To analyze compliance with a prescribed pre-surgical antibiotic prophylaxis protocol established by the Antimicrobial Stewardship Program team and the Orthopedics Department of Hospital Mexico, a public hospital located in Costa Rica, from February to March 2019. No assessments of compliance with the protocol had been conducted since its introduction in 2018, nor had variations in surgical site infection rates been determined.
MethodThis is a retrospective observational study that extended from February 1st to March 31st, 2019. We identified patients hospitalized during the study period in the hospital's Orthopedics Department. We reviewed each patient's medical record to record their prescribed antibiotic prophylaxis. Following an analysis of the overall compliance with the protocol, we made an estimation of the surgical site infection rate as well as a descriptive analysis of the studied population.
ResultsThe study included 110 clinical records. The most frequently prescribed antibiotics were clindamycin and gentamicin. Compliance with the protocol ranged between 89.1% and 100% across the different criteria, except for dosing appropriateness and prescription of antibiotics at discharge (14.3% and 65.8%, respectively). The most common non-compliance factor was gentamicin's dosing. The surgical site infection rate was 5%.
ConclusionsThe preoperative antibiotic prophylaxis protocol established between the Antimicrobial Stewardship Program team and the Orthopedic Department reduced the length of exposure to postoperative antibiotics to only 24 hours and enjoyed widespread acceptance and a high compliance rate. However, compliance with some criteria must be improved, such as dosing appropriateness and prescription of antibiotics at discharge. Involvement of the pharmacist is vital for the compliance with and auditing of these types of protocols as pharmacists are uniquely positioned to ensure that high-quality antibiotic prophylaxis is provided in all surgical procedures that require it.
Analizar el cumplimiento en la prescripción de la profilaxis antibiótico prequirúrgica, según el protocolo establecido por el Programa de Optimización de Antibióticos y el Servicio de Ortopedia del Hospital México, Caja Costarricense del Seguro Social, ubicado en San José, Costa Rica, de febrero a marzo de 2019. Desde la instauración del protocolo en 2018 no se ha realizado una evaluación de su cumplimiento ni se ha determinado la tasa de infección del sitio quirúrgico.
MétodoEstudio observacional retrospectivo; se identificaron los pacientes hospitalizados en el Servicio de Ortopedia desde el 1 de febrero al 31 de marzo de 2019. Se accedió al expediente digital de cada paciente, se caracterizó la profilaxis antibiótica prescrita y se analizó el cumplimiento según el protocolo vigente. Se estimó la tasa de infección de sitio quirúrgico. Se realizó un análisis descriptivo de la población.
ResultadosEl estudio incluyó 110 expedientes clínicos. Los antibióticos más prescritos fueron clindamicina y gentamicina de manera concomitante. El cumplimiento de la prescripción de profilaxis antibiótica osciló entre 89,1% y 100% para los criterios considerados en el protocolo, exceptuando dosis y antibiótico al alta (14,3 y 65,8%, respectivamente). El criterio de incumplimiento más frecuente fue la dosis de gentamicina. La tasa de infección de sitio quirúrgico fue del 5%.
ConclusionesEl protocolo de profilaxis antibiótica prequirúrgica establecido entre el equipo Programa de Optimización de Antibióticos y el Servicio de Ortopedia disminuyó el tiempo de exposición a antibióticos postoperatorios a únicamente 24 horas, y tiene una aceptación y cumplimiento positivo. Sin embargo, deben mejorarse puntos como la prescripción adecuada de la dosis y la no prescripción de antibiótico al egreso. La participación del farmacéutico es vital para el cumplimiento y auditoría de este tipo de protocolos, de modo que la calidad de la profilaxis antibiótica sea garantizada en todos los procedimientos quirúrgicos que así lo requieran.
Antimicrobial Stewardship Programs (ASPs) have been defined as coordinated interventions by a multidisciplinary team intended to improve and measure the safe and appropriate use of antibiotic agents by promoting the selection of the optimal antibiotic regimen including dosing, duration of therapy and route of administration1.
