The document “Guide to Excellence in the Conduct of Clinical Trials in Hospital Pharmacy” was drawn up by hospital pharmacists and representatives of the pharmaceutical industry. Its objective is “to unite criteria, introduce improvements in communication, harmonize and digitalize processes” in all phases of development of a clinical trial in Hospital Pharmacy Services.
This special article includes the reflections of the Working Group of the Spanish Society of Hospital Pharmacy about this document. The analysis is based on its participation in the drawing of the Guide of Excellence, and includes its most relevant aspects, including those which, despite being discussed during the process of preparing the document, were finally not included, for reasons of synthesis or for further analysis and agreement.
While recognizing the undoubted value of a so far unprecedented first document of consensus, the Clinical Trials Working Group also highlights the future challenges that both hospital pharmacists and pharmaceutical companies have ahead in order to improve the quality of the management of clinical trials.
The Clinical Trials Working Group believes that the existence of communication routes both with the pharmaceutical industry and other agents involved in the conducting of clinical trials, as well as the improved visibility of the hospital pharmacist as an expert in the management of investigational medicines, will help achieve a better management of clinical trials in our environment and the assignment of the necessary human and material resources to reach excellence.
El documento “Guía de Excelencia para la Realización de Ensayos Clínicos en Farmacia Hospitalaria” ha sido elaborado por farmacéuticos de hospital y representantes de la Industria Farmacéutica. Su objetivo es “aunar criterios, introducir mejoras en la comunicación, armonizar y digitalizar procesos” en todas las fases de desarrollo de un ensayo clínico en los Servicios de Farmacia Hospitalaria.
El presente artículo especial recoge las reflexiones del Grupo de Trabajo de Ensayos Clínicos de la Sociedad Española de Farmacia Hospitalaria acerca del documento. El análisis se basa en su participación en la elaboración de la Guía de Excelencia, y recoge los aspectos más relevantes de la misma, haciendo referencia también a algunos puntos que, pese a ser motivo de discusión durante el proceso de elaboración del documento, finalmente no se incluyeron, por motivos de síntesis o para un posterior desarrollo y acuerdo.
Reconociendo el indudable valor de un primer documento de consenso inédito hasta el momento, desde el Grupo de Trabajo de Ensayos Clínicos se ponen de manifiesto también algunos retos de futuro en la gestión de los ensayos clínicos que se presentan para ambos colectivos, Farmacia Hospitalaria e Industria Farmacéutica.
En opinión del Grupo de Trabajo, la apertura de vías de comunicación, tanto con la Industria Farmacéutica, como con otros agentes implicados en la realización de ensayos clínicos, y el consecuente aumento de la visibilidad del farmacéutico de hospital como experto en el manejo del medicamento en investigación, ayudará a mejorar la calidad de la gestión de la medicación de ensayos clínicos en nuestro entorno, así como la asignación de los recursos humanos y materiales necesarios para alcanzar la excelencia.
Clinical trials (CTs) are considered the cornerstone of clinical research into drugs.1 According to recent data published by the Spanish pharmaceutical industry association (Farmaindustria), Spain is one of the most prolific European Union countries in terms of performance of CTs,2 with a steady growth in the number of CTs carried out every year.
Although Good Clinical Practice (GCP) guidelines3 entrust principal investigators with the responsibility of managing investigational medicinal products (IMPs), the current Spanish legislation delegates drug reception, custody and dispensing functions to hospital pharmacy departments (HPDs).4
The responsibility of managing a growing number of CTs, some of them highly complex and requiring individualized and specific storage, handing and management has created a situation where the clinical trial units (CTUs) of HPDs are faced with an increasing demand of material resources and specialized staff.
At the same time, the excessive bureaucratization of the processes related with the conduct of CTs together with the need to adapt to the specific requirements and procedures of different CT sponsors also constitute a formidable challenge for HPDs, as it is often the case that the scarce resources available must be assigned to procedures that not only lack any added value but also jeopardize the safety of patients and of the professionals involved in managing IMPs.
From the standpoint of the pharmaceutical industry (PhI), IMP management optimization is construed as a way of enhancing the eligibility of a country, in this case Spain, to host CTs, which has for many sponsors been an important priority since the implementation of the EU Clinical Trials Regulation.5
Against this background, the Clinical Trials Working Group (GTEC) of the Spanish Society of Hospital Pharmacists (SEFH) considers it essential to establish communication channels with the PhI, insofar as it is pharmaceutical companies that sponsor most of the CTs performed in Spain. The final goal would be to come up with a consensus regarding the procedures to be followed and the criteria to be applied, optimize processes involved in the management of investigational medicines, and increase the quality of such management processes, eliminating superfluous tasks.
