Given poor medication adherence in severe asthma is difficult to evaluate in daily practice, using at least two methods concurrently is recommended. We aimed to determine the prevalence of nonadherence to inhalers using the Test of Adherence to Inhalers questionnaire and the medication possession ratio obtained from the pharmacy refill data in patients with severe asthma treated with anti-interleukin-5 biologics and to evaluate their concordance.
MethodThis was a cross-sectional retrospective observational study of 53 patients with severe asthma recruited from the severe asthma unit of a tertiary hospital in Madrid from June to December 2020. We registered demographic data, comorbidities and concomitant therapy for asthma. Nonadherence was defined as pharmacy refill data < 80% and/or Test of Adherence to Inhalers questionnaire results < 50. Concordance was assessed by determining the Cohen's kappa statistic.
ResultsThe median age was 61 years (interquartile range 51.8–67.0), and 33 (61%) were women. According to the pharmacy refill data lack of adherence to the primary inhaler was 58.5%. However, when using the Test of Adherence to Inhalers questionnaire, it was 22.6%. Combining both methods, 17% of patients were considered to have nonadherence to inhalers. Likewise, when identifying nonadherence by either of these methods, it reached a prevalence of 64.2%. The pharmacy refill data and Test of Adherence to Inhalers questionnaire agreed in 53.1% and disagreed in 46.9% of patients (k = 0137; 95% confidence interval -0.057 to 0.331; p = 0.318).
ConclusionsWe observed a higher prevalence of non-adherence to inhalers in patients with severe asthma treated with anti-interleukin-5 biologics. The agreement between the Test of Adherence to Inhalers questionnaire and the pharmacy refill data is lower when evaluating nonadherence in patients with severe asthma treated with anti-interleukin-5 biologics. The pharmacy refill data detect a higher proportion of nonadherence compared with the Test of Adherence to Inhalers questionnaire.
Dado que la mala adherencia a la medicación en el asma grave es difícil de evaluar en la práctica diaria, se recomienda utilizar al menos dos métodos simultáneamente. El objetivo es determinar la prevalencia de la falta de adherencia a los inhaladores mediante el cuestionario Test de Adherencia a los Inhaladores y la ratio de posesión de la medicación obtenida a partir de los datos de dispensación de la farmacia en pacientes con asma grave tratados con biológicos anti interleucina 5 y evaluar su concordancia.
MétodoEstudio observacional retrospectivo transversal de 53 pacientes con asma grave reclutados en la unidad de asma grave de un hospital terciario de Madrid de junio a diciembre de 2020. Se registraron datos demográficos, comorbilidades y el tratamiento concomitante para el asma. La falta de adherencia se definió como una ratio de posesión de la medicación < 80% y/o un valor en los resultados del cuestionario Test de Adherencia a los Inhaladores < 50. La concordancia se evaluó con el coeficiente kappa de Cohen.
ResultadosLa mediana de edad fue de 61 años (rango intercuartílico 51,8–67,0), y 33 (61%) eran mujeres. Según la ratio de posesión de la medicación, la falta de adherencia al inhalador primario fue del 58,5%. Sin embargo, al utilizar el cuestionario Test de Adherencia a los Inhaladores, ésta fue del 22,6%. Combinando ambos métodos, se consideró que el 17% de los pacientes presentaban no adherencia a los inhaladores. Asimismo, al identificar la no adherencia por cualquiera de estos métodos, se alcanzó una prevalencia del 64,2%. El cuestionario Test de Adherencia a los Inhaladores y la ratio de posesión de la medicación coincidieron en el 53,1% y discreparon en el 46,9% de los pacientes (k = 0,137; intervalo de confianza del 95% -0,057 a 0,331; p = 0,318).
ConclusionesSe observó una alta prevalencia de no adherencia a los inhaladores en los pacientes con asma grave tratados con biológicos anti interleucina 5. La concordancia entre el cuestionario Test de Adherencia a los Inhaladores y la ratio de posesión de la medicación es menor cuando se evalúa la no adherencia en pacientes con asma grave tratados con biológicos anti interleucina 5. La ratio de posesión de la medicación detecta una mayor proporción de no adherencia en comparación con el cuestionario Test de Adherencia a los Inhaladores.
One of the major issues in asthma is the lack of adherence to inhaled therapies, which is observed in nearly 50% of patients1. Poor asthma treatment compliance is associated with higher morbidity and mortality and with greater use of health services2.
