A study about the adherence of the antimicrobial prescriptions to the local guidelines of treatment of infections was conducted in a hospital emergency department to study the clinical and epidemiological characteristics of the patients who received these treatments. Conducting a feasibility study for supporting the design and execution of future studies, addressing specific aspects of the appropriateness of the antimicrobial prescription.
MethodObservational, descriptive and cross-sectional pilot study, with retrospective data collection about the antimicrobial prescription in a hospital emergency department. Seven cross sections were made, corresponding to seven different days of the week, in seven consecutive weeks. Inclusion criteria: patient over 14 years of age, with at least one first dose of antimicrobial treatment prescribed on the day of recruitment. The main variable was the inappropriate antimicrobial prescription according to the local guidelines. Epidemiological and clinical parameters of the patients were collected as secondary variables. In order to determine inappropriate prescription a revision was carried out by two specialists in emergencies, two pharmacists and one specialist in infectious diseases, all unrelated to prescriptions.
Results168 patients with 192 prescriptions were evaluated. Seventy-six (39.6%) of the prescriptions were not conformed to the local treatment guidelines. Of these, 55% were with active antimicrobial coverage against the microorganism but not recommended, 23.5% with inactive drugs, 13.7% presented an inappropriate dose and 7.8% were unnecessary treatment. The strength of agreement in the evaluation of the adequacy of treatment between doctors and pharmacists was high (kappa = 0.71).
ConclusionsA high rate of inappropriate antimicrobial prescriptions was obtained in a hospital emergency department according to local guidelines. The hospital pharmacist has an opportunity to improve the use of antimicrobials in this area.
describir la adecuación de las prescripciones de antimicrobianos a las guías de tratamiento locales de infecciones, en el área de urgencias hospitalarias, así como conocer las características clínicas y epidemiológicas de los pacientes que reciben dichos tratamientos. Llevar a cabo un estudio de viabilidad para el diseño y ejecución de investigaciones que aborden aspectos específicos de la inadecuación de prescripción de antimicrobianos.
Métodoestudio piloto observacional, descriptivo y transversal, con recogida de datos retrospectiva de prescripción de antimicrobianos en un servicio de urgencias hospitalario. Se realizaron 7 cortes transversales, correspondientes a los 7 días diferentes de la semana, en 7 semanas consecutivas. Criterios de inclusión: paciente mayor de 14 años de edad, con al menos una primera dosis de tratamiento antimicrobiano prescrita el día del estudio. La variable principal fue la prescripción de antimicrobianos inadecuada según las guías locales. Como variables secundarias se recogieron parámetros epidemiológicos y clínicos de los pacientes. La evaluación de la adecuación la realizaron 2 especialistas médicos de urgencias y 2 especialistas en farmacia hospitalaria, más un tercer evaluador, especialista en enfermedades infecciosas, todos ajenos a la prescripción.
Resultadosse evaluaron 168 pacientes con 192 prescripciones. Setenta y seis (39,6%) de las prescripciones no se ajustaron a las guías de tratamiento locales. De estas, el 55% fueron con cobertura antimicrobiana activa frente al microorganismo pero no recomendada, el 23,5% con fármacos inactivos, el 13,7% presentaban una dosis inapropiada y el 7,8% eran tratamientos innecesarios. La fuerza de la concordancia en la evaluación de la adecuación del tratamiento entre médicos y farmacéuticos fue alta (kappa = 0,71).
ConclusionesSe obtuvo una alta tasa de prescripciones de antimicrobianos inadecuadas en un servicio de urgencias hospitalario, según las guías locales. El farmacéutico de hospital tiene una oportunidad para mejorar el uso de los antimicrobianos en este área.
Infections are among the most prevalent conditions treated in hospital emergency departments (HEDs), antimicrobials constituting one of the most frequently prescribed drug classes. Indeed, it is estimated that 15% of patients treated in HEDs receive anti-infectious therapy.1,2 On the other hand, the decisions adopted in HEDs impact the whole hospitalization process as many of the drugs prescribed at the HED are administered to patients throughout their stay in hospital. Moreover, correct antimicrobial treatment (AMT) selection is a complex endeavor as, more often than not, it must be done empirically. According to some authors, however, this selection is inappropriate in up to five of every ten patients, increasing the length of their hospital stay.3,4 For these reasons, and in order to optimize and homogenize the prescription of AMTs and reduce the incidence of resistant microorganisms, the Spanish Action Plan on Antimicrobial Resistance (PRAN) includes an antibiotic resistance strategy that proposes that prescribers use empirical antimicrobial treatment guidelines adapted to the local circumstances of each hospital.5 Needless to say, an appropriate empirical antibiotic prescription strategy should consider, apart from epidemiological factors and local sensitivity/resistance patterns, elements such as the infection site, the patient's profile and the pharmacokinetic and pharmacodynamic (PK/PD) characteristics of the prescribed antimicrobials.6–8
Despite the importance of aligning prescriptions to the therapeutical guidelines in force, few HEDs take the latter into consideration when prescribing an antimicrobial.9–11 It has been estimated that between 50 and 63% of prescriptions do not follow the advice provided in the local AMT guidelines,10,11 in contravention of the recommendations of the PRAN.