Implementation of these programs is one of the most effective ways of improving clinical outcomes in patients with bacterial infections, minimizing the incidence of adverse events (including appearance and expansion of antimicrobial resistance) and ensuring the administration of cost-effective treatments2,3.
In 2019, Costa Rica launched its “2018-2025 National Action Plan on Antimicrobial Resistance”. With the aim of monitoring, reducing and controlling antimicrobial resistance in human, animal and plant populations, the Plan promotes the implementation of ASPs across the different hospitals in the country4.
The design of protocols that control the use of preoperative antibiotic prophylaxis is based on a timely selection and administration of antibiotics in order to prevent surgical site infections (SSIs), which are estimated to account for 20% of all healthcare-associated infections, negatively impacting the patients’ quality of life and increasing healthcare costs as a result of longer hospital stays5,6. Controlling SSIs is therefore essential to reduce morbimortality and the duration and cost of medical care, and to minimize the adverse consequences of such infections for patients’ microbial flora7–9.
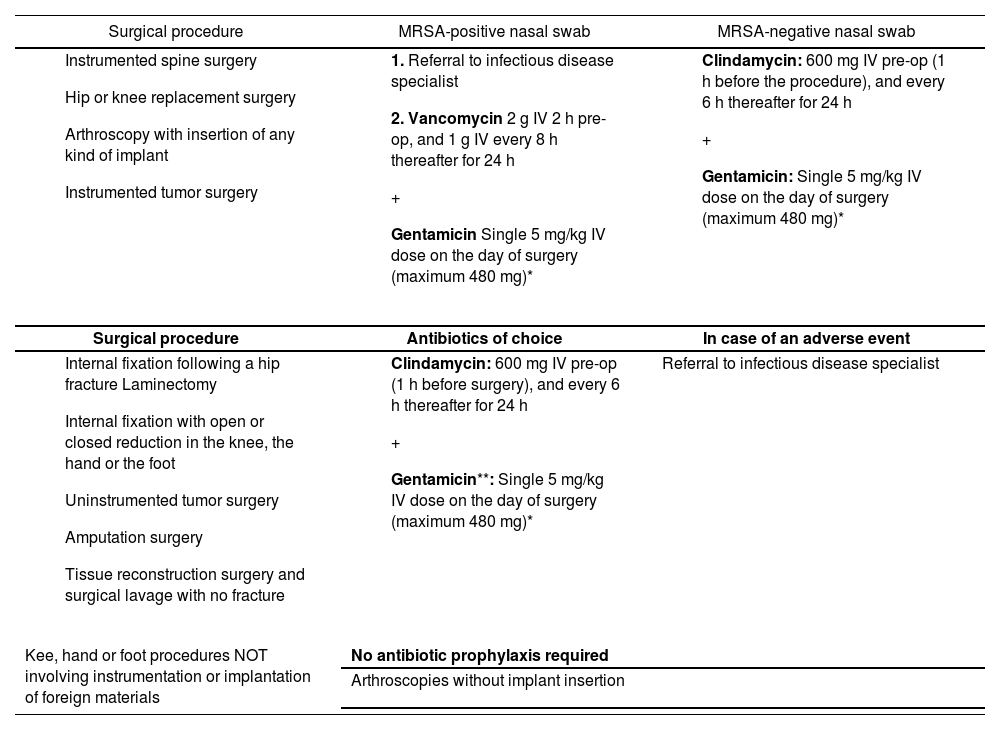
In 2018 an ASP team was set up at Hospital México in San Jose, Costa Rica comprising infectious disease specialists, pharmacists, microbiologists, epidemiologists, and nursing staff. The team's first decision was to work together with the Orthopedic Department to implement a preoperative antibiotic prophylaxis protocol for orthopedic procedures with a view to optimizing presurgical antibiotic prophylaxis, providing clear clinical and operational guidelines for antibiotic selection (see Table 1). The guidelines, based on the literature and on the hospital's epidemiological situation, were an update of the previous protocol, which established that preoperative antibiotics had to be administered for 72 hours.