Many studies have attempted to identify which factors are associated with nonadherence. Noncompliance has been related to the patient's own characteristics (e.g., age, sex, sociocultural level, poor experiences with previous treatments, depression, lack of social support), complexity of the inhalation regimen, peculiarities of the inhaler devices and the type of inhaled agent3,4.
To measure adherence to inhalers, direct and indirect methods are employed. Direct methods, which include electronic monitoring and drug levels, are based on the quantification of a drug, its metabolites or a tracer substance in a biological fluid (blood, urine, saliva or skin). These methods are objective, specific, accurate and reliable, but also expensive, complex and can only be used with some drugs3. In contrast to direct methods, indirect ones, such as obtaining clinical information by anamnesis, are economic and can be employed for all inhalers. However, they tend to provide erratic results5. Accordingly, in clinical practice, use of validated questionnaires with acceptable reliability is recommended. Therefore, the Spanish Society of Pneumology and Thoracic Surgery has developed the Test of Adherence to Inhalers (TAI) questionnaire to assess patient compliance when receiving inhalers in daily clinical practice. As mentioned previously, however, self-report questionnaires tend to overestimate compliance6, so that the use of concurrent methods to measure adherence, such as medication withdrawal in pharmacies obtained from pharmacy refill data (PRD), are recommended when using questionnaires6–8. According to this strategy, and due to the simplicity, low cost and acceptable reliability of both methods, the Global Initiative for Asthma (GINA) and the Spanish Guideline on the Management of Asthma propose using them concurrently6,7.
Previous studies that have evaluated the degree of inhaler compliance using the TAI questionnaire and PRD in patients diagnosed with asthma, analysed all severities of asthma together and have not been focused on patients receiving specific biologic treatments to control asthma2,9. The use of anti-interleukin-5 (anti-IL-5) therapy agents in the treatment of asthma has been associated with improvements in respiratory symptoms, lung function and control of the disease10–14. Therefore, we suspect that the high efficacy of anti-IL-5 biologics in controlling asthma might predispose patients to abandon treatment with inhalers and, as a consequence, to reduce the adherence to inhaled therapy. For this reason, we aimed to determine the prevalence of nonadherence to inhaler medication based on the TAI questionnaire and PRD in patients with severe asthma treated with anti-IL-5 biologics and to define the degree of concordance between these two measures.
MethodsStudy designThis was a cross-sectional, retrospective, observational study that analysed adherence to inhaled therapy using two different methods: the results of the TAI questionnaire registered in the electronic medical record, and the dispensing of inhalers registered in the pharmacy records. The analyses were conducted using data collected during the six months prior to the start of the study in December 2020.
We included patients followed-up by the severe asthma unit of a tertiary hospital belonging to the National Health System in Madrid. Asthmatic patients are referred to this unit when they had a not-controlled asthma disease despite of using high doses of combined corticosteroid and long-acting beta (2)-agonist inhalers or oral corticosteroids during 6 months7. The severe asthma unit was following 95 patients at the time of the study, 57 (60%) of whom were receiving treatment with anti-IL-5 biologics. The inclusion criteria were (1) age ≥ 18 years; (2) use of anti-IL-5 biologics; and (3) availability of TAI questionnaire results in the medical records. We excluded patients not residing in the Community of Madrid, because the registry of drugs dispensed in the community pharmacy was not available. Possible prescriptions by private doctors were not taken into account as the patients are followed up by a severe asthma unit of the National Health System, and therefore all prescriptions for their chronic disease are handled by this unit.
The study was conducted in accordance with the Declaration of Helsinki and was approved by the Research Ethics Committee of La Paz University Hospital. All personal data were anonymised.
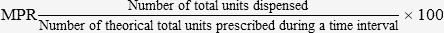
Evaluation instrumentsPharmacy refill dataPRDs were obtained from the patients’ pharmacy records. To measure adherence, we calculated the medication possession ratio (MPR), according to the following formula:
We included the units prescribed and dispensed by the pharmacy in the previous 6 months. The cutoff point for considering nonadherence was < 80%, in accordance with the report by Karve et al.15, which showed that hospitalisations were associated with this MPR in prevalent chronic diseases
Similar to previous studies9, the PRD were used to measure adherence to the primary inhaler. For this purpose, we considered as primary inhaler the combination of drugs in a single inhaler, as stated in the GINA guidelines6. Thus, given that only patients diagnosed with severe asthma were included, we considered the primary inhaler as combination therapy with an inhaled corticosteroid (ICS) and a long-acting β-agonist (LABA). In all the other cases, the primary inhaler was the device that contained inhaled corticosteroids.
