To estimate the prevalence of medication-related problems in patients treated in continuous care units and to identify the therapeutic areas in which these problems were more concentrated.
MethodObservational descriptive prospective study. Review of clinical histories and outpatient treatment by a hospital pharmacist. Communicating medication-related problems detected to the responsible doctor. Analysis of the therapeutic areas in which the problems were most concentrated.
Results85 patients were reviewed, and 368 potential medication-related problems were identified. The areas with the most prevalent medication-related problems were the long-term use of hypnotics, sub-optimal analgesia, optimizable antidepressant treatment, statins in patients older than 75 years in primary prevention and in those with high-intensity doses in secondary prevention, patients with heart failure without angiotensin-converting enzyme inhibitors, and proton-pump inhibitors without indication.
ConclusionsTraining interventions should be implemented and computer assistance should be developed to help avoid the most prevalent medication-related problems.
Estimar la prevalencia de problemas relacionados con la medicación en los pacientes atendidos en la consulta de la unidad de continuidad asistencial e identificar las áreas terapéuticas donde se concentran.
MétodoEstudio observacional descriptivo y prospectivo. Revisión de la historia clínica y el tratamiento domiciliario por un farmacéutico hospitalario y comunicación al médico de los problemas relacionados con la medicación detectados. Análisis de las áreas terapéuticas donde se concentran.
ResultadosSe revisaron 85 pacientes, identificando 368 potenciales problemas relacionados con la medicación. Las áreas más prevalentes fueron el uso crónico de hipnóticos, la analgesia subóptima, el tratamiento antidepresivo optimizable, estatinas en mayores de 75 años en prevención primaria y con dosis altas en prevención secundaria, pacientes con insuficiencia cardiaca sin inhibidores de la enzima convertidora de angiotensina e inhibidores de la bomba de protones sin indicación.
ConclusionesSe deberían realizar intervenciones formativas y desarrollar asistencias informáticas que ayuden a evitar los problemas más prevalentes relacionados con la medicación.
Chronic diseases are the main cause of mortality and disability in developed countries. To adapt the healthcare model to this situation, the Autonomous Community of Castile and León (Spain) has designed a strategy for the care of chronic patients1 by creating Continuous Care Units (CCU) in hospitals, with a specialist in Internal Medicine acting as an intermediary and consultant for Primary Care physicians (PCP).
One of the main challenges in the management of chronic patients is related to pharmacotherapy: There is a lack of evidence due to the exclusion of these types of patients from clinical trials, clinical practice guidelines address the management of a single disease2, and this group of patients is particularly frail. In recent years, different methods have emerged to adapt treatments to these patients3,4, but their implementation in daily clinical practice is difficult. Depending on the care setting under study and the tool used for assessment, the prevalence of medication-related problems (MRPs) ranges from 22% to 33% in Spain5,6.
This study estimated the prevalence of MRPs in complex chronic patients (CCP) treated in the CCU, and identified the therapeutic areas with the highest concentration of MRPs and the greatest margin for improvement.
MethodsObservational descriptive prospective study of the prevalence of MRPs in CCP treated in the CCU from June to December 2016. To fulfil one of the objectives of the yearly management plan of the Autonomous Community, the work methodology was consensually designed at a joint meeting of the medical management of the hospital, the internists from the CCU, and the pharmacy service. The study included all the outpatients with electronic prescriptions to ensure that a complete and updated list of the home treatment of each study participant was available. A hospital pharmacist reviewed the electronic medical record of each patient, both from primary care (Medora®) and specialized care (SiClínica®), and systematically checked the following treatment-related items:
- 1.
Current indication, validated and registered in the medical record.
- 2.
Evidence related to the drug (reviewed in UpToDate, Cochrane, Trip Database, and using the Beers3 and Stopp-Start4 criteria).
- 3.
Absence of duplication.
- 4.
Absence of interactions with other drugs or with preexisting pathologies.
- 5.
Appropriate dosage: optimal schedule and adjustment to renal function, weight, and age.
- 6.
Patient follow-up and periodic monitoring needed.
- 7.
Selection of the safest, most effective, and cheapest drug.
- 8.
Absence of unaddressed indications.
Based on the type of negative results associated with medication (NRMs), the MRPs detected were classified into: need, safety, and effectiveness7.