In the last few years, a series of studies have been published that underscore the importance that, in patients with severe infections, AMT be administered early on during their stay in the HED as it has a direct impact on their survival. This has resulted in clinical guidelines incorporating the recommendation to administer AMT within a specific time window for certain infections and clinical situations such as sepsis. However, some authors have suggested that, without an appropriate diagnosis, early administration could lead to an increase in the number of inappropriate AMTs.12 Unawareness of the risks inherent in inappropriate antimicrobial prescribing in areas such as the HED is undoubtedly as problematic as the lack of consensus about the most crucial criteria to be met when prescribing antimicrobials.
Against this background, HEDs are considered a key area where hospital pharmacists can make crucial contributions to more effective antimicrobial use. In this connection, the present study is intended to describe the degree of compliance of antimicrobial prescriptions with local guidelines for the treatment of infections by HEDs, and to find out the clinical and epidemiological characteristics of patients receiving such prescriptions. Moreover, we set about conducting a feasibility study for the design and implementation of research projects that address specific aspects related to inappropriate antimicrobial prescribing. The idea was to identify areas where specific actions can be applied to enforce the recommendations of antimicrobial stewardship programs (AMSPs).
Materials and methodsDesign and patient selectionThis was a descriptive cross-sectional observational pilot study carried out at the emergency department of a second-level Spanish hospital with a catchment population of 265,000 inhabitants, which deals with about 250 emergencies a day. Data was gathered in a retrospective manner.
For the recruitment of patients and the collection of data, seven cross sections were made corresponding to the seven days of the week, during seven consecutive weeks, from January to February 2020. Inclusion criteria were as follows: patients had to be over 14 years of age and they were required to have had at least one first AMT dose prescribed to them by a specialist or a resident from the HED by the day of the study. Patients who in spite of being in the HED had not received their first antimicrobial dose by the day of the study were excluded.
The size of the study sample was calculated on the basis of the mean number of patients admitted each day to the HED (around 250), with a 15% prevalence of antibiotic prescriptions.2 Moreover, considering the assumption that 63% of antimicrobial prescriptions by HEDs do not follow the local guidelines,11 as well as a 95% confidence interval, a precision of +/− 10 percentage units, and a 10% replacement rate, the minimum sample size was estimated at 120 patients.
VariablesDemographic variables (age, sex, weight) and clinical variables (Charlson index and chronic renal failure, multi-resistance factors [institutionalised patient, instrumentation in the last month, immunosuppressed, antibiotherapy or hospitalisation in the last 3 months or history of multi-resistance]13 were collected in a coded database; focus, site of acquisition of infection and severity of infection, antimicrobial prescribed, timing of first dose, type of prescription [empirical, targeted, prophylactic] and compliance with PK/PD recommendations).
Compliance of the antibiotic prescription with the recommendations of the hospital's clinical guidelines for empirical antimicrobial treatment was defined as the main variable. These protocols, which are drawn up and regularly updated by the hospital's infectious disease committee, are based on the recommendations laid out in the PRAN, can be accessed through the hospital's web portal, and are classified according to the different infection sites.
In order to identify priority intervention targets, inappropriate antimicrobial prescriptions, i.e. those where the recommendations of local guidelines were not followed, were classified into four categories:10a) Unnecessary antimicrobial: No signs or symptoms indicative of infection were reported in the patient's clinical record; b) Inactive antimicrobial: The antimicrobial administered was not appropriate for the pathogen, empirical treatment being required. In the case of targeted treatment, antimicrobials in this category appeared as resistant in the antibiogram; c) Active yet not recommended antimicrobial: The antimicrobial proved to be active against the expected pathogens, although it did not feature as recommended in the local guidelines; d) Active yet incorrectly dosed antimicrobial: The antimicrobial was incorrectly dosed in terms of the PK/PD parameters (loading dose, if appropriate, weight-based dose, renal failure-based adjustment, liver failure-based dosing) included in the product's Summary of Product Characteristics, which may be obtained from the Spanish Medicines and Health products Agency.14
With a view to understanding the consequences of inappropriate prescription, the study also recorded cases of long hospital stays as well as all readmissions and instances of mortality within 30 days of the patient's visit to the emergency department. A hospital stay was considered “long” when it was longer (in days) than the mean hospital stay of the overall sample. It must be noted that patients suffering a septic shock and those who died while admitted were removed from the sample.