Recommended preoperative antibiotic prophylaxis for orthopedic procedures
| Surgical procedure | MRSA-positive nasal swab | MRSA-negative nasal swab |
|---|---|---|
|
|
|
| Surgical procedure | Antibiotics of choice | In case of an adverse event |
| Referral to infectious disease specialist | |
| Kee, hand or foot procedures NOT involving instrumentation or implantation of foreign materials | No antibiotic prophylaxis required | |
| Arthroscopies without implant insertion | ||
MRSA: methicillin-resistant staphylococcus aureus.
Source: Programa de Optimización de Antibióticos-Hospital México. Protocolo para el manejo de profilaxis antibiótica en el Servicio de Ortopedia. San Jos, Costa Rica. 2018.
According to onsite epidemiological analyses, the germs most frequently isolated at the Orthopedic Department of Hospital Mexico between 2017 and 2018 were Staphylococcus aureus and several gram-negative bacilli (GNBs) such as Enterobacter cloacae, Providencia rettgeri, Escherichia coli, Proteus mirabilis, Citrobacter koseri and Pseudomonas aeruginosa. As cephalothin reached levels of resistance greater than 50% to these germs, it was considered justified the use of clindamycin and gentamicin concomitantly, in all cases except those with a methicillin-resistant staphylococcus aureus (MRSA)-positive nasal swab, where vancomycin was indicated instead of clindamicyn9.
The specific goals of our study were to analyze the level of compliance with the antibiotic prophylaxis protocol established by the ASP team and the Orthopedic Department between February and March 2019 and to determine the SSI rate in the studied population.
MethodsWe carried out a retrospective observational study to analyze compliance by the orthopedics team with the established preoperative antibiotic prophylaxis. As the analysis covered the whole population, the total sample of clinical cases was defined in accordance with the period of time considered in the study. The studied population comprised the cases hospitalized from February 1st to March 31st 2019 who underwent an orthopedic surgical procedure.
Exclusion criteria comprised incomplete or unavailable patient data on the Single Digital Health Record platform (EDUS, for its acronym in Spanish) and/or cases where the procedure was not among those contemplated in the hospital's ASP. No distinctions were made in terms of age, sex, ethnicity, sexual orientation or any other factors. The study was approved by the hospital's ethics committee.
Study variables included age, sex, weight, presence of drug allergies, type of procedure, results of the MRSA nasal swab, antibiotic characteristics (type, dosing, frequency of administration, length of administration prior to the procedure, duration, and antibiotic prescription at discharge) and SSI rate. A record was kept of the degree of compliance with presurgical antibiotic prophylaxis and the presence of absence of SSI at 30 days post-op.
A Microsoft Excel® data collection form and a database were designed to record all the relevant information. The Labcore® system was used to document the results of the MRSA nasal swabs. In addition, the Costa Rican Integrated Pharmacy System (SIFA®, for its acronym in Spanish) was used to evaluate the levels of dispensation of the required antibiotics. Both Labcore® and SIFA® are software solutions used by the Costa Rican Social Security (CCSS, for its acronym in Spanish).
We made a descriptive analysis of the sample. Qualitative variables were described with their frequency distributions (number and percentages). Quantitative variables were recorded as mean and standard deviation (SD). No comparison groups were used. In the course of the study, we made an analysis of the degree of compliance with all the aspects defined in the ASP (Tables 1 and 2). Finally, the SSI rate was calculated.
