender distribution of participants | Evaluation of the effects of diagnóstico and treatment on patients with CML. It provides recommendations to the HCP in change of patient support. | In-depth interviews.Patients from Brazil and France were given the option of participating in two additional phases of the project: preparing photo journals and keeping a diary during the 7 days prior to the interview and a subsequent telephone interview. | Ethnography |
| Experiences of living with chronic myeloid leukemia and adhering to tyrosine kinase inhibitors: A thematic synthesis of qualitative studies. | Hewison et al. 2020 | Chronic CML, age > 18 years, males and females, any location, qualitative studies, chronic use TKI, outpatient management | 9 studies included | Thematic synthesis of different experiences of living with CML | Data extracted included quotes from the participants, investigators' summaries, and analytical concepts and interpretations. | Full coding of extracted data, using indictive codes based on the goals of the study |
N: number of patients; CML: chronic myeloid leukemia; TKI: tyrosine kinase inhibitor; HCP: healthcare professional.
Sixteen of the articles excluded were from Pubmed/Medline. Fourteen of these (87.5%) were found to deal basically with acute leukemia and 2 (12.5%) turned out not to be related to CML but rather to transplantation and leukemia in children. As regards the 160 excluded studies obtained from WoS, 103 (64%) dealt with acute leukemia, 30 (19%) with diagnostic and analytic techniques, and 27 (17%) were unrelated to CML. One-hundred percent of the articles selected based on their title and abstract were analyzed in full-text form. Inter-reviewer concordance with respect to the full-text study selection achieved a kappa index of 0.92.
The six studies that were finally included were subjected to an information extraction, description and analysis process. These studies on CML, which came from Brazil, Australia, France, the Netherlands, Germany, Russia, Spain and Taiwan, typically looked into aspects related to diagnóstico, disease control, patient experience, adherence and relationship with healthcare professionals (HCPs). The qualitative methods used were as follows: narrative analysis, phenomenological/interpretive analysis, ethnographic analysis, mixed methods and constant comparison. All the studies included patients, and only one also included HCPs.
Results of the analysis of the studiesBelow is a description of the main characteristics of the six studies analyzed:
- Boons et al. (2018), the Netherlands. Influence of social activities on the use of TKIs. Boons et al.21 published a mixed methods study based on a questionnaire and semi-structured interviews. The goal was to obtain information on the reasons why patients did not adhere to their CML medication and on their need and desire for information and communication. A cohort of CML patients (≥18 years) treated with TKIs was recruited and asked to fill out a questionnaire. Subjects were subsequently asked to participate in a semi-structured interview. Sixty-one patients (54 ± 12 years, 43% male), treated with imatinib (n = 32), dasatinib (n = 10) or nilotinib (n = 19), filled out the questionnaire. Thirty-three patients (54%) used TKIs as first-line treatment, 29 of them were on imatinib (87,9%). Patients were being treated at 28 Dutch hospitals. Fifteen (25%) patients reported that they missed a dose at least once a month. Most patients were not concerned about missing a dose, and never raised these omissions with their HCP. Finally, 13 patients (8 female and 5 male) aged between 27 and 73 years, coming from nine different hospitals, were interviewed. The reported causes of non-adherence were that the treatment interfered with their social activities (such as celebrations) and their daily routine, and the wish to avoid the side effects of the treatment. Patients expressed a wish to be provided with extensive and comprehensible information about all the aspects involved in their CML treatment, particularly its side effects. They also wished for greater support from HCPs.