Work planThe AMTs prescribed on the day of the study were identified by computer screening. All the prescriptions given that day were classified according to the drug class prescribed and a code-protected list was drawn up of the patients who received the AMTs. The HPHCIS software (v. 3.8) was used as a support to the patients' clinical records and to the information on the episode that had resulted in their visit to the emergency department. Compliance of prescriptions with local guidelines was assessed in pairs by medical specialists from the HED and two hospital pharmacists. Discrepancies between practitioners were resolved by a third evaluator, who was a specialist in infectious diseases.
Statistical analysisAll variables were subject to a descriptive analysis. Categorical variables were estimated by means of overall percentages and frequencies. Normality was determined for all quantitative variables using the Kolmogorov–Smirnov test. Parametric variables were expressed as mean ± standard error of the mean, and non-parametric variables were expressed as median and interquartile range. The association between qualitative variables was evaluated with the chi-squared test, while parametric and non-parametric-tests were conducted for quantitative variables (e.g., Student's t test and the Wilcoxon test, respectively, depending on the normality of the variables' distribution). Cohen's kappa coefficient was used to measure the agreement/disagreement between the different practitioners. Statistical significance was set at a p value <0.05. The statistical analysis was carried out using the SPSS v.23 and GraphPad v.8 software packages.
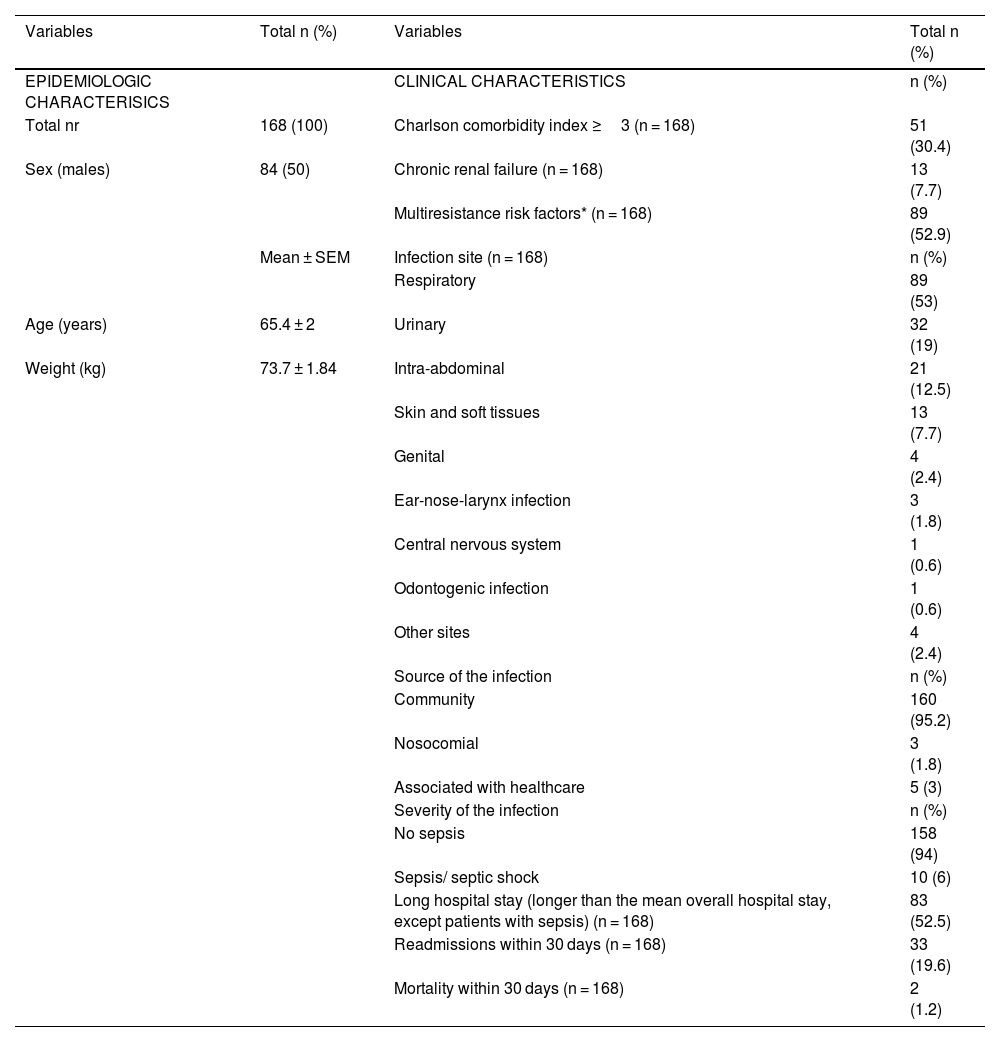
ResultsBaseline characteristics of the patients treated with antimicrobialsOf the 187 patients that had presented to the HED with an infection and who received at least one antimicrobial, 168 met the inclusion criteria. Nineteen were excluded on account of not being given the first antimicrobial dose on the day of the study. A total of 192 antimicrobials were administered to these 168 patients. All the patients presented with a single infection site, with all the infections observed featuring among those included in the clinical guidelines (Table 1). In 53% of patients, the infection was respiratory; 95.2% of all infections were community-acquired, and 94% were not associated with sepsis. Table 1 contains a description of the patients' clinical and epidemiologic profile.