Test of adherence to inhalersThe TAI questionnaire is a validated test consisting of a 10-item questionnaire that patients complete. All patients followed-up by the severe asthma unit are asked to answer the TAI questionnaire routinely. The scoring range for each question goes from 1 (poorest compliance) to 5 (best compliance), providing a total score that ranges from 10 (minimum) to 50 (maximum). It classifies patients as nonadherent when the score is < 50 and identifies the specific type of nonadherent behaviour16,17. We employed the first score registered in the medical records during the same period as when the PRD were calculated.
Study variablesPrimary variable: Proportion of patients classified as not having therapeutic adherence measured by both of the following methods:
The demographic variables consisted of age and sex.
The comorbidities were smoking, chronic obstructive pulmonary disease, bronchiectasis, allergic bronchopulmonary aspergillosis, nasal polyposis, gastroesophageal reflux, anxious-depressive syndrome, vocal cord dysfunction and aspirin-exacerbated respiratory disease.
The inhaled and concomitant therapies were LABA, long-acting muscarinic antagonists, short-acting beta2-agonists, short-acting muscarinic antagonists, oral corticosteroids, montelukast and anti-IL-5 biologic.
Statistical analysisThe quantitative variables were expressed as medians (interquartile range [IQR]). For the categorical variables, frequencies and proportions were employed. To compare the quantitative variables, the Mann–Whitney U test was used; in the case of qualitative variables, the chi-squared test or Fisher's test was used. Concordance was assessed by determining the Cohen's kappa statistic. The SPSS (IBM SPSS Statistics version 19.0) programme was used to analyse the data, and differences with p < 0.05 were considered to be statistically significant.
ResultsPatients’ characteristicsA total of 57 patients were initially selected. Four patients were excluded due to outdated PRD or minor age; therefore, 53 patients were finally included. The median age was 61 years (IQR 51.8–67.0), and 33 (61%) were female. Concerning coexisting illnesses, 77.3% of patients had treated comorbidities; in particular, rhinoconjunctivitis (61.0%), nasal polyposis (38.0%) and anxiety or depression (35.6%). The comorbidities are described in table 1.
Demographic characteristics and patients' comorbidities under pharmacologic treatment
| Variable | n = 53 (100) |
|---|---|
| Age | 61 (51.8-67.0) |
| Female sex | 20 (39%) |
| Treated comorbidity | n = 41/53 (77.3) |
| Rhinoconjunctivitis | 25 (61.0) |
| Nasal polyposis | 16 (38.0) |
| Anxiety and depression | 15 (35.6) |
| Gastroesophageal reflux | 7 (17.1) |
| Bronchiectasis | 6 (14.6) |
| Aspirin-exacerbated respiratory disease | 5 (12.2) |
| Allergic bronchopulmonary aspergillosis | 1 (2.4) |
Data expressed as medians (IQR) and numbers (percentages).
All patients were undergoing treatment with LABA or ICS combination inhalers, and 75.5% had an associated long-acting muscarinic antagonist (LAMA) inhaler. Oral corticosteroids were needed by 35.8% of patients, and with respect to anti-IL-5 biologics, most patients were treated with benralizumab (47.2%). Inhaled and oral therapies to treat asthma are shown in table 2.
Inhaled and concomitant therapies
| Patients n = 53 | |
|---|---|
| Inhaled therapy | 53 (100.0) |
| LABA and corticosteroids combined | 53 (100.0) |
| LAMA | 40 (75.5) |
| SABA | 45 (84.9) |
| SAMA | 6 (11.3) |
| Oral corticosteroid treatment | 19 (35.8) |
| Deflazacort | 3/19 (15.8) |
| Methylprednisolone | 1/19 (5.3) |
| Prednisone | 15/19 (79.0) |
| Montelukast | 31 (58.5) |
| Biologic therapies | 53 (100.0) |
| Benralizumab | 25 (47.2) |
| Mepolizumab | 19 (35.8) |
| Reslizumab | 9 (17.0) |
Data expressed as numbers (percentages)
LABA: long-acting beta2-agonists; LAMA: long-acting muscarinic antagonists;
SABA: short-acting beta2-agonists; SAMA: short-acting muscarinic antagonists.