- Chen et al. (2014), Taiwan. Acceptance of CML and chronic CML treatment with imatinib. Chen et al.22 looked into the perceptions, attitudes and concerns that may impact adherence to treatment with imatinib. The study was conducted in the outpatient oncology department of a medical center in Taiwan. The study cohort comprised patients with CML who attended the outpatient oncology department regularly from October 2011 to March 2012 to receive treatment with imatinib. Semi-structured face-to-face interviews were used to explore patients' experiences and opinions on their treatment, their current CML status, the ways in which CML had impacted their health, their concerns about their treatment and their adherence to imatinib. Interviews were recorded, transcribed verbatim, and thematically analyzed using the constant comparative method. The study deals with the patients' opinions on their disease and health condition and with how their concerns and anxieties impact their adherence to imatinib. Forty-two patients aged between 20 and 80 years participated in the study. The emerging topics included: acceptance of the existing disease and health status, misconceived notions on the progression of the disease, factors associated with adherence to imatinib and anxieties about the way adverse events should be managed. Participants rightly considered CML a chronic disease, but harbored misconceived ideas about the progression of their disease, its follow-up, resistance to imatinib and the symptoms resulting from adverse events. On the whole, they all followed the recommendations on how imatinib should be taken and showed a preference for long-term prescriptions, which might spare them from having to visit the hospital regularly to collect their medication. Adverse reactions were the main barrier to adherence, and typically resulted in polypharmacy. Most participants adapted the way they took their medication so as to maintain long-term use of imatinib.
- Alzate et al. (2014). Brazil. Experiences and dimensions of CML as a biographical disruption. Alzate et al.23 analyzed the experience of CML patients as a biographical disruption at three levels: (1) the meanings of illness and CML as life threatening, (2) physical and social disruption and stigmatizing experiences, and (3) the before and after perception of CML, focusing on changes in self, in social relations, and in daily life. This is a qualitative study that included six patients between 23 and 62 years of age treated in Brazil. The analysis of the patients' narratives in connection with their illness experience constitutes the mainstay of the study's methodology. Field work for this study took seven months. As regards the three biographical disruption levels, the authors explain the following:
- (1)
CML as a threat: suspicion and confirmation of the abnormality took place in association with a trivial occurrence, a routine examination or an incidental finding. Narratives about this initial phase included in some instances references to the exact number or to an excessive increase of white blood cells in the blood. Patients said that they would not mention anything to their friends or family. Uncertainty tended to be present at different moments along the way. Being seen to by a hematology consultant was described as an unexpected relief or as reason for hope. The study also explains the impact of the word leukemia on participants' lives.
- (2)
Physical and social disruption and stigmatizing experiences: some patients reported experiences where they felt rejected by their neighbors or friends due to lack of awareness or knowledge. The sociocultural significance of cancer emerged bringing to the fore the lethality of this often hidden or suppressed condition.
- (3)
Perceptions before and after suffering from CML, changes in self, in social relations and in daily life: leukemia is perceived as a bombshell, a turning point that permanently changes the patient's life and marks a watershed between the things they could do before and those they can do now. The importance of living the moment was underscored by most patients. CML forced patients to negotiate their life and identity with the disease, to define a new relationship with the health system and with HCPs, and to deal with the ambiguities involved in suffering from a severe disease. Relationships with HCPs appear in patients' narratives as sources of hope.
- Wu et al. (2015). Australia. Lack of consistency between the perspectives of patients and HCPs. HCPs were not aware of the complex underlying causes. Wu et al.24 tried to identify barriers to and enablers of adherence to TKIs by analyzing the experiences of patients with CML. The study included 16 patients and 10 HCPs (4 hematologists, 3 nurses and 3 pharmacists). Semi-structured qualitative interviews were administered. Each interview was manually recorded, transcribed, anonymized and analyzed by means of a phenomenological/interpretive analysis. A total of 12 patients were included and at least one instance of nonadherence was detected. The causes of unintentional non-adherence (forgetfulness or changes in routine) were recorded. Reasons for intentional adherence included a desire to reduce dose-dependent adverse events, inadequate support and poor physician-patient communication. Patients with higher nonadherence rates were those who, after considerable periods of sustained disease control, received contradictory advice on adherence. The information obtained was structured into themes and subthemes: (1) Management of the disease: tolerance of treatment, search for alternative medicine options. (2) Perspectives: promotion, adherence and awareness of the disease; comparisons with others. (3) Adherence strategies: patient education, triggers, advances in crisis management and in clinical practice. (4) Risks of nonadherence: complacency, inconsistency, poor adherence detection methods. (5) Reasons for unintentional nonadherence: forgetfulness and poor communication. (6) Reasons for intentional nonadherence: reducing the impact of the treatment on patients' lives, access to medical devices.