Descriptive analysis of the epidemiological and clinical profile of patients on antimicrobial treatment due to infection as indicated by the hospital emergency department (HED).
| Variables | Total n (%) | Variables | Total n (%) |
|---|---|---|---|
| EPIDEMIOLOGIC CHARACTERISICS | CLINICAL CHARACTERISTICS | n (%) | |
| Total nr | 168 (100) | Charlson comorbidity index ≥3 (n = 168) | 51 (30.4) |
| Sex (males) | 84 (50) | Chronic renal failure (n = 168) | 13 (7.7) |
| Multiresistance risk factors* (n = 168) | 89 (52.9) | ||
| Mean ± SEM | Infection site (n = 168) | n (%) | |
| Respiratory | 89 (53) | ||
| Age (years) | 65.4 ± 2 | Urinary | 32 (19) |
| Weight (kg) | 73.7 ± 1.84 | Intra-abdominal | 21 (12.5) |
| Skin and soft tissues | 13 (7.7) | ||
| Genital | 4 (2.4) | ||
| Ear-nose-larynx infection | 3 (1.8) | ||
| Central nervous system | 1 (0.6) | ||
| Odontogenic infection | 1 (0.6) | ||
| Other sites | 4 (2.4) | ||
| Source of the infection | n (%) | ||
| Community | 160 (95.2) | ||
| Nosocomial | 3 (1.8) | ||
| Associated with healthcare | 5 (3) | ||
| Severity of the infection | n (%) | ||
| No sepsis | 158 (94) | ||
| Sepsis/ septic shock | 10 (6) | ||
| Long hospital stay (longer than the mean overall hospital stay, except patients with sepsis) (n = 168) | 83 (52.5) | ||
| Readmissions within 30 days (n = 168) | 33 (19.6) | ||