Combining both methods, 17.0% of patients were considered nonadherent, whereas 35.8% of patients were adherent. Nonadherence to the primary inhaler was detected in 58.5% of patients according to the PRD; however, this percentage only reached 22.6% when employing the TAI questionnaire. When identifying nonadherent patients by either of the 2 methods (PRD < 80% and TAI questionnaire < 50), 64.2% were recognised as having nonadherence to inhalers. Likewise, the two methods agreed in 53.1% and disagreed in 46.9% of cases, (k = 0.137; 95% CI –0.057 to 0.331; p = 0.318). All these results are shown in table 3.
Comparison between adherence measured by pharmacy refill data and test of adherence to inhalers questionnaire
| PRD nonadherence | PRD adherence | Kappa | p | |
|---|---|---|---|---|
| TAI nonadherence | 9 (17.0) | 3 (5.7) | 0.137 | 0.318 |
| TAI adherence | 22 (41.5) | 19 (35.8) |
Data expressed as numbers (percentages).
PRD: pharmacy refill data; TAI: Test of Adherence to Inhalers.
When analysing differences according to sex, we observed that women had slightly less adherence to inhalers than men, but without significant differences (for PRD 60% vs. 55%, respectively, p = 0.688; and for the TAI questionnaire 24.2% vs. 20.0%, respectively, p = 0.721). According to the patients’ comorbidities, the highest nonadherence to inhalers was detected in patients with rhinoconjunctivitis (54.8% and 50.0%, measured by PRD and the TAI questionnaire, respectively). Moreover, agreement of the two methods was low in all comorbidities (Table 4). Finally, nonadherence was higher in patients taking montelukast (54.8% for PRD and 50.0% for the TAI questionnaire).
Nonadherence to inhalers according to comorbidities and concomitant therapy
| Comorbidity under treatment | PRD nonadherence n = 31 | TAI nonadherence n = 12 | K (95%) |
|---|---|---|---|
| Comorbidity | 23 (74.2) | 9 (75.0) | 0.087 (− 0.144-0.318) |
| Rhinoconjunctivitis | 17 (54.8) | 6 (50.0) | 0.022 (− 0.256-0.300) |
| Nasal polyposis | 7 (22.6) | 5 (41.7) | −0.049 (− 0.421-0.519) |
| Gastroesophageal reflux | 3 (9.7) | 1 (8.3) | 0.364 (− 0.210-0.938) |
| Anxiety and depression | 10 (32.3) | 3 (25.0) | 0 (− 0.317-0.317) |
| AERD | 3 (9.7) | 2 (16.7) | −0.154 (− 0.659-0.967) |
| Concomitant therapy for asthma | |||
| Oral corticosteroid treatment | 10 (32.3) | 3 (25.0) | 0.086 (− 0.226-0.398) |
| Montelukast | 18 (54.8) | 7 (50.0) | 0.111 (− 0.148-0.369) |
Data expressed as numbers (percentages).
AERD: aspirin-exacerbated respiratory disease; PRD: pharmacy refill rate; TAI: Test of Adherence to Inhalers.
To our knowledge, this is the first study that analyses the degree of compliance using two methods, PRD and the TAI questionnaire, in patients diagnosed with severe asthma and treated with anti-IL-5 biologics. Our results show a higher percentage of nonadherent patients when combining both methods. Likewise, we have detected that PRD identify a higher percentage of nonadherent patients compared with the TAI questionnaire. Finally, the results of both methods are poorly correlated, a finding in line with the results reported by Plaza et al.9.
When treating asthma, it is important to use long-term control medications to achieve and maintain control of the disease, but it is also necessary that patients follow the recommendations provided. With respect to severe asthma, its treatment frequently requires polymedication; thus, deficient adherence increases the risk of poorer control of the disease, leading to more exacerbations and higher morbidity and mortality rates18,19. In developed countries, adherence to treatment in chronic diseases is approximately 50%20, and it tends to be lower in asthma, where it ranges from 22% to 78%6. In this context, we have found a high prevalence of nonadherence to inhalers in patients with severe asthma on therapy with anti-IL-5 biologics. Thus, we have identified a higher percentage of nonadherence (58.5%) compared with other studies2,9,21,22. One explanation could be that, given our population was included from a severe asthma unit and all of them were being treated with anti-IL-5 biologics, we were unable to find any research with the same study population with which to compare them. Thus, anti-IL-5 biologics, unlike inhalers, have the advantage of being administered monthly or bimonthly. Given that their use is associated with an important improvement in respiratory symptoms, patients have a higher risk of abandoning their treatment with inhalers and, as a consequence, of reducing their adherence to inhaled therapy. In fact, the multidisciplinary consensus Delphi study23 supports that improvement of symptoms in asthma predisposes patients to nonadherence because patients believe that treatment becomes unnecessary24. Various studies have shown a relationship between beliefs about asthma and adherence to preventive therapy, especially in those patients who consider that asthma is an episodic rather than a chronic disease, and that therapy is necessary only during exacerbations25.