A list of the MRPs detected and their proposed solutions were sent by e-mail to the physician responsible for the CCU the day before the appointment with the patient. The physician assessed the solutions proposed for these MRPS and decided if they were applicable or not. If the solutions were accepted, they were registered in the patients’ electronic medical record. If the physician rejected the solution or considered that it should be assessed by the PCP, the pharmacist was contacted by telephone.
ResultsIn total, 85 complex patients with electronic prescriptions were treated in the CCU during the study period. Mean age was 83.7 years (range = 61-98) and 53.7% of the participants were women. A total of 1125 treatment lines were reviewed (= 13.2 lines/patient, standard deviation = 3.97). We identified 368 potential MRPs (median = 4 MRPs/patient; interquartile range = 3-6), entailing a prevalence of 32.7 MRPs/100 treatment lines.
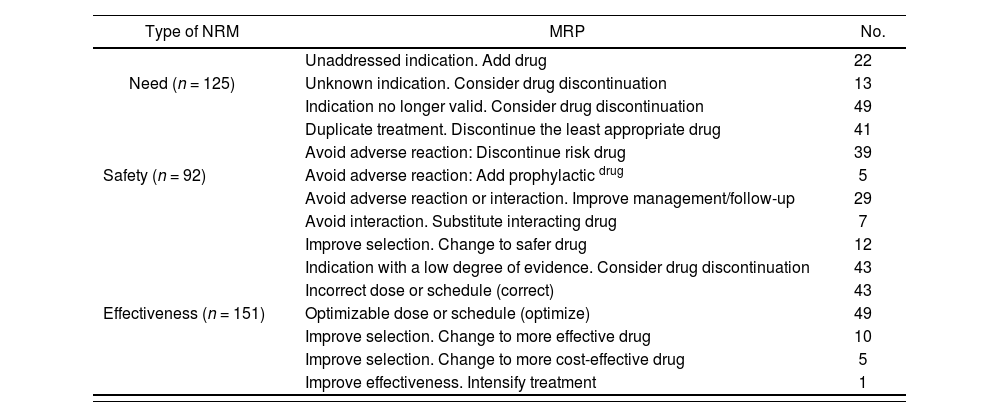
Table 1 shows the MRPs detected, which were classified as follows: need NRMs = 125/368 (34%); safety NRMs = 92/368 (25%); and effectiveness NRMs = 151/368 (41%).
Detected medication-related problem and negative results associated with medication
| Type of NRM | MRP | No. |
|---|---|---|
| Unaddressed indication. Add drug | 22 | |
| Need (n = 125) | Unknown indication. Consider drug discontinuation | 13 |
| Indication no longer valid. Consider drug discontinuation | 49 | |
| Duplicate treatment. Discontinue the least appropriate drug | 41 | |
| Avoid adverse reaction: Discontinue risk drug | 39 | |
| Safety (n = 92) | Avoid adverse reaction: Add prophylactic drug | 5 |
| Avoid adverse reaction or interaction. Improve management/follow-up | 29 | |
| Avoid interaction. Substitute interacting drug | 7 | |
| Improve selection. Change to safer drug | 12 | |
| Indication with a low degree of evidence. Consider drug discontinuation | 43 | |
| Incorrect dose or schedule (correct) | 43 | |
| Effectiveness (n = 151) | Optimizable dose or schedule (optimize) | 49 |
| Improve selection. Change to more effective drug | 10 | |
| Improve selection. Change to more cost-effective drug | 5 | |
| Improve effectiveness. Intensify treatment | 1 |
MRP: medicalion-relaled problem; NRM: negative results associated with medication.
Regarding the pharmacist's recommendations, 35.3% were accepted by the physician responsible for the CCU, while the remaining 64.7% were deemed to require assessment by the PCP. None of the solutions were rejected. In total, 105 of the proposed solutions were not assessed for the following reasons: 45 e-mails were not read because of lack of time; 25 solutions were not assessed due to software problems; 24 were not assessed because the patient did not attend the appointment; and 11 were not assessed because the patient died.
The most prevalent problems were found in the following therapeutic areas:
- 1.
Long-term use of hypnotics (23.5%).
- 2.
Sub-optimal analgesia (23.5%).
- 3.
Optimizable antidepressant treatment (14.1%).
- 4.