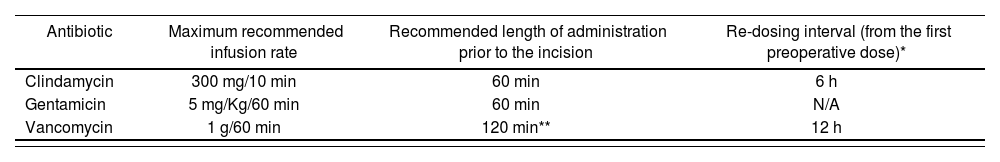
Dosing, length of administration and re-dosing intervals for preoperative antibiotic prophylaxis
| Antibiotic | Maximum recommended infusion rate | Recommended length of administration prior to the incision | Re-dosing interval (from the first preoperative dose)* |
|---|---|---|---|
| Clindamycin | 300 mg/10 min | 60 min | 6 h |
| Gentamicin | 5 mg/Kg/60 min | 60 min | N/A |
| Vancomycin | 1 g/60 min | 120 min** | 12 h |
Source: Programa de Optimización de Antibióticos-Hospital México. Protocolo para el manejo de profilaxis antíbíótíca en el Servicio de Ortopedia. San José, Costa Rica. 2018.
The present study analyzed a total of 110 clinical cases, corresponding to 54 males (49.1%) and 56 females (50.9%). Mean age was 58.2 years (SD = 20.2); 48.5 years for the male subjects (SD = 20.7) and 67.5 years for the female subjects (SD = 20.8). Mean patient weight was 71.3 kg (SD = 14.2).
Seven of the 110 clinical cases (6%) experienced drug allergies but none of them developed allergies to the medicines established in the protocol. The main procedures carried out were internal fixation with open or closed reduction in the knee, the hand or the foot (46%), hip or knee replacement surgery (25%), and instrumented spine surgery (14%). Although, it was deemed advisable to carry out a MRSA nasal swab in 47 of the 110 procedures performed, this was not documented in the patients’ records.
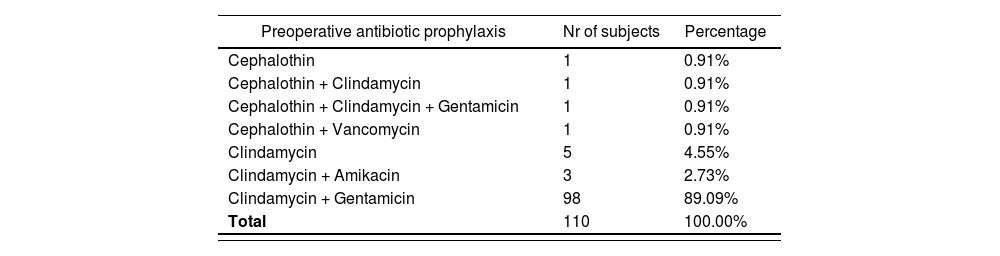
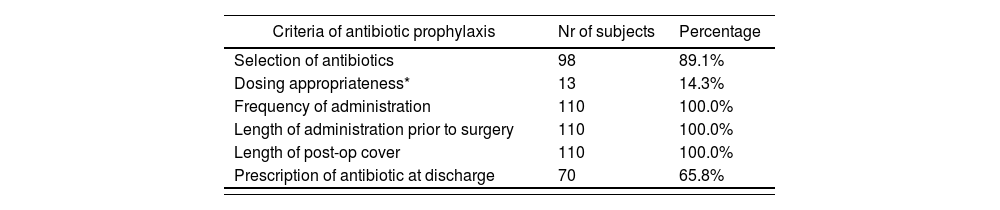
Table 3 shows the number of patients who were prescribed the different antibiotics and the percentage they represented of the total sample. The different agents were prescribed alone or in combination depending on the characteristics of each patient. Table 4 shows the level of compliance with the protocol in terms of prescribed dose, frequency of administration, length of administration prior to surgery, and length of post-operative cover of the prescribed agent(s). Compliance with the dosing appropriateness criterion was calculated on the basis of 91 of the 110 subjects that made up the sample as 8 subjects whose body weight had not been documented had to be excluded from this calculation.
Preoperative antibiotic prophylaxis prescribed during the study. The different agents were prescribed alone or in combination depending on the characteristics of each patient
| Preoperative antibiotic prophylaxis | Nr of subjects | Percentage |
|---|---|---|
| Cephalothin | 1 | 0.91% |
| Cephalothin + Clindamycin | 1 | 0.91% |
| Cephalothin + Clindamycin + Gentamicin | 1 | 0.91% |
| Cephalothin + Vancomycin | 1 | 0.91% |
| Clindamycin | 5 | 4.55% |
| Clindamycin + Amikacin | 3 | 2.73% |
| Clindamycin + Gentamicin | 98 | 89.09% |
| Total | 110 | 100.00% |
Compliance with the preoperative antibiotic prophylaxis protocol established by the ASP team and the Orthopedics Department
| Criteria of antibiotic prophylaxis | Nr of subjects | Percentage |
|---|---|---|
| Selection of antibiotics | 98 | 89.1% |
| Dosing appropriateness* | 13 | 14.3% |
| Frequency of administration | 110 | 100.0% |
| Length of administration prior to surgery | 110 | 100.0% |
| Length of post-op cover | 110 | 100.0% |
| Prescription of antibiotic at discharge | 70 | 65.8% |
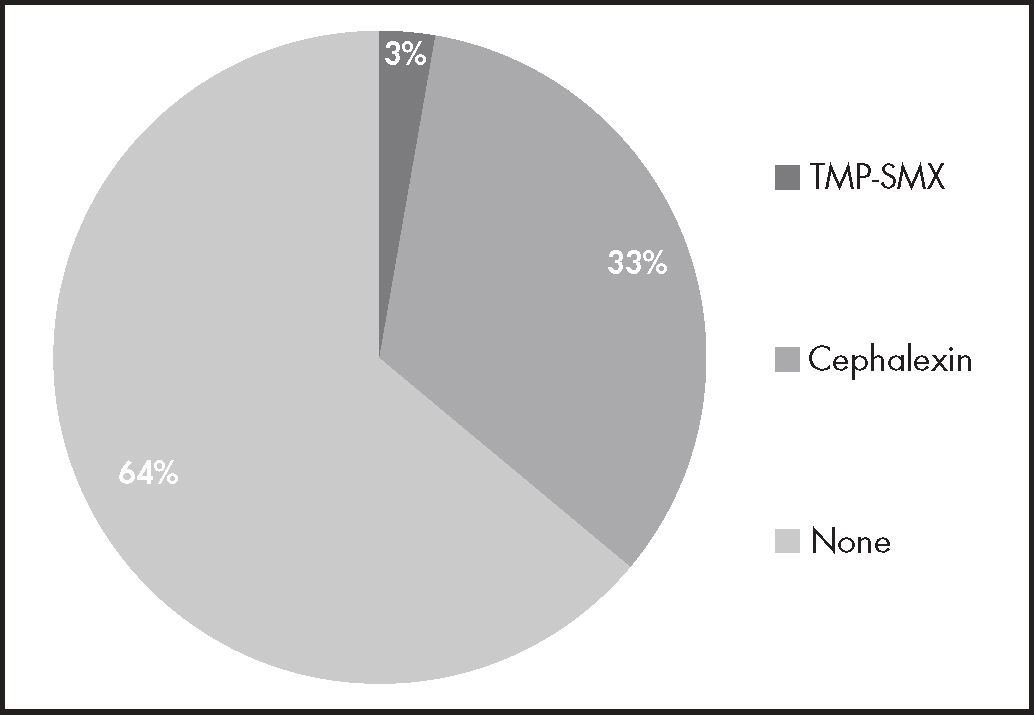
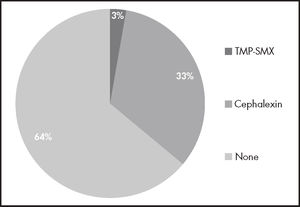
The antibiotics prescribed as post-discharge treatment were trimethoprim-sulfamethoxazole (3%) and cephalexin 500 mg (33%). In the remaining 64% of cases no antibiotic was prescribed. The SSI rate over the whole study period was 5%.
DiscussionPreoperative antibiotic prophylaxis has traditionally been considered an effective tool to prevent and/or attenuate the development of SSI. For prophylaxis to work, enough concentrations of the appropriate antibiotic has to reach the tissues and other areas surrounding the surgical site and stay in place throughout the procedure10–12. In this study, for every case where prophylaxis was prescribed there was a clear indication.
In accordance with the established protocol (Table 1), it was to be expected that clindamycin and gentamicin would be the most frequently prescribed antibiotics (Table 2), with the exception of some cases with MRSA-positive nasal swabs. However, in the cases analyzed no MRSA screening was performed.
In a similar study conducted in Australia by Chandrananth et al., the antibiotic regimen selected as preoperative prophylaxis achieved a compliance rate of 98.5%. In Spain, del-Mora-Luque et al. reported a compliance rate of 92.3%, higher than the values obtained in our study (89.1%)13,14. However, the compliance obtained in our study compares favorably with that reported by other authors. For example, a study from Qatar reports antibiotic selection compliance rates of 68.5% and length of antibiotic administration compliance rates of 40.7% with respect to the benchmark provided by the country's Nosocomial Infections Committee11. Similar data were obtained by a study of 2,373 patients from Tokyo, where the compliance rate for antibiotic selection stood between 53% and 84%, while compliance with the required length of antibiotic administration ranged from 38% to 68%15.
Regarding the time of administration of preoperative prophylaxis, a similar study reported a compliance rate of 98.6%, which indicates that findings of the present study for such criteria are more encouraging than those conveyed by the literature13.
An important aspect to be considered is the compliance with the prescribed dose of gentamicin (14.3%). One of the main barriers to compliance with the regimens recommended in the protocol was the fact that most prescriptions did not take into consideration the patients’ real or documented weight. It has recently been determined that the antibiotic dose administered should always fall within the upper range of the therapeutic dose, namely it should never be lower than the standard dose of the relevant drug. The dose must be repeated should the surgical procedure last more than double the antibiotic's half-life, or if blood loss following the administration of fluids exceeds 1.5 L16–18.
Based on the above, the main clinical consequence of administering less than the required dose of gentamicin is the risk of not reaching the serum concentration needed to trigger the drug's full bactericidal effect. In fact, in 71.6% of patients who were prescribed gentamicin the dose administered was lower than the dose that should have been prescribed according to the protocol, i.e. dependent on the patient's weight (the remaining 28.4% received a higher dose than established in the protocol). At the same time, as aminoglycosides are concentration-dependent drugs administering a lower dose than reported in the literature (5-7 mg/kg every 24 hours) could result in failure to achieve the desired therapeutic target19,20.
The second most common non-compliance criterion was antibiotic prescription at discharge. Although the expected outcome was that few patients would have to keep taking antibiotics at discharge, as many as 33% were prescribed cephalexin (Figure 1), which, in addition, was not the drug of choice for any of the patients discharged. The reasons for non-compliance are not well understood, but analyzing such reasons was beyond the scope of this study.
Clearly, the best way of improving compliance with the antibiotic prophylaxis protocols is through continuous education and awareness-raising activities geared towards the orthopedics, nursing and pharmacy staff. It is indeed essential to regularly remind these practitioners, particularly resident physicians on rotations in these departments, about the contents of the ASP guidelines, as they often come from hospitals where different practices and guidelines are adhered to.
As far as pharmacists are concerned, being the ones in charge of validating medication prescriptions places them in an ideal position to request that the patients’ weight be included in all prescriptions for preoperative antibiotic prophylaxis. This would greatly facilitate calculations of the right dose of gentamicin to be administered. Moreover, pharmacists should also review patients’ medical records to ensure they do not present with allergies; that the rate and time of administration of the antibiotic are the correct ones; and that postoperative doses are not administered for longer than 24 hours. Lastly, pharmacists should also monitor whether antibiotic therapy must be maintained in a given patient after discharge so that attending physicians can issue the relevant prescription in these cases.