Phases of the projectThe Guide to Excellence for the Conduct of Clinical Trials in Hospital Pharmacies6 resulted from an initiative of Farmaindustria and the Hospital Affairs Section of the General Council of Pharmacist Associations, further to a multidisciplinary meeting held in July 2019 where a document called Decálogo de Criterios de Excelencia para la realización de Ensayos Clínicos (Ten standards for the conduct of high-quality clinical trials) was drafted.7 One of the standards in this document made reference to the importance that HPDs be involved in the performance of CTs.
After an initial meeting in November 2020, attended by PhI representatives and hospital pharmacists, including several members of GTEC, a list was drawn up of the issues which, in the participants' opinion, required urgent action with respect to the relationship between the PhI and HPDs. The document was divided into six problem areas, each assigned to a joint working group made up of members of the PhI and of the hospital pharmacy community. The six working groups created were required to work on the following areas:
- •
Communication
- •
Document harmonization and standardized working procedures
- •
Platform standardization
- •
Process improvement
- •
Comparator drug supplies
- •
Process digitalization
The working groups presented their conclusions in March 2021 and, after that, a joint drafting committee (DC) was created to work on preparing a final document. The DC decided that the document be structured in guideline form as this would not only make it intuitive and didactic, but it would also make it a flexible document capable of accurately conveying the conclusions of the different working groups.
Further to a series of consensus meetings of the DC, the document was finally released to the public in April 2022.
The GuideThe DC decided that the most didactic way to structure the Guide would be to follow the typical chronological order of a CT, dividing the document into three sections: 1) pre-study phase, 2) initiation phase, and 3) execution and closure. Each of these stages was developed from different points of view, adapting the initial thematic distribution to a simpler and clearer structure. Each section was structured around the following themes:
- 1.
Communication.
- 2.
Documents and processes.
- 3.
Investigational drug.
- 4.
Platforms, systems and digitalization.
Four support infographics were also included to assist readers in the preparation of the different documents and the implementation of the different processes.
In what follows a detailed description is provided of the most significant aspects under each of the themes from which the three development phases of a CT were analyzed. Reference is made both to the points included in the Guide and to those which, although discussed by the working groups, were finally excluded from the Guide for reasons of brevity or because it was decided to leave them for future development and discussion.
CommunicationCommunication between sponsors, investigational teams and HPDs is essential for the effective and high-quality management of CTs and IMPs. It also has an unquestionably beneficial effect from the very early stages on all parties involved, particularly in the case of CTs with more complex management of IMPs. Moreover, once the CT is underway, specific communication channels must be established between sponsors and HPDs, avoiding redundant and unnecessary information but, at the same time, ensuring effective communication and the ability to resolve any issues related to the management of IMPs (changes in drug compounding and conservation, new dosage forms, initiation or discontinuation of treatment arms in CTs, adaptive designs, etc.).
Hospital pharmacists are equipped with the necessary training and experience to manage and handle complex and innovative IMPs. Sponsors and clinical monitors must interact with hospital pharmacists in an individualized way, different from the way in which they relate to other members of the investigational team, on account of the highly specialized, variable and intensive roles played by hospital pharmacists in the conduct of a CT.
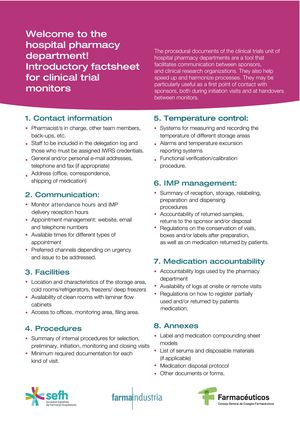
An important aspect that should be taken into consideration is the constant turnover of staff that characterizes HPDs and monitoring teams. This issue stands in the way of effective communication between the sponsor of the CT and the HPD. Availability at the HPD's CTU of welcome leaflets with basic information on procedures and contact data greatly facilitates HPD selection and CT implementation.
Table 1 shows different proposals aimed at improving communication between sponsors and HPD members before and during the performance of a clinical trial.