| Mortality within 30 days (n = 168) | 2 (1.2) |
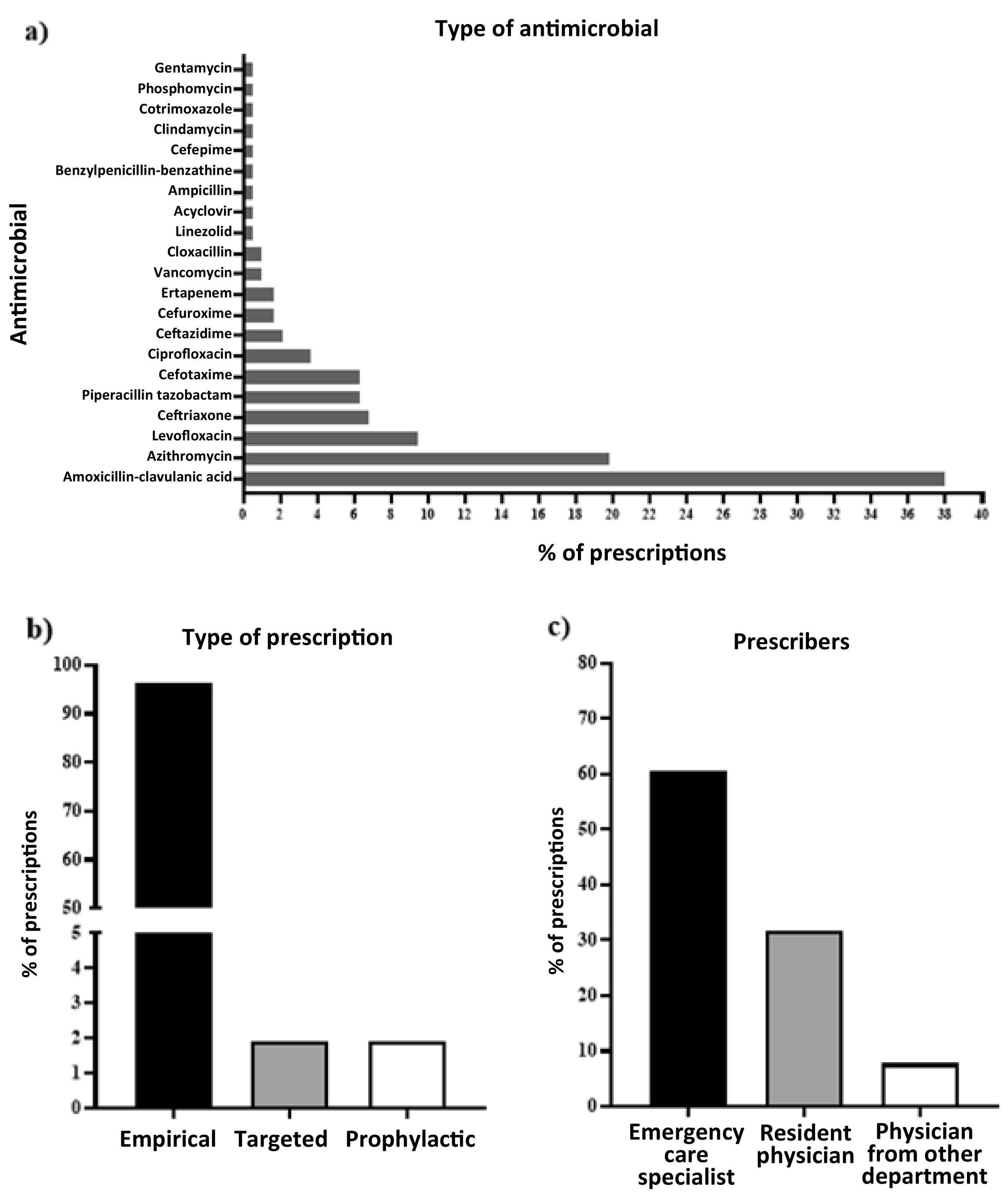
A total of 20 different antimicrobials were prescribed, with the following prevalence: amoxicillin-clavulanic acid: 38%; azithromycin: 19.8%; levofloxacin: 9.4%; ceftriaxone: 7%; cefotaxime: 6.3%; piperacillin-tazobactam: 6.3%; ciprofloxacin: 4.2%. The remaining antimicrobials presented with a prescription prevalence under 4% (Fig. 1a). A total of 96.2% of prescriptions were empirical (Fig. 1b) and 60.4% were decided by specialist physicians from the HED (Fig. 1c). Seventy-six (39.6%) of the prescriptions were inappropriate in terms of the local guidelines. Forty-two (55%) of these were active yet not recommended treatments; 18 (23.5%) were inactive treatments; 10 (13.7%) were active yet inappropriately dosed treatments, and 6 (7.8%) were unnecessary treatments according to the guidelines. The strength of agreement regarding the adequacy of treatment between physicians and pharmacists was high (kappa index = 0.71, 95% CI =0.6–0.8). The median time elapsed between the diagnosis and administration of the treatment was 4 h and 9 min, with a range between 15 min and 24 h and 29 min. A total of 52.5% of patients stayed in hospital for over 4 days; 19.6% of patients were readmitted within 30 days. The 30-day death rate was 1.2% (Table 1).