According to studies monitoring the incidence of SSI, deep incisional and organ-space SSIs account for two-thirds of all SSIs. Antibiotic prophylaxis is an efficient tool to significantly reduce the incidence of these types of infections, shortening the patients’ hospital stay and morbimortality, and the cost associated with caring for these patients14,21.
The SSI rate in the studied population was 5%, which is within the range reported in the literature, which varies from 1 to 5%. This is indicative that the prophylaxis measures contained in our protocol have been successful in keeping SSIs within the normal range. Furthermore, studies performed in Singapore and the United States have also shown that overall adherence to preoperative prophylaxis guidelines can lead to a statistically significant reduction in the SSI rate22.
Its retrospective nature and its short duration (2 months) are important design-related limitations of this study. Another limitation has to do with the fact that the choice of preoperative antibiotic prophylaxis was considered correct even if no MARSA-screening was performed in patients who would have required it. This represents a bias not only with respect to the study itself but also to the whole clinical practice as the presence of pathogens such as MARSA in a patient undergoing surgery radically changes their antibiotic cover requirements to the extent that not administering the correct prophylaxis exposes them not only to a potential failure of treatment but also to the possibility of developing an SSI.
At the same time, patient follow-up was limited to no more than 30 days post-op, failing to consider the SSIs that may have developed after that period such as late chronic SSIs23. This should be taken into consideration when analyzing the complications observed as well as those arising at a later stage. Even so, as the main goal of the study, namely analyzing compliance with the preoperative antibiotic prophylaxis protocol, was successfully achieved, it could be said that the final results obtained were not impacted by that limitation.
ConclusionsThe preoperative antibiotic prophylaxis protocol analyzed in this study, which resulted in a reduction in the time of exposure to postoperative antibiotics to only 24 hours, has a widespread acceptance and satisfactory compliance rates. Nonetheless, aspects such as dosing appropriateness and the prescription of antibiotics at discharge should be improved. Barriers to compliance with proposed protocol include failure to consider the real patient's weight for the calculation of the dose of gentamicin to be administered and inappropriate prescription of antibiotic therapy at discharge.
The study emphasizes the significant role that pharmacists can play in monitoring compliance with the guidelines established by an antibiotic prophylaxis protocol, ensuring that prophylaxis is guaranteed across all surgical procedures. It also points to the need for such protocols be linked to educational activities geared towards all departments involved to ensure the application of antibiotic prescription and administration best practices, thereby minimizing any adverse effects associated to the use of antimicrobials.
The guidelines established in the protocol have contributed to maintaining the SSI rate at levels considered acceptable by the literature. This means that every patient undergoing an orthopedic procedure should receive a combination of clindamycin (or vancomycin, depending on the result of the MRSA nasal swab) and gentamicin to ensure that they benefit from effective and appropriate preoperative antibiotic prophylaxis.
FundingNo funding.
AcknowledgementsThe authors would like to thank the Hospital Mexico's Pharmacy Department for allowing them access to the different databases used to obtain the data used in this study. They would like to express their appreciation towards the different staff members of both Hospital Mexico and the School of Pharmacy for their support, particularly Dr. Carlos Ramírez Valverde for his invaluable advice.
Conflict of interestNo conflict of interest.
Contribution to the scientific literature
The present study presents the hospital pharmacists as a facilitator in the design and evaluation of, and compliance with the guidelines established in an Antimicrobial Stewardship Program. As key components in the multidisciplinary teams responsible for patient management in Costa Rica's Social Security system, pharmacists play a vital role in ensuring the quality of antibiotic prophylaxis across all orthopedic procedures.
The results of the study confirm the need to supplement antimicrobial stewardship programs with continuing education programs geared toward all relevant healthcare providers to optimize best practices in terms of antibiotic prescription and administration and minimize any adverse effects associated with the use of antimicrobials.