Communication between sponsors and HPDs.
| Proposals for improvement for HPDs | |
|---|---|
| Pre-study phase/ initiation phase of the CT | Availability of initiation factsheets with basic information on the operation of the HPD and contact details. |
| Availability of checklists aimed to facilitate the preparation of initiation visits so as to focus the information on aspects relevant to the management of IMPs. | |
| Establishing communication channels with research foundations or legal departments in charge of determining eligibility of hospitals and prepare contracts, aimed at ensuring that HPDs receive all the relevant information for the performance of CTs. | |
| Establishing a system that makes it possible to conduct a preliminary evaluation of the protocol and, if appropriate, establish a cost to be charged for the HPD activities. | |
| During the development of the CT | Implementing contingency plans for issues related with custody of investigational medicines (alarms warning of out of range temperatures or stock-outs) or other aspects of drug management. |
| Establishing communication channels with the research team, particularly when special medicines must be compounded or unusual procedures must be followed. | |
| Proposals for improvement for sponsors | |
| Preliminary phase/ initial phase of the CT | Informing HPDs of the nature of their participation in the CT and providing them with all relevantinformation available on the IMP, particularly in cases of new therapies or those involving a complex compounding process. |
| Informing HPDs about the channels to be used to supply all investigational and auxiliary medicinal products in order to achieve a consensus on alternatives should it not be possible for the sponsor to supply comparator or auxiliary medicinal products. | |
| Preparing a report that includes the CT management plan that should be shared with all parties involved at the different phases of development. | |
| During the development of the CT | Updates and new documents: only information affecting HPD procedures should be sent. Documents should have the track changes function enabled or contain a summary that allows fast identification of differences with respect to the previous version. |
| Establishing a fast and effective system to manage temperature excursions, avoiding excessive red tape. | |
| Preparing individualized follow-up reports addressed to HPDs after each monitoring visit. These reports should include the findings made, the actions undertaken and the agreements concluded. | |
HPD: Hospital pharmacy department.
Finally, it is considered good practice for monitors to send an e-mail or a follow-up note to HPDs after the pre-study and initiation visits with the HPD stating the agreements concluded between the HPD staff and the CT sponsor, as well as all actions required for implementation of the CT. The principal investigator should be included in all follow-up reports, with all agreements made duly recorded lest the staff involved changes during performance of the study.
Documents and processesGCP guidelines3 describe the documents to be included in the investigator site file, while the CT is underway and once it has been completed. However, it is not clear nor there is general agreement on the contents or the format of a CT's pharmacy file.
HPDs with a high volume of CTs should be able to avail themselves of a practical, safe and efficient way of managing all the documents generated. At the same time, standards should be developed regarding minimum documentation requirements and the format in which documents must be stored, which not be accepted by all sponsors.
The Guide stipulates the minimum set of documents to be delivered by the sponsor to the HPD and lays emphasis on the importance that the HPD should make available a welcome leaflet with basic information on the way the CTU operates as well as a checklist of the different topics to be discussed during the initiation visit.
Table 2 shows a proposal of the minimum set of documents to be included in the pharmacy file of a CT at the pre-study, initiation and development phases.
Proposed contents of pharmacy records in the context of clinical trials (physical and/or digital records).
| Pre-study /initiation phase of the clinical trial | Protocol | Current version at the time of the initial visit. |
| Pharmacy handbook | The HPD must be handled a written record of all the required information and/or materials related to the IMP:- Storage conditions.- Preparation conditions (if appropriate).- Administration conditions.- Label and package type model, allowing HPDs to decide how much storage space is necessary. | |
| Safety Data Sheet or its equivalent | Document providing information on the safety conditions required for handling of the IMP. | |
| Legal documents | Regulatory Agency (AEMPS) approvalFavorable opinion by the Ethics CommitteeSite Agreement | |
| HPD documents | Resumés and GCP training certificates of the HPD staff in charge. | |
| Internal delegation document: A record must be kept of the staff involved in managing the investigational drug (preparation, dispensing etc.) who are not included in the CT's task delegation form. | ||
| Valid calibration certificates for the temperature probes used in the storage facility. | ||
| In the course of the clinical trial | Updating of reference documents | Changes to the protocol, the pharmacymanual or other documentswhich may affect the procedures of the HPD. |
| Source documents and registries | Source documents (in physical or digital format) related to reception/dispensing-preparation/return of IMPs. | |
| IMP accountability forms (in physical or digital format). | ||
| Temperature records |
GCP: Good clinical practice; AEMPS: Spanish Agency of Medicines and Medical Products; CEIM: Ethics Committee for Drugs Research; HPD: hospital pharmacy department.