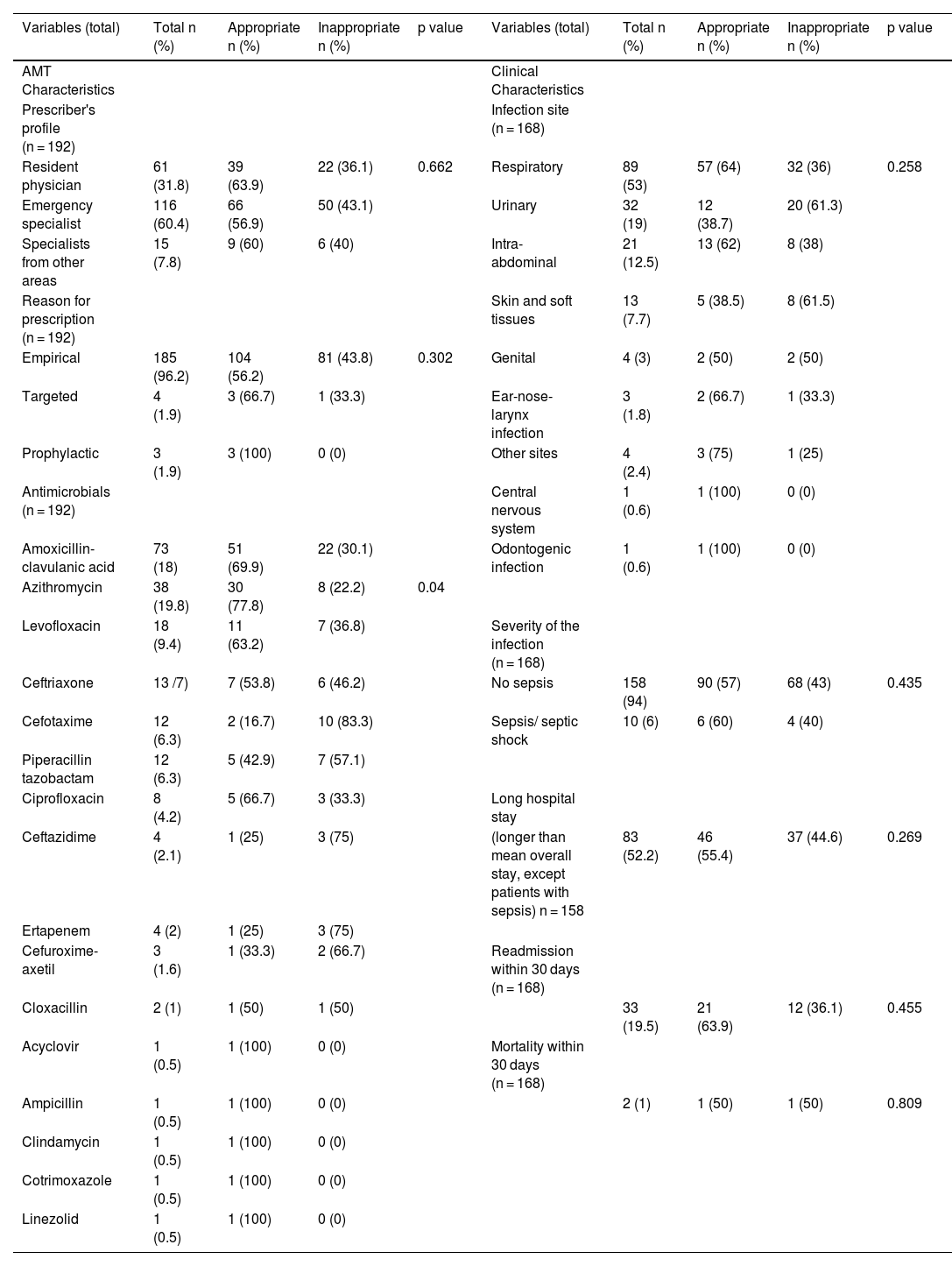
Characteristics of antibiotic prescriptions according to their compliance with local guidelinesThe characteristics of the antibiotic prescriptions of patients treated as per the recommendations of local guidelines were compared with those of patients who were not treated in accordance with such guidelines (Table 2). No significant differences were found in prescribers' profiles (p = 0.662) or types of prescriptions (p = 0.302).
Characteristics of antibiotic prescriptions according to their compliance with local guidelines.