- Guilhot et al. (2013), a multi-site ethnographic analysis. Patients need support, education, reassurance and continuity of care to improve their experience with their medication. Guilhot et al.25 ethnographic study included 50 CML patients between 21 and 80 years of age from individual clinical practice centers or online communities from Brazil, France, Germany, Russia and Spain. The study's in-depth interview is based on an extensive semi-structured script, which made it possible to subsequently classify findings into five stages that CML patients go through during the diagnóstico, treatment and management of CML: crisis, hope, adaptation, new normal and uncertainty. Findings were subsequently classified into initially characterized, eventually characterized, key findings, challenges, patients' representative phrase, and recommendations for HCPs at each one of the phases. In this regard, it was concluded that HCPs can help patients as they move through the crisis and hope stages, showing them their support, promoting healthcare education, and providing reassurance. When patients reach the adaptation and new normal stages, HCPs can help them establish realistic expectations on the risks and benefits of chronic long-term drug therapy, the follow-up of the disease and the advantages of adherence. The different stages were affected by patients' emotional and social expectations, their understanding about CML, their positive relationship with HCPs and/or their treatment and their optimism about their long-term prognosis.
- Hewison et al. (2020), a thematic synthesis. Patients with CML typically experience significant side effects as a result of their treatment, which more often than not undermine their psychological and physical wellbeing. Hewison et al.26 is a thematic review. The purpose of this synthesis was to gain an understanding of the factors influencing patient adherence to TKIs. The publications included were extracted from five electronic databases. All the qualitative studies included examined adults with CML on TKI treatment (9 in all). Results were structured around three general predefined topics, within which other aspects were also analyzed:
- (1)
Impact of the disease: The authors made specific reference to the side effects impacting the patients' physical and psychological wellbeing, which often lead them to develop their own strategies to control them, thus improving adherence. As regards activities of daily living, many of them are impacted by CML and its treatment: work, leisure, family roles, stigmatization resulting from the disease. Consequently, patients often adapt their routine, their work and their pastimes so that they can cope with and manage their disease and their treatment. Being diagnosed with CML comes a real shock, which creates anxiety and a concern about one's health, often accompanied by pessimistic thoughts and fear of the new situation. This phase is succeeded by an acceptance and adaptation phase, where patients increase their understanding of the disease and become concerned with their analytical results and the progression (or lack thereof) of their condition.
- (2)
Disease management strategies: Patients develop their own strategies to deal with their treatment with TKIs, often with family support. Some patients refuse to consult with HCPs regarding suspending their medication or how to deal with their side effects. They fail to report missing doses either because they do not want to disturb HCPs or because they do not consider it important. Some patients resort to alternative or complementary medicine. As regards nonadherence, two kinds were distinguished: intentional and unintentional (forgetfulness, difficulties in accessing medications, cost…). Adherence-related decisions are heavily influenced by the patient's health condition and social status. Nonadherence could also be encouraged by the reassurance that HCPs tend to provide when patients admit to having missed a dose. Patients' information needs changed over time and across individuals. Patients' understanding about their treatment was often scarce and prone to confusion.
- (3)
Appraisal of the care provided by HCPs: Patients were positive about the psychological support provided by HCPs, their accessibility, their caring attitude and the reassurance they provided. As regards consultations with HCPs, an open and individualized approach facilitating discussions on symptoms, adherence and the patients' perspectives about living with CML would be most welcome as, according to the literature, such an approach would result in a higher quality of care.
The six qualitative studies included in this review article describe the impact of CML on patients' lives. Diagnosis of CML completely changes their hopes, their prospects and their approach to life. Although the illness experience is described in all the studies, Alzate et al.23 turn it into the central axis of their analysis. Analyzing CML as a multi-level biographical disruption makes it easier for HCPs to understand the different phases patients go through as well as the emotional pain and suffering they experience. Graffigna et al.27 pointed out that a better understanding of patients' experience may provide HCPs with a clearer idea of the emotional triggers they should act on, of how to improve their relationship with their patients, and of how to get them to become more involved with their treatment. Guilhot et al.25 ethnographic study uses extensive semi-structured interviews as a method to segment the patients' illness experience into a series of stages (crisis, hope, adaptation, new normal and uncertainty) and to make specific recommendations to HCPs for each stage of the disease process. This constitutes a useful contribution for future research and a tool that can by itself be applied in clinical practice.