Use of statins in patients over 75 years in primary prevention (9.4%) and with high-intensity doses in secondary prevention (4.7%).
- 5.
Patients diagnosed with heart failure not treated with angiotensin-converting enzyme inhibitors (ACEIs) (10.6%).
- 6.
Use of proton-pump inhibitors (PPIs) without valid indication (8.2%).
The prevalence of MRPs (32.7%) in this study was similar to that described in previous studies5,6; however, the patients are not fully comparable because both the average age of the participants and the number of drugs prescribed were higher in our study. We found that the long-term use of hypnotics and inappropriate use of PPIs were two of the therapeutic areas associated with more MRPs, which is line with the findings of previous studies5,6. However, we also identified other therapeutic areas with large numbers of MRPs; thus, further research is warranted.
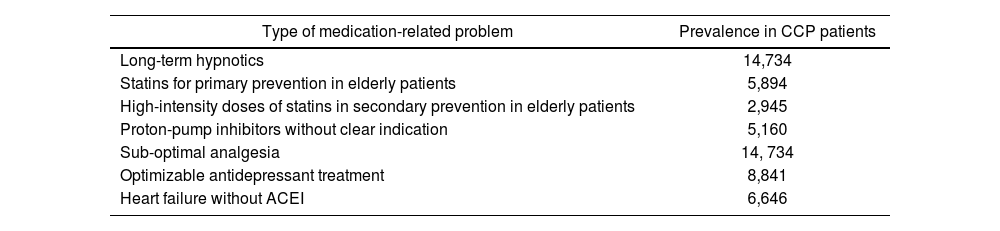
To better understand the magnitude of these results, we extrapolated them to the 62,700 CCP in the Autonomous Community of Castile and León (see Table 2). Thus, 14,734 patients would have prescriptions for the long-term use of hypnotics for chronic insomnia, with the consequent risk of falls, confusion, and excessive daytime sleepiness8; 14,734 patients would have the opportunity for improved analgesic treatment; 8,841 would have an inappropriate prescription for antidepressant drugs (e.g. caused by not taking into account their potential for interactions with comorbidities or concomitant drugs); 5,894 patients over 75 years would be treated with statins in primary prevention and 2,945 patients over 75 years would be treated with high-intensity doses in secondary prevention: statins have not been shown to have any benefits in these situations, but have been shown to increase the risk of myopathy, diabetes, and cognitive abnormalities9; 6,646 patients with congestive heart failure and LVEF < 40% would not have been treated with ACEIs, although they have been shown to reduce morbidity and mortality10; and 5,141 patients would have been treated with
Most prevalent medication-related problems extrapolated to all CCP patients in the Autonomous Community of Castile and León (Spain)
| Type of medication-related problem | Prevalence in CCP patients |
|---|---|
| Long-term hypnotics | 14,734 |
| Statins for primary prevention in elderly patients | 5,894 |
| High-intensity doses of statins in secondary prevention in elderly patients | 2,945 |
| Proton-pump inhibitors without clear indication | 5,160 |
| Sub-optimal analgesia | 14, 734 |
| Optimizable antidepressant treatment | 8,841 |
| Heart failure without ACEI | 6,646 |
ACEI: angiotensinxconverting enzyme inhibitor.
PPIs without indications, which would have increased the risk of pneumonia, overinfection by Clostridium difficile, and vitamin B12, iron, and calcium deficiencies11.
One of the limitations of this study is that only 45% of the patients treated in the CCU had an electronic prescription, which may have biased the results. Moreover, the CCU physician considered that most of the recommendations (64.7%) required assessment by the PCP; however, the number of recommendations that were accepted remains unknown. Given our results and those described in previous studies12, we recommend the creation of multidisciplinary teams comprising all the professionals involved in the different levels of care in the treatment of CCP, and also recommend the development of training interventions and computer assistance to help avoid the most prevalent MRPs.
FundingNo funding.
Conflict of interestsNo conflict of interests.
Contribution to scientific literature.
This study tries to identify the main problems related to medication (MPRs) in CCP. Although in recent years different methods have emerged for the adequacy of treatment in this type of patients, its application in daily clinical practice is very complicated. Identifying the main problems related to medication (PRMs) in these patients, training interventions and computer assistance could be developed, facilitating the management of pharmacotherapy in CCP.