| Variables (total) | Total n (%) | Appropriate n (%) | Inappropriate n (%) | p value | Variables (total) | Total n (%) | Appropriate n (%) | Inappropriate n (%) | p value |
|---|---|---|---|---|---|---|---|---|---|
| AMT Characteristics | Clinical Characteristics | ||||||||
| Prescriber's profile (n = 192) | Infection site (n = 168) | ||||||||
| Resident physician | 61 (31.8) | 39 (63.9) | 22 (36.1) | 0.662 | Respiratory | 89 (53) | 57 (64) | 32 (36) | 0.258 |
| Emergency specialist | 116 (60.4) | 66 (56.9) | 50 (43.1) | Urinary | 32 (19) | 12 (38.7) | 20 (61.3) | ||
| Specialists from other areas | 15 (7.8) | 9 (60) | 6 (40) | Intra-abdominal | 21 (12.5) | 13 (62) | 8 (38) | ||
| Reason for prescription (n = 192) | Skin and soft tissues | 13 (7.7) | 5 (38.5) | 8 (61.5) | |||||
| Empirical | 185 (96.2) | 104 (56.2) | 81 (43.8) | 0.302 | Genital | 4 (3) | 2 (50) | 2 (50) | |
| Targeted | 4 (1.9) | 3 (66.7) | 1 (33.3) | Ear-nose-larynx infection | 3 (1.8) | 2 (66.7) | 1 (33.3) | ||
| Prophylactic | 3 (1.9) | 3 (100) | 0 (0) | Other sites | 4 (2.4) | 3 (75) | 1 (25) | ||
| Antimicrobials (n = 192) | Central nervous system | 1 (0.6) | 1 (100) | 0 (0) | |||||
| Amoxicillin-clavulanic acid | 73 (18) | 51 (69.9) | 22 (30.1) | Odontogenic infection | 1 (0.6) | 1 (100) | 0 (0) | ||
| Azithromycin | 38 (19.8) | 30 (77.8) | 8 (22.2) | 0.04 | |||||
| Levofloxacin | 18 (9.4) | 11 (63.2) | 7 (36.8) | Severity of the infection (n = 168) | |||||
| Ceftriaxone | 13 /7) | 7 (53.8) | 6 (46.2) | No sepsis | 158 (94) | 90 (57) | 68 (43) | 0.435 | |
| Cefotaxime | 12 (6.3) | 2 (16.7) | 10 (83.3) | Sepsis/ septic shock | 10 (6) | 6 (60) | 4 (40) | ||
| Piperacillin tazobactam | 12 (6.3) | 5 (42.9) | 7 (57.1) | ||||||
| Ciprofloxacin | 8 (4.2) | 5 (66.7) | 3 (33.3) | Long hospital stay | |||||
| Ceftazidime | 4 (2.1) | 1 (25) | 3 (75) | (longer than mean overall stay, except patients with sepsis) n = 158 | 83 (52.2) | 46 (55.4) | 37 (44.6) | 0.269 | |
| Ertapenem | 4 (2) | 1 (25) | 3 (75) | ||||||
| Cefuroxime-axetil | 3 (1.6) | 1 (33.3) | 2 (66.7) | Readmission within 30 days (n = 168) | |||||
| Cloxacillin | 2 (1) | 1 (50) | 1 (50) | 33 (19.5) | 21 (63.9) | 12 (36.1) | 0.455 | ||
| Acyclovir | 1 (0.5) | 1 (100) | 0 (0) | Mortality within 30 days (n = 168) | |||||
| Ampicillin | 1 (0.5) | 1 (100) | 0 (0) | 2 (1) | 1 (50) | 1 (50) | 0.809 | ||
| Clindamycin | 1 (0.5) | 1 (100) | 0 (0) | ||||||
| Cotrimoxazole | 1 (0.5) | 1 (100) | 0 (0) | ||||||
| Linezolid | 1 (0.5) | 1 (100) | 0 (0) |
The conformity of qualitative variables (characteristics of antimicrobial treatments) with the guidelines was measured by means of the chi-squared test; whereas the conformity of quantitative variables (clinical characteristics) was measured by means of the t-test. Statistical significance was set at a p value <0.05. Total number of prescriptions: 192.
Inappropriate prescriptions occurred mainly in the case of urinary or skin and soft tissue infections, although no statistically significant differences were observed with respect to infection site, severity, length of hospital stay, readmissions or mortality within 30 days.
DiscussionSince the PRAN was implemented in 2014, there has been an increasing interest in optimizing and homogenizing the prescription of antimicrobial treatments through clinical guidelines. The purpose is to reduce the incidence of resistant microorganisms.5 Nonetheless, there is a scarcity of studies on how compliant current prescriptions are with the local guidelines and on their impact on areas such as emergency care. The present pilot study, developed in the context of an HED, was therefore designed to evaluate the extent to which antibiotic prescriptions comply with the hospital's empirical treatment guidelines, paving the way for the development of future studies and strategies to promote antimicrobial stewardship.
The study showed that four in every ten prescriptions made in the HED was not aligned with local guidelines, a considerably lower figure than those reported in the few articles in the literature.10,11,15–17 Most antimicrobials had the right spectrum of activity and were prescribed at the right dose, but they were not included in the local empirical antibiotic therapy guidelines, i.e. they were active yet not recommended agents. This prescription category accounted for 55% of all inappropriate prescriptions and for 21.9% of all AMT prescriptions. These figures are higher than those reported by Oltra et al.,10 who found overall inappropriate prescription rates of 51.4% and 27.1% of active yet not recommended antimicrobial prescriptions, which – in turn - accounted for 14% of all AMT prescriptions. Although no statistically significant differences were found in terms of prescriber profile or other analyzed variables, it could be assumed that prescription inappropriateness was due to a prioritization of personal clinical experience and routine clinical practice over the use of empirical antimicrobial treatment guidelines, or to limited familiarity with approved protocols. This study was therefore able to demonstrate that there is a need to identify the reasons behind inappropriate prescribing as that would make it possible to develop specific strategies aimed at reducing the incidence of inappropriate prescriptions and boost adherence to the guidelines. Inappropriate prescriptions included a higher incidence of inaccurate definitions of urinary, skin and soft tissue infection sites than of other sites. Great emphasis should therefore be placed on analyzing antimicrobial prescriptions for infections in those sites, ensuring that the results of such studies be used to update and disseminate clinical protocols and develop training programs for HED staff.
It is also essential to consider the specific characteristics of HEDs, where 96.3% of AMT prescriptions are empirical in nature. This means that no data exists on the microorganisms responsible for infections or on the sensitivity patterns present at the time of prescription. Despite this high rate of empiricism, few studies have described the rate of compliance of HED prescriptions with clinical guidelines or the implications of noncompliance. AMSPs play an important role in this regard5 as these programs, included in the PRAN's recommendations, seek to optimize antimicrobial prescribing in order to improve the clinical benefits obtained by patients, minimize the incidence of adverse events, monitor the appearance of resistances, and ensure therapeutic cost-efficiency.18 In this respect, González-del Castillo et al.4 analyzed the effect of applying the AMSP to 376 patients admitted to an HED with some kind of infection and observed a reduction of up to 15.8% in the number of inappropriate prescriptions, which they attributed to the strict adherence of the HED to empirical antimicrobial treatment guidelines and to the implementation of related training activities promoted by AMSP-specialized practitioners. Along the same lines, Zimmerman et al.19 observed a significant increase in the compliance of antimicrobial prescriptions with the clinical guidelines in cases of community-acquired pneumonia following the promotion of protocols and the training of prescribers. This study, in line with others in the literature, identified a need to develop and implement empirical anti-infectious treatment protocols and encourage the implementation of continuous training programs for emergency care providers.3 At the same time, the last few years have seen an increasing trend to include pharmacists in different clinical activities given the realization of the importance of involving them in multidisciplinary emergency teams.20 According to a recent publication by the American Society of Health-System Pharmacists, clinical pharmacists have a responsibility to take prominent roles in antimicrobial stewardship and infection prevention and control programs.21 This statement is meant as an encouragement for hospital pharmacists to champion antimicrobial stewardship.
This study is not without limitations. Firstly, it is a descriptive cross-sectional observational pilot study, which contributes information from one single center, obtained following a longitudinal process. In addition, the retrospective review of the patients' clinical records lacks clinical rigor given the work overload the HED was subject to, which meant that no data could be obtained on certain parameters. The subsequent review by different specialists and the agreement analysis carried out confirmed a high incidence of inappropriate prescriptions.
In a nutshell, the HED analyzed demonstrated a high incidence of inappropriate antimicrobial prescribing according to local treatment guidelines. The results of this study are indicative of the feasibility and importance of continued investigation into this issue, and provide essential information for carrying out larger-scale projects geared towards implementing strategies devoted to promoting antimicrobial stewardship in HEDs.
Submission for presentation at congressesThe preliminary results of the study were submitted under the title Appropriate antimicrobial prescribing in an emergency department as a poster to the 65th National SEFH Congress, held online from the 20th to the 22nd of October 2020.
Ethical responsibilitiesThe study was conducted according to the standards of good clinical practice and ethical and ethical principles, which have their origin in the Declaration of Helsinki, and was approved by the local Research Ethics Committee (IB1512/20). (IB1512/20). Data were collected in a coded form, through retrospective review of medical records.
FundingNo funding.
Authorship statementAll six authors declare that they have intellectually contributed to the design of the article, to the collection of data, to the analysis and interpretation of results, and to the writing of the manuscript. They have all approved the final version submitted for publication.
Contribution to the literatureThe present study analyzed compliance of antimicrobial use with local guidelines in a hospital emergency department. The information obtained is essential for the development of antimicrobial stewardship strategies.