To prioritise the initiatives to be developed for the development of the Strategic Map of Outpatient Care (MAPEX) project to improve the quality of care and pharmaceutical care for patients seen in hospital pharmacy outpatient clinics in the period 2024–2027 in Spain.
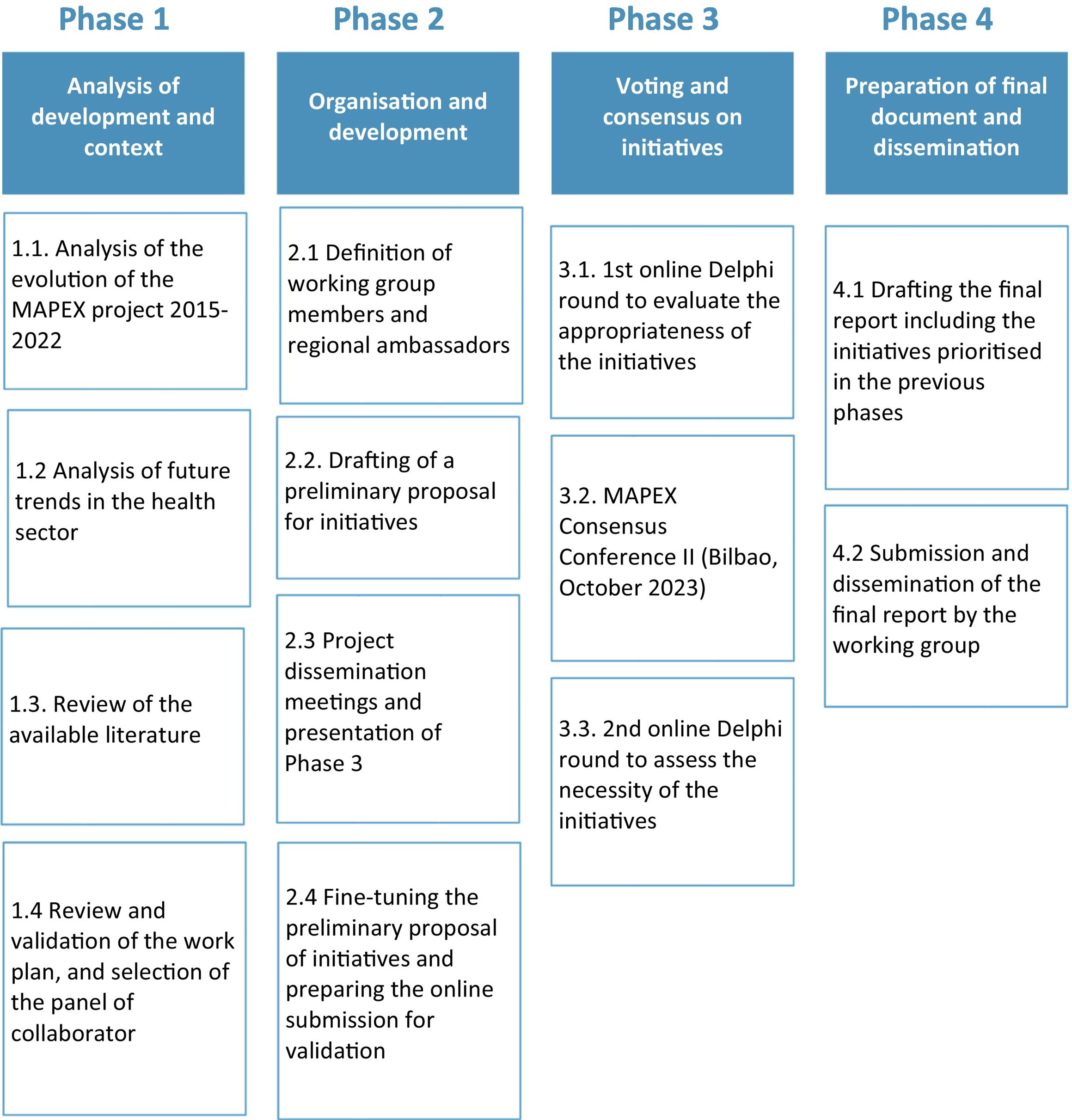
MethodThe study was carried out in 4 phases between January and December 2023.