As regards the information factsheet to be made available by the HPD, infographic 1 of the Guide (Fig. 1) contains a proposal of the minimum items of information it should include: contact data, opening hours, description of the facilities and work procedures.
During the CT initiation visit, all agreements regarding the handling of the IMP and the responsibilities of the HPD staff must be concluded. The initiationvisit should not be a replica of the initiationvisit with the research team, attendance of the monitor assigned to the HPD is required, and its duration and contents must beadapted to the CT's complexity.
Infographic 2 of the Guide includes the aspects and documentation that should ideally be shared with monitors during their initiation visit to the HPD (Fig. 2).
One of the chief milestones achieved has been the acceptance by CT sponsors of the individual hospitals' specific accountability logs provided that they contain the minimum items of information required by the GCP guidelines. Infographic 3 of the Guide (Fig. 3) contains the minimum set of information to be included in an accountability log.
Investigational medicinesIn accordance with the current legislation,8 sponsors are responsible for supplying all IMPs both for the experimental and the control arms free of charge. They must also ensure the medications' proper manufacturing, packaging and labeling. They shall also be responsible for the preservation of the samples and their manufacturing and control protocols, recording the samples delivered, and ensuring that the venue where the trial is conducted possesses a protocol that guarantees appropriate sample management and conservation.
With regard to the supply of IMPs, the Royal Decree on Clinical Trials8 contemplates the possibility for alternative supply routes to be established by CT sponsors when it is not feasible to supply a hospital with all IMPs packaged and labeled exclusively for a specific CT. Although this exception was initially intended for non-commercial CTs, sponsors often invoke it in cases where the comparator arm includes already approved medicines or medicine combinations, which are also the standard of care for the disease under analysis. In these cases, sponsors usually suggest that the HPD administer the medication in advance, undertaking to reimburse the cost incurred at a later date.
As mentioned in a position paper published by GTEC,9 this practice involves several practical and legal issues, with some hospitals being unable to use the reimbursed amount to defray the cost of the medication.
The Guide contemplates different alternatives for supplying comparator medicines, which can be summarized as follows:
- -
Option 1: Direct reimbursement of the medicines' cost to the hospital, taking into account the considerations made in SEFH's relevant position statement.9
- -
Option 2: Advance purchase of the medicines by the HPD, which subsequently bills the sponsor for the amount spent.
- -
Option 3: Advanced purchase of the medicines by the sponsor from third parties (wholesalers authorized to handle IMPs).
- -
Option 4: The sponsor restores the used medicines to the hospital's stock.
In addition to the supply of comparator medicines, the working groups discussed other important subjects, including ways to increase quality in the management of IMPs and improve the safety of patients and the staff in charge of handling the medications. The subjects discussed, not all of which included in the final version of the Guide, were as follows:
- -
Quantity and quality of the information included in the medication delivery notes.
- -
Adaptation of the IMP dosage forms to the real doses required.
- -
Recommendations for the management of potentially hazardous medicines, including counting the tablets of oral medication returned by patients and discarding empty or partially used vials following preparation by the HPD.
- -
Home delivery of medicines.
- -
Delivery of medicines with reasonable expiry periods and relabeling of expired samples.
The 2020 pandemic gave a significant boost to the development of digital tools allowing two-way communication and the exchange of data between sponsors and hospitals, while ensuring continuity and integrity of CT data.10 Massive application of remote data digitalization and monitoring has made it possible to identify the advantages, disadvantages and limitations or the hitherto available tools.
HPDs believe that, given the difficulties inherent in working across different platforms when managing multiple CTs, the use of single platforms and single sign-in systems where the same credentials can be employed to access different platforms should be promoted insofar as possible. Another demand of HPDs is that corporate access tools, with single credentials for the entire HPD staff, may be allowed for the most commonly-used platforms, such as interactive web response systems (IWRS's). This can obviously be possible only in cases where the CTU's documents allow internal traceability to the person executing a given interaction.
For cases where monitoring is conducted remotely, a series of tools have been proposed for remote visits to be conducted successfully (teleconferencing apps, online software or repositories allowing monitors remote access to the HPD's records). At the same time, it is important to define what activities monitors may perform remotely and which they must obligatorily perform onsite (e.g., collection of signatures [until electronic signatures are universally accepted in GCP audits], reviewing of non-digital source information, drug reconciliation by monitors and relabeling due to batch expiry or other causes).