Self-report questionnaires are commonly used to measure adherence due to their low cost, acceptable reliability and the short time required to complete them (less than 10 minutes for the TAI questionnaire)16,17. Thus, the TAI questionnaire was specifically designed for inhalers, and it also assesses the type of noncompliance16,17. On the other hand, PRD makes it possible to calculate adherence by comparing the prescription made through the electronic prescription system with the medication dispensed in pharmacies in a given period of time. Previous studies have reported that low nonadherence rates detected by the PRD are related to the low cost of inhalers in Spain (which has universal health care coverage)9. Nevertheless, our results highlight that nonadherence is higher when assessed by PRD than by TAI questionnaire. Furthermore, we suspect that this rate of nonadherence obtained when using PRD could even be underestimated, given that patients could continue getting inhalers from the pharmacy (adherence obtained from the PRD) without taking them (adherence obtained from the TAI questionnaire). In previous studies2,9, the TAI questionnaire identified more nonadherent patients than the PRD, whereas in our population it is the other way around. This difference could be explained by multiple factors. First, the use of anti-IL-5 biologics is associated with a considerable improvement of respiratory symptoms10–14; second, the belief that inhalers are necessary only during exacerbations25,26. Both factors contribute to nonadherence to inhalers and consequently nonwithdrawal at the pharmacy.
We have shown poorer agreement between methods. Llano et al.2, who also used the TAI questionnaire and PRD to estimate the adherence to inhalers in patients with asthma, but not in patients with severe asthma who are on anti-IL-5 biologics, reported a moderate agreement between methods. Nevertheless, Plaza et al.9 reported that these methods are poorly correlated, a finding consistent with our results (k = 0.137). This low correlation supports their concomitant use in clinical practice as is recommended by clinical guidelines6,7.
This study has potential strengths. First, as far as we know, this is the first study conducted in a population treated with biologics. Second, our results agree with previous studies9,27 and guidelines6,7 that support the concomitant use of two methods to evaluate adherence in asthma. We show that this recommendation could be extended to patients with severe asthma treated with anti-IL-5 biologics. Third, although it might appear that our sample is small in relative terms, we have included a larger number of patients than previous studies2,9, given that severe asthma affects approximately 4%28,29 of the population worldwide, and not all of them use biologics. Even though lung function test results were not analysed, they were not necessary for our objective.
As limitations of the study, we consider first that none of the methods used to assess adherence is considered the gold standard. Another limitation of our study is the design, as it is retrospective, monocentric and lacks of a control group (not treated with anti-IL-5 biologics). Although we have included comorbidities as a variable in our study, because they also affect adherence to medications, other factors might also be involved in adherence to inhalers and have not been considered such as age group, number of medications, duration of asthma, health literacy or number of exacerbations.
In conclusion, our results highlight the high prevalence of nonadherence to inhalers in severe asthma treated with biologics. Also, the agreement between indirect methods that evaluate adherence is low; therefore, it is plausible to use them concurrently in clinical practice1.
FundingNo funding.
Conflict of interestsNo conflict of interests.
Contribution to the scientific literature
Many studies have attempted to measure the prevalence of nonadherence in asthma, but none of them have focused on patients with severe asthma treated with biologics. Our results highlight the high prevalence of non-adherence to inhalers in this population, as it was observed in almost 65% of patients.
In previous studies, the Test of Adherence to Inhalers questionnaire identified more non-adherent patients than pharmacy refill data whereas in our population it is the other way around. This may be explained firstly by the fact that the use of anti-interleukin-5 biologics is associated with considerable improvement of respiratory symptoms and secondly by the belief that inhalers are necessary only during exacerbations.
Inadequate adherence represents a public health problem. Our study exposes, firstly, the possible causes of non-adherence to inhalers in patients with severe asthma treated with biologics and secondly, compares and discloses the limitations of indirect methods available to identify and quantify this non-adherence in order to focus efforts on targeted and individualised multidisciplinary interventions to identify and quantify non-adherence in order to remove barriers to patient compliance.
Early Access date (05/19/2022).