For phase 1, a literature review of the evolution of the project was carried out by the coordinating committee with the aim of establishing a basis on which to define a new proposal for initiatives. In addition, an analysis was made of the health trends that will have an impact in the coming years.
In phase 2, a working group of 19 specialists from all the autonomous communities was created, who were called regional ambassadors. They all made a preliminary proposal of initiatives and established revisions for their adjustment and final version both online and in telematic meetings.
In phase 3, a consensus was established based on the Delphi-Rand/UCLA methodology with 2 rounds of online voting to select the initiatives classified as: priority and key or breakthrough.
Between the first and second round of voting, a face-to-face “Consensus Conference” was held, where the results of the first round were presented.
In phase 4, a public presentation was made in scientific forums and through the web.
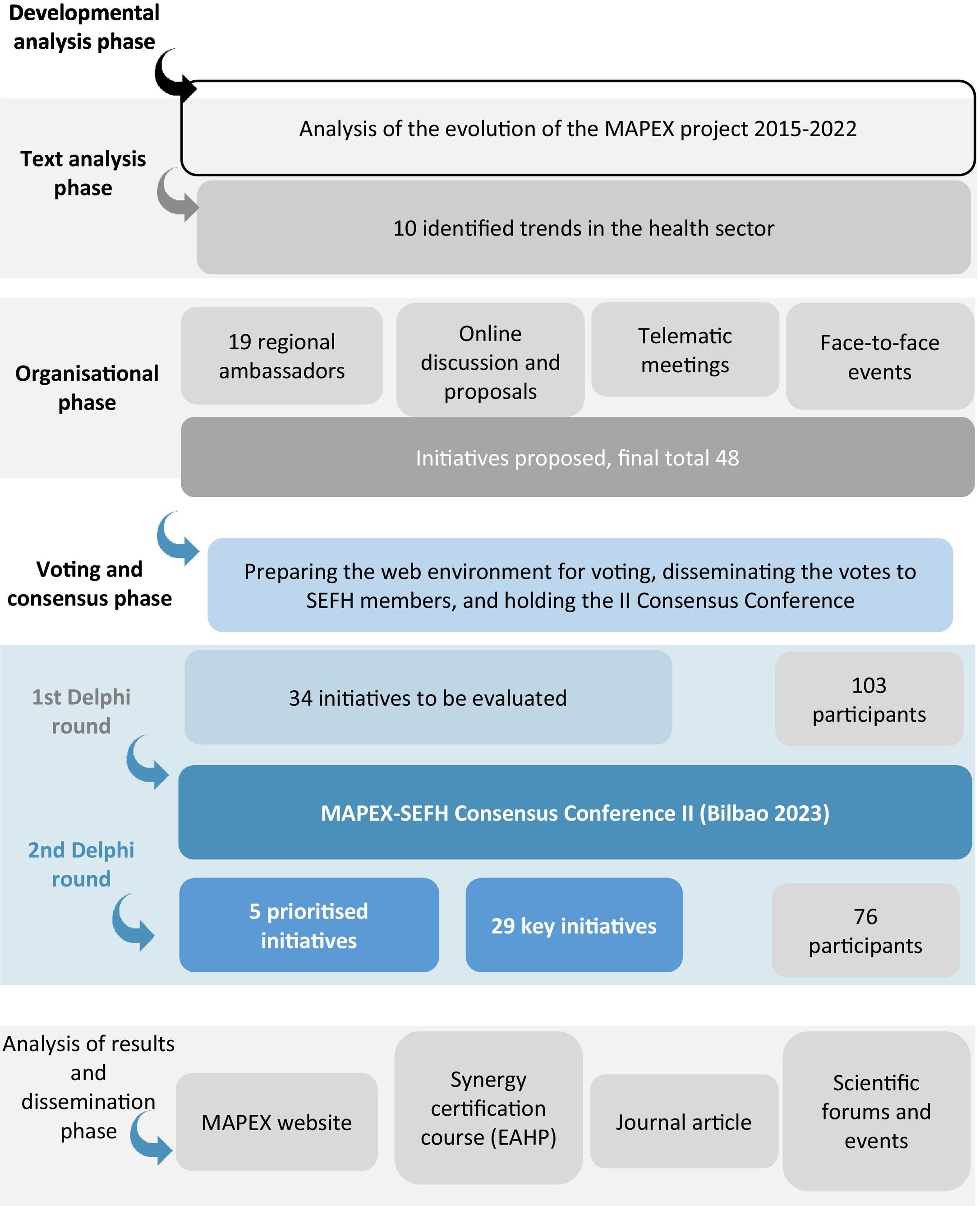
ResultsTen trends in the health sector were identified. A list of 34 initiatives grouped into 5 lines of work was established. A total of 103 panellists participated in the first round and 76 in the second. Finally, 5 initiatives were established as priority and 29 as key. Among those prioritised were external visibility, adaptations to the CMO methodology, strengthening certification, and improving training.