DiscussionSeveral organizations, among them SEFH, have published quality guidelines and procedural recommendations for the proper management of IMPs at HPDs.10–14 Nonetheless, to the best of our knowledge, none of them are the result of a consensus with pharmaceutical companies, which tend to be the sponsors of CTs. The value of the Guide discussed in this study is precisely that it is the result of a joint effort between pharmacists and the PhI and that it paves the way for further collaboration between sponsors and HPDs.
New developments such as digitalization of documents and processes, decentralization of CTs, the use of telepharmacy in the context of CT, the development of CTs on advanced therapies and more effective management of hazardous drugs, among others, may no doubt benefit from close communication and collaboration with the PhI. However, GTEC believes that much work remains to be done to speed up processes, reduce red tape and eliminate activities which not only contribute no added value but also interfere with the quality of IMP management, undermining the safety of both patients and those handling IMPs.
Some examples include deficiencies in the labeling and the appropriateness of the IMP dosage forms, restrictions to the use of closed drug transfer systems, the problems inherent in long-term storage at HPDs of potentially hazardous leftover IMPs, and duplicate accounting of IMPs.
In this regard, GTEC is currently working hand in hand with principal investigator representatives and CT coordinators, monitors and sponsors on the preparation of a do's and don'ts document aimed at improving the quality and efficiency of HPD's CTUs.
It would be of the essence for collaboration between HPDs and the PhI to continue in the future, in the form of permanent or temporary working groups or one-off projects such as the one discussed in this study. Other parties, such as regulatory authorities and CT coordinator groups, should also be involved in any joint initiatives undertaken so as to discuss, and agree on issues of common interest.
Lastly, HPD should be equipped with the staff, infrastructure and resources required to achieve the standards of excellence needed in a continuously-evolving environment such as that of the conduct of CTs. Investments made in the HPD's CTUs will also be a great boon for hospitals themselves as they will no doubt benefit from the innovations introduced, the knowledge generated, and the potential investments attracted, as well as from an increase in their ability to develop their own high-quality investigations. HPD's CTUs will only be able to train their staff to the desired standard and attract the resources needed to face the challenges of the future if they enjoy the support of hospital and foundation managers and if they secure the support of hospital pharmacists, raising their awareness about the importance of excellence.
ConclusionsThe Guide to Excellence for the Conduct of Clinical Trials in Hospital Pharmacies is the first consensus document developed by the PhI and the hospital pharmacy profession for the management of IMPs.
The establishment of an open dialog between hospital pharmacists and the PhI and other agents involved in the conduct of CTs facilitates an effective approach to the different issues contemplated in the Guide, and makes it possible to address other present and future challenges to improve the efficiency and quality of managing the medications used in CTs in our country.
The leadership of hospital pharmacists as experts in the management of IMPs should be used as a tool to increase their visibility and make it possible for HPDs to be assigned the human and material resources they need to pursue excellence.
Authorship statementBelow is a list of the contributing authors, who have read and approved the final version of the article and have agreed for it to be submitted to the Revista. Next to each author's name and ID# is a description of the specific tasks they carried out.
Pilar Suñé Martín, ID# 43686923X: definition of the intellectual content, design, analysis and coordination of the project and writing of the manuscript. José Manuel Carretero-Abascal, ID# 28455136 L: definition of the intellectual content, design, analysis and interpretation of the project and final review of the manuscript with significant contribution. Cristina González-Pérez, ID# 47.033.105-Z: design, analysis and interpretation of the project and final review of the manuscript with significant contributions.
FundingThis project received no external funding.
The authors would like to thank Ana Herranz Alonso (Hospitals Chapter of the Spanish Pharmaceutical Council), Amelia Martín Uranga and Emili Esteve (Farmaindustria) for their encouragement and for their assistance in coordinating the preparation of the Guide, and
the pharmaceutical industry and hospital pharmacy representatives who contributed to the Guide.
Annex 1 (Coordinating Committee of the Clinical Trials Working Group of the Spanish Society of Hospital Pharmacists): María Serrano Alonso. María del Puy Goyache Goñi, Begoña Gómez Pérez, Concepción Martínez Nieto, Anna María Ferrer Artola, Marta Mullera Martí, Garbiñe Lizeaga Cundín, Ferran Capdevila Bastons, Ángela Villalba Moreno, Mireya Fernández Sánchez, Monike de Miguel Gascón