As regards the patients' experience with their medication, according to the findings of the studies analyzed in this review, patients with CML experience significant side effects, which impact their psychological and physical wellbeing. Consequently, as CML is a chronic disease they must learn to live with, patients typically develop their own strategies to control the disease and manage their treatment and the resulting side effects. Chen et al.22 pointed out that, although Taiwanese CML patients did adhere to imatinib, the drug's side effects had changed their attitude toward taking other chronic medications. Selecting a CML treatment that is simple and adaptable to patients' everyday routines may be a key factor for bolstering their quality of life and adherence, as indicated by Hirji et al.28 Consequently, against a background characterized by behavioral and adaptative changes, the pharmacists' role may be crucial as they are the HCPs in charge of seeing to the patient before they take their medication. Pharmacists should inform patients about the adverse events resulting from the medications prescribed to them and guide them as to how to best deal with such side effects. This could help increase patients' perception of disease control and reduce the treatment's negative impact on their quality of life. Considering that pharmaceutical consultations are not just an occasion to discuss CML medication but also to review the effectiveness of concomitant treatments, they could be used as an opportunity to provide patients with comprehensive guidance about their treatment.
As far as the patients' information needs are concerned, these differ depending on the stage of the disease they are at. It would be advisable to analyze the factors involved at each different stage and adapt the information provided, the resources assigned and the interventions carried out so as to best respond to the patients' needs in a personalized way.
Boons et al.21 mentioned another aspect that ought to be considered when applying the recommendations made in the articles reviewed to clinical practice. Indeed, these authors stated that nonadherence occurred when patients altered their daily routines. This is something that could well be investigated by future studies as it would be useful to identify the activities that most affect the lives of patients as they attempt to use their medication as prescribed. Specifically, it would be interesting to know whether this is a phenomenon related to a specific age bracket or if it responds to other circumstances (seasonality, weekly distribution, social patterns, etc.). Findings would allow clinicians to develop a proactive prevention strategy and make relevant recommendations. Boons et al.21 also mention that nonadherence does not constitute a cause for concern for many patients and it is therefore not brought up with the clinician or discussed in an open or proactive way. This is also reported by Wu et al.24, who explain that the complex causes resulting in behavioral changes and the emotions that may affect the use of medication still remain unknown. In this regard, it should be considered that, due to a social desirability bias, patients -being subject to the judgment of HCPs- tend to behave in the way they believe is expected of them. Although chronic patients, particularly those with CML, are repeatedly informed about the importance of adherence, the way they respond will depend on whether they feel they are being judged. From a qualitative standpoint, the point is not to judge whether patients are being truthful, but rather to understand why they act the way they do and how they cope with the difficulties involved in using their medications. It is essential to take this into account and establish a therapeutic relationship that allows an open dialog where patients feel free to discuss the factors preventing them from taking their medication or those that may make them miss a dose. Although they are the most commonly used tools to determine adherence in clinical practice, questionnaires are considered insufficient to tackle this problem as they do not probe into the causes or the biopsychosocial circumstances that influence patients' medication-taking habits.
The papers included in this review comprised a qualitative thematic synthesis (Hewison et al.26) that, in turn, examined studies on how to survive with CML and be adherent to the prescribed medication. This means that, from a methodological standpoint, we are in a position to compare our results. Methodologically, the differences with respect to Hewison et al.26 in the number of articles identified may be due to the fact that their thematic synthesis was performed on the basis of five electronic databases whereas in our review we only used three. Also, differences exist regarding the goals pursued. Indeed, Hewison et al.26 only focused on adherence as a biomedical concept quantifiable through questionnaires, while the purpose of the present systematic review was broader in that it sought to enlarge the qualitative dimension of every patient's experience. The illness experience16 and medication experience17 concepts were useful in our analysis as they contributed a comprehensive biopsychosocial perspective of the patients' pharmacotherapeutic needs29. Nevertheless, Hewison et al.26 thematic synthesis confirms the importance of resorting to psychological support and emotional management strategies30 to cope with the impact that the disease exerts on their lives.
All the studies analyzed underscore the need to improve communication between patients and HCPs: Wu et al.24 identified inconsistencies between the patients' and the HCPs' perspectives. Chen et al.22 stated that patients often harbor misconceived ideas about their disease and their medication. HCPs play a key role in providing patients with the support and motivation they need to improve actively management of their medication17. The patient-HCP relationship emerges from the reviewed articles in the form of “hope” and “trust” and, occasionally, as “relief.” These findings are in line with the literature. Pioneering studies such as Haynes et al.31, or more recent analyses such as Brown et al.32 and Polinski et al.33 have demonstrated that the most significant variable affecting adherence is the HCP-patient relationship. HCPs should take this into consideration and be mindful of the fact that patients rely on them all along the various stages of the disease.
A series of cross-sectional factors, such as the sociocultural stigma of cancer, the difficulties accessing the required medication or the cost of medication, have also been analyzed in studies other than those reviewed here. Nonetheless, one should identify and analyze the beliefs associated with the disease and its treatment in each biopsychosocial setting and anticipate the specific barriers patients may encounter. In Spain, the cost of TKI treatment is defrayed by the National Health System: patients are not required to pay for their medications or the tests needed to follow up their condition. Conversely, in other countries where access to these drugs and the follow-up of the disease constitute an economic limitation, adherence and follow-up may be impacted. This could affect the translation and applicability of our findings as the studies reviewed were carried out in countries whose health systems and sociocultural contexts are very different from those in Spain.
The results of the present review should be interpreted taking into account several potential limitations. First and foremost, the findings are based on only six articles. Methodologically, one of the most serious problems is the fact that many articles do not incorporate the MeSH term “qualitative research,” which makes it difficult to locate them when performing a literature search. Moreover, the gray literature was excluded from the search as were all articles not available in Spanish, French, English and Portuguese, which could limit the global relevance of our findings. The SRQR guidelines20 were followed for critically analyzing the selected articles. This made it possible to extract our results and conclusions ensuring that the analysis was based on studies that met the required standards for qualitative research.
As regards the practical implications of the above, the present review of qualitative studies constitutes a theoretical framework for future field research. The most appropriate way of understanding the pharmacotherapeutic experience29 of patients diagnosed with CML should be to resort to the so-called Comprehensive Medication Management (CMM) approach9, which allows pharmacists to investigate the factors influencing patients' beliefs, perceptions, concerns, expectations, attitudes, motivations and behaviors with regard to their treatment at the same time as they perform their strictly pharmaceutical duties. Supporting patients during the long journey of using TKIs as treatment for CML could help meet their pharmacotherapeutic needs with regard to their decisions and their social background, from a technical-scientific, clinical and human perspective34.
In short, the studies reviewed emphasize that CML marks a huge turning point in patients' lives. The present analysis provides substantial evidence that patients develop their own disease and adverse event management strategies and underscores the significant benefit of providing patients with personalized, empathetic care that caters for their needs. The study also points out that HCPs are often unaware of the complex factors influencing their patients' medication experience.
The factors determining the experience of being diagnosed with CML and receiving TKI treatment should therefore be approached by implementing personalized strategies. This would allow early detection of problems, it would strengthen education at the different stages of the disease and it would promote an open discussion on the causes of nonadherence and, above all, on the complex factors resulting in difficulties or even in the failure of TKI treatment.
Contribution to the literatureOur research, which followed the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines for systematic reviews, examined a series of qualitative studies by adapting the PICO (Population, Intervention, Comparison, Outcome) question to the SPIDER (Sample, Phenomenon of Interest, Design, Evaluation, Research type) formula, which facilitates the analysis of narratives, points of view, discourses, experiences and perceptions, among other qualities inherent in the use of medicines. Qualitative investigation makes it possible to understand the causes of the behaviors, beliefs and experiences that determine patients' health outcomes.
This review hopes to provide HCPs with the tools they need to treat patients with a comprehensive approach, incorporating a biopsychosocial perspective and some elements pertaining to the human sciences. At the same time, we hope to make it easier for HCPs to come to terms with complex realities such as nonadherence, shared decision-making or the suffering of their patients. We believe that our qualitative approach, which differs from the quantitative approach typically used in hospital pharmacy studies, may be applied to future investigations in this or other domains, contributing new conceptual frameworks with implications for our daily practice.
FundingNo funding was received to carry out this review.