ConclusionsThe initiatives agreed upon as priorities were aimed at improving professional visibility, broadening the methodology of care work, expanding the quality of care, enhancing the training of professionals, and the voice of patients.
Priorizar las iniciativas a desarrollar para el desarrollo del proyecto Mapa estratégico de atención al paciente externo (MAPEX) para la mejora de la calidad asistencial y la Atención Farmacéutica a los pacientes atendidos en consultas externas de Farmacia Hospitalaria en el periodo 2024–2027 en España.
MétodoEl estudio se desarrolló en 4 fases entre enero y diciembre de 2023.
Para la fase 1, se llevó a cabo una revisión bibliográfica de la evolución del proyecto por parte del comité coordinador con el objetivo de establecer una base sobre la que definir una nueva propuesta de iniciativas. Por otro lado, se hizo un análisis de las tendencias en salud que van a impactar en los próximos años.
En la fase 2, se creó un grupo de trabajo conformado por 19 especialistas, procedentes de todas las comunidades autónomas, a los que se denominó embajadores regionales. Todos realizaron una propuesta preliminar de iniciativas y establecieron revisiones para su ajuste y versión definitiva tanto online como en reuniones telemáticas.
En la fase 3 se estableció un consenso basado en la metodología de Delphi-Rand/UCLA con dos rondas de votación online para seleccionar las iniciativas clasificadas como: prioritarias y claves o de avance.
Entre la primera y la segunda ronda de votaciones se llevó a cabo una «Conferencia de consenso» presencial, donde se expusieron los resultados de la primera ronda.
En la fase 4 se llevó a cabo la presentación pública en foros científicos y a través de la web.
ResultadosSe identificaron 10 tendencias en el sector salud. Se estableció una lista de 34 iniciativas agrupadas en 5 líneas de trabajo. En la primera ronda participaron 103 panelistas y en la segunda 76. Finalmente, 5 iniciativas fueron establecidas como prioritarias y 29 como claves. Entre las priorizadas se encontraron las de visibilidad externa, adaptaciones metodología CMO, potenciar certificación y mejorar la formación.
ConclusionesLas iniciativas consensuadas como prioritarias se orientaron a la mejora de la visibilización profesional, ampliar la metodología de trabajo asistencial, expandir la calidad asistencial, potenciar la capacitación de los profesionales y la voz de los pacientes.
The management of chronic disease has emerged as a key challenge for modern healthcare systems due to the exponential growth of these diseases and their impact on patients' quality of life.1 This situation has driven the need to rethink care strategies, health policies, and therapeutic approaches in order to address the issue in a comprehensive and sustainable way.2 The socio-economic burden of chronic care not only challenges the viability of health systems but also raises ethical questions about access to optimal care.3 Understanding the multifaceted nature of healthcare, its management, and health promotion have become key elements in optimising resources and improving quality of life. A number of institutions have been exploring innovative strategies in approaching healthcare in order to find comprehensive and sustainable solutions in healthcare management.4
In the field of hospital pharmacy (HP), the increasing number of patients seen in outpatient consultations, coupled with the scarcity of resources, has led to difficulties in forming multidisciplinary teams as well as significant variability in healthcare. This situation was identified by the Spanish Society of Hospital Pharmacy (SEFH) and prompted the creation of a joint initiative to provide a collaborative response to these challenges.5
In 2014, the “Strategic Map for Outpatient Pharmaceutical Care” (MAPEX-SEFH) was launched with a forward-looking vision, founded on principles of multidisciplinary and multidimensional care, excellence in knowledge, and the evaluation of outcomes.6
Since then, the provision of outpatient pharmaceutical care (PC) has undergone striking advances, gained increasing relevance, and become firmly established in the care portfolio of hospital pharmacy services (HPSs).
From the time of its inception, and following the Consensus Conference I in 2016, initiatives have emerged to address various challenges, including the “Model of Integration in the Care Team”,6 stratification tools,7 and documents on telepharmacy.8 However, one of the most notable aspects has been the redefinition of the concept of PC9 and the creation of the “CMO Model” of PC—based on capacity, motivation, and opportunity—which responded to the 3 major identified needs: personalised care, work toward pharmacotherapeutic objectives, and longitudinal follow-up.10 This model, which has been adapted for several diseases, has shown better results in practice than the traditional approach.11–13
In line with the commitment to quality care, the Q-PEX initiative was developed in 2019.14 This initiative aims to establish a reference framework for quality improvement in PC and is the first quality certification standard registered by the SEFH. This standard establishes the general principles of a management system and technical requirements to promote best practice in PC.
However, the evolution of healthcare requires continuous and specific refinement of outpatient PC, underlining the need to adapt approaches to ensure optimal proactive and participatory care.
The main objective of this study was to prioritise initiatives for the advancement of the MAPEX project, aimed at further improving the quality of care and PC for patients in outpatient HP consultations in Spain from 2024 to 2027.
MethodThe study was conducted in 4 phases between January and December 2023 (Fig. 1).
Phase 1 involved organising the work, analysing the development and context of the project, selecting the experts, and planning. Phase 2 addressed its development, Phase 3 focussed on voting and consensus of initiatives, and Phase 4 involved the preparation and dissemination of the final report.
Initially, Phase 1 involved analysing the development of the project from its inception in 2015 to 2022. This task was conducted by the coordinating committee composed of HP specialists with experience in PC from different HPSs. This group reviewed and validated the objectives, scope, expectations, and methodology. It also participated in the development of various defined actions over the course of the project including literature analysis, proposal development, consensus rounds, review of deliverables, and validation of the final report.
This was followed by a literature review and analysis of trends in the healthcare sector that could impact HP over the next 4 years. To achieve this, key MESH terms were identified and combined using the necessary boolean operators. These terms included HP, trends, and pharmaceutical innovation, to which the related terms health technology, artificial intelligence (AI), telepharmacy, personalised medicine, and pharmacogenomics were added. Systematic reviews and observational studies were screened to obtain an overview as well as specific data on trends. To identify the most relevant articles, the search was limited to those published in the last 7 years.
Finally, the work plan and the design for the selection of the panel contributors were validated.
In Phase 2, the so-called regional ambassadors, a group made up of 19 HPs representing all the Spanish Autonomous Communities, were selected by regional delegates of the SEFH governing board. Their task was to generate value proposals to prioritise at the upcoming conference. Initially, these proposals were received independently by the coordinating committee, which was responsible for collating and analysing them in order to avoid duplication or to merge those that were similar in wording. As a result, a report on initiatives was produced and returned to the ambassadors for their individual votes on the 34 proposals they deemed the most relevant to take forward to Phase 3.
Once all the contributions had been collected, a preliminary proposal was drafted, and semantic alignment revisions were made both offline and during several online work sessions. The first step in the development of the activities was to define the prioritisation criteria based on the analysis of the identified reference documents and in line with the previous initiatives developed within the MAPEX project. The proposed initiatives were then grouped into strategic lines.
Next, the preliminary proposal was sent online to all members of the ambassador committee for review. An online meeting was then held to adapt the initiatives, incorporate possible changes to the proposed considerations, establish the voting and consensus methodology, and develop the timetable to be followed.
The committee assessed the necessity and appropriateness of the proposals. Thus, an initiative was considered necessary if it had the ability to guide decision-making in PC. Similarly, appropriateness was assessed if the initiative could ensure optimal PC and help advance the profession.
From May to September 2023, several face-to-face and online meetings were held in different Autonomous Communities to report on the project's status from its inception to the present, as well as discuss the upcoming Consensus Conference.
In Phase 3, the consensus methodology was implemented. For this purpose, the initiatives defined in the preliminary proposal were identified and validated through the analysis of 2 evaluation rounds of an online questionnaire based on the Delphi-Rand/UCLA methodology.15 Voting was open to all SEFH members via the project website for 1 month.
In the first round, SEFH members and the coordinating group evaluated the initiatives based on the established criteria of necessity and appropriateness. They were scored on an ordinal scale ranging from 1 (minimum) to 10 (maximum) points.
After the first online round, the face-to-face MAPEX Consensus Conference II was held in Bilbao, where the preliminary results were presented and the second round of voting was announced.
A second round was then held online over 15 days, but only members who had voted in the first round were invited to participate. They were aware of the scores awarded and the median scores of the other participants, enabling them to re-evaluate and finalise the scores awarded.
The initiatives were ranked and prioritised as described below.
Priority initiatives: Those that can have a direct and relevant impact on PC-related patient decision-making and are considered essential and strategic to ensure optimal PC and the advancement of the profession. Appropriateness was determined by the median position of the scores awarded and the degree of consensus of these scores. Thus, all initiatives with a median score between 9 and 10 and for which more than 80% of the panellists reached a consensus were considered.
Key initiatives: Those which, without being essential, are strategic and add value to the PC process and professional development. Their development and implementation is therefore recommended. All initiatives with a median score between 7 and 9 and for which more than 80% of the panellists reached a consensus were considered.
Initiatives for progress: Those which, without being priority or key, can add value to the PC process and professional development, either partially or within specific care areas or HPSs. Therefore, their development and implementation is only recommended if all the preceding ones have been developed. Those with a median necessity score between 5 and 7 and for which more than 80% of the panellists reached a consensus were considered.
In Phase 4, the coordinating group prepared the final report, which was presented at the 5th Synergy Certification Course of the European Association of Hospital Pharmacists.
Finally, the report was sent to the coordinating group for final validation and then to the SEFH board of directors and all members via the MAPEX project website (Fig. 2).
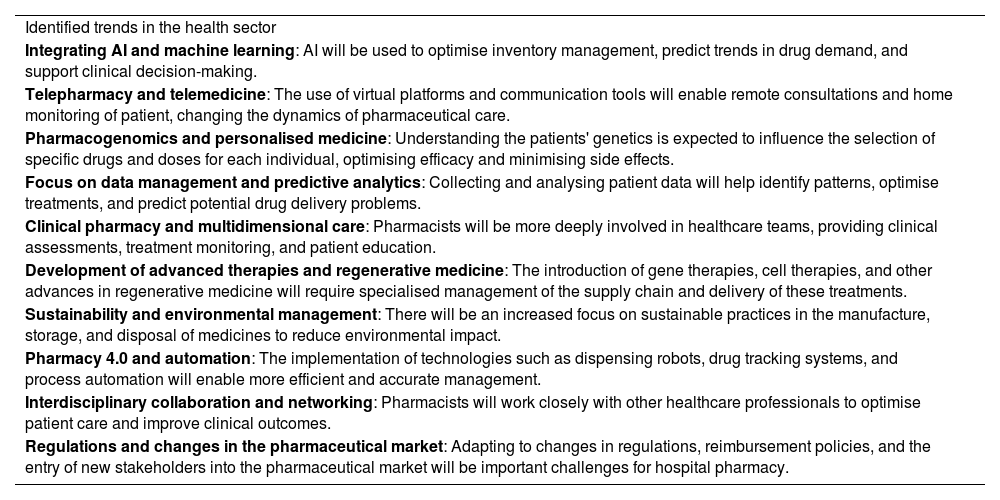
ResultsDuring Phase 1, the coordinating committee identified the 10 health sector trends that were considered to have the greatest future impact (Table 1).
Health sector trends identified as having an impact on hospital pharmacy between 2024 and 2027.
| Identified trends in the health sector |
| Integrating AI and machine learning: AI will be used to optimise inventory management, predict trends in drug demand, and support clinical decision-making. |
| Telepharmacy and telemedicine: The use of virtual platforms and communication tools will enable remote consultations and home monitoring of patient, changing the dynamics of pharmaceutical care. |
| Pharmacogenomics and personalised medicine: Understanding the patients' genetics is expected to influence the selection of specific drugs and doses for each individual, optimising efficacy and minimising side effects. |
| Focus on data management and predictive analytics: Collecting and analysing patient data will help identify patterns, optimise treatments, and predict potential drug delivery problems. |
| Clinical pharmacy and multidimensional care: Pharmacists will be more deeply involved in healthcare teams, providing clinical assessments, treatment monitoring, and patient education. |
| Development of advanced therapies and regenerative medicine: The introduction of gene therapies, cell therapies, and other advances in regenerative medicine will require specialised management of the supply chain and delivery of these treatments. |
| Sustainability and environmental management: There will be an increased focus on sustainable practices in the manufacture, storage, and disposal of medicines to reduce environmental impact. |
| Pharmacy 4.0 and automation: The implementation of technologies such as dispensing robots, drug tracking systems, and process automation will enable more efficient and accurate management. |
| Interdisciplinary collaboration and networking: Pharmacists will work closely with other healthcare professionals to optimise patient care and improve clinical outcomes. |
| Regulations and changes in the pharmaceutical market: Adapting to changes in regulations, reimbursement policies, and the entry of new stakeholders into the pharmaceutical market will be important challenges for hospital pharmacy. |
Abbreviation: AI, artificial intelligence.
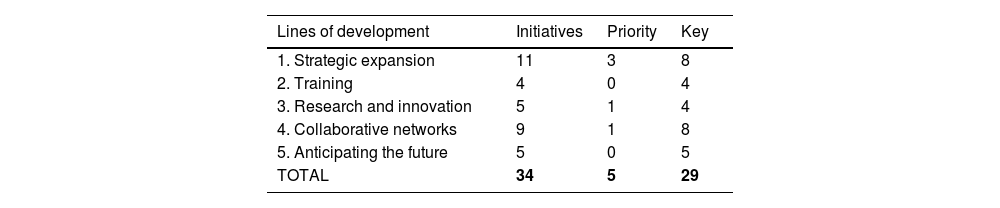
In Phase 2, a total of 48 initiatives were received, of which 34 were prioritised for consensus voting, after semantic and quality filtering. Based on the previously defined criteria of quality, necessity, and appropriateness, the initiatives were grouped into 5 lines of work: strategic expansion, training, research and innovation, collaborative networks, and anticipating the future.
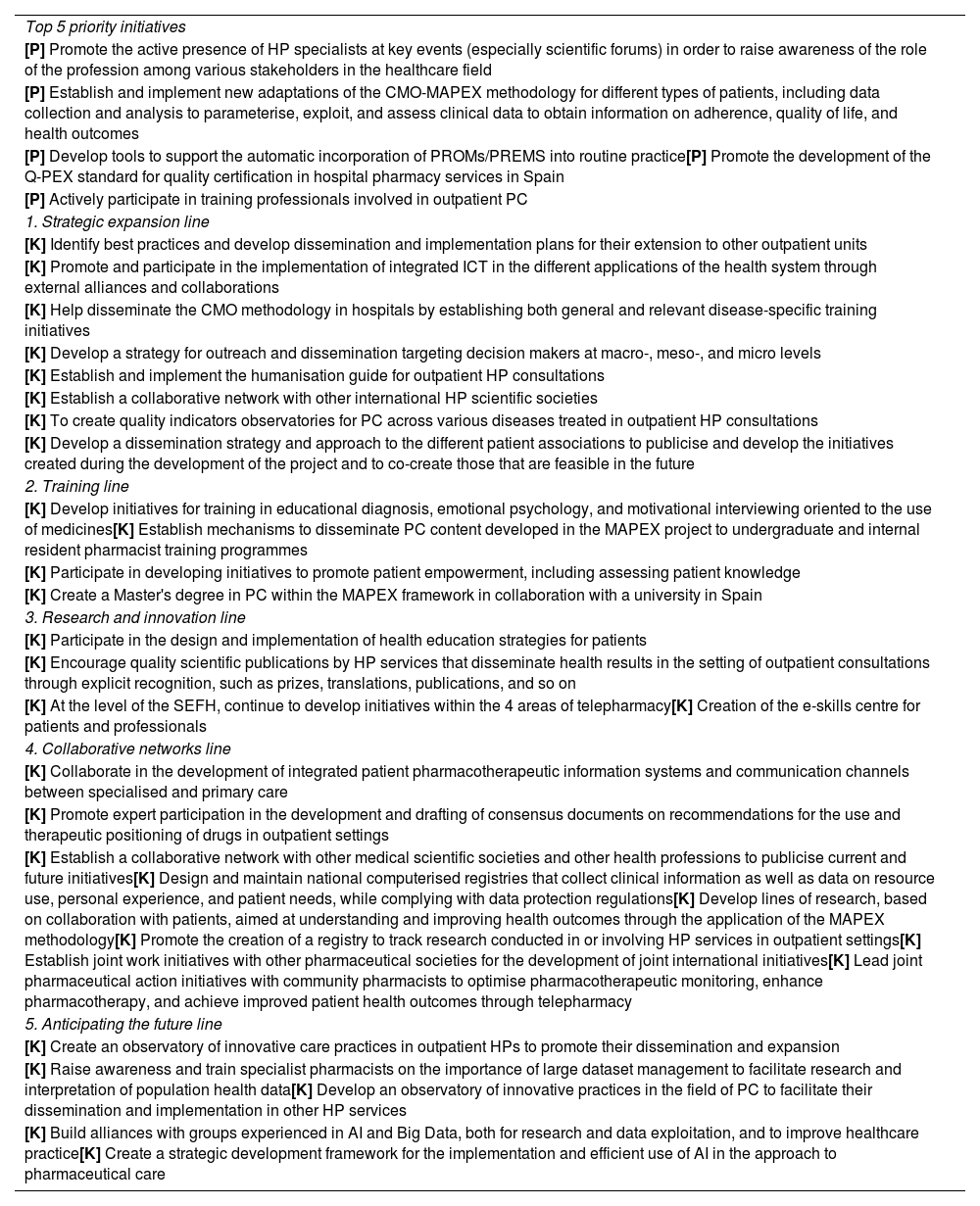
Table 2 summarises the initiatives grouped by the 5 lines of work considered.
In the first round of Phase 3, 103 completed questionnaires were received and 3 incomplete questionnaires were discarded. Of the 34 initiatives evaluated, 5 were considered priority and 29 were considered key. These preliminary results were presented at the face-to-face MAPEX Consensus Conference II.
In the second round, 79 questionnaires were received. Of these, 76 were completed, while 3 were incomplete and therefore discarded. Similarly to the first round, of the 34 initiatives evaluated, 5 were considered as priority, 29 as key, and 0 as progress.
Table 3 shows the priority and key initiatives.
Proposed priority and key initiatives.
| Top 5 priority initiatives |
| [P] Promote the active presence of HP specialists at key events (especially scientific forums) in order to raise awareness of the role of the profession among various stakeholders in the healthcare field |
| [P] Establish and implement new adaptations of the CMO-MAPEX methodology for different types of patients, including data collection and analysis to parameterise, exploit, and assess clinical data to obtain information on adherence, quality of life, and health outcomes |
| [P] Develop tools to support the automatic incorporation of PROMs/PREMS into routine practice[P] Promote the development of the Q-PEX standard for quality certification in hospital pharmacy services in Spain |
| [P] Actively participate in training professionals involved in outpatient PC |
| 1. Strategic expansion line |
| [K] Identify best practices and develop dissemination and implementation plans for their extension to other outpatient units |
| [K] Promote and participate in the implementation of integrated ICT in the different applications of the health system through external alliances and collaborations |
| [K] Help disseminate the CMO methodology in hospitals by establishing both general and relevant disease-specific training initiatives |
| [K] Develop a strategy for outreach and dissemination targeting decision makers at macro-, meso-, and micro levels |
| [K] Establish and implement the humanisation guide for outpatient HP consultations |
| [K] Establish a collaborative network with other international HP scientific societies |
| [K] To create quality indicators observatories for PC across various diseases treated in outpatient HP consultations |
| [K] Develop a dissemination strategy and approach to the different patient associations to publicise and develop the initiatives created during the development of the project and to co-create those that are feasible in the future |
| 2. Training line |
| [K] Develop initiatives for training in educational diagnosis, emotional psychology, and motivational interviewing oriented to the use of medicines[K] Establish mechanisms to disseminate PC content developed in the MAPEX project to undergraduate and internal resident pharmacist training programmes |
| [K] Participate in developing initiatives to promote patient empowerment, including assessing patient knowledge |
| [K] Create a Master's degree in PC within the MAPEX framework in collaboration with a university in Spain |
| 3. Research and innovation line |
| [K] Participate in the design and implementation of health education strategies for patients |
| [K] Encourage quality scientific publications by HP services that disseminate health results in the setting of outpatient consultations through explicit recognition, such as prizes, translations, publications, and so on |
| [K] At the level of the SEFH, continue to develop initiatives within the 4 areas of telepharmacy[K] Creation of the e-skills centre for patients and professionals |
| 4. Collaborative networks line |
| [K] Collaborate in the development of integrated patient pharmacotherapeutic information systems and communication channels between specialised and primary care |
| [K] Promote expert participation in the development and drafting of consensus documents on recommendations for the use and therapeutic positioning of drugs in outpatient settings |
| [K] Establish a collaborative network with other medical scientific societies and other health professions to publicise current and future initiatives[K] Design and maintain national computerised registries that collect clinical information as well as data on resource use, personal experience, and patient needs, while complying with data protection regulations[K] Develop lines of research, based on collaboration with patients, aimed at understanding and improving health outcomes through the application of the MAPEX methodology[K] Promote the creation of a registry to track research conducted in or involving HP services in outpatient settings[K] Establish joint work initiatives with other pharmaceutical societies for the development of joint international initiatives[K] Lead joint pharmaceutical action initiatives with community pharmacists to optimise pharmacotherapeutic monitoring, enhance pharmacotherapy, and achieve improved patient health outcomes through telepharmacy |
| 5. Anticipating the future line |
| [K] Create an observatory of innovative care practices in outpatient HPs to promote their dissemination and expansion |
| [K] Raise awareness and train specialist pharmacists on the importance of large dataset management to facilitate research and interpretation of population health data[K] Develop an observatory of innovative practices in the field of PC to facilitate their dissemination and implementation in other HP services |
| [K] Build alliances with groups experienced in AI and Big Data, both for research and data exploitation, and to improve healthcare practice[K] Create a strategic development framework for the implementation and efficient use of AI in the approach to pharmaceutical care |
Abbreviations: PC, pharmaceutical care; K, Key; CMO, capacity, motivation, opportunity; HP, hospital pharmacy; P, priority; AI, artificial intelligence; ICT, Information and Communication Technology.
Of the 5 prioritised initiatives, 3 were from the strategic expansion line, 1 was from training, 1 from research and innovation, and none from the other initiatives.
DiscussionThe selected initiatives are intended to guide HP specialists, heads of service, and health decision-makers in decision-making and to facilitate the development, implementation, measurement, and assessment of key aspects aimed at improving the quality of PC in outpatient consultations over the next 4 years. Among these initiatives, the consensus highlighted improving the visibility of the profession, expanding care activities based on the methodology already developed, monitoring clinical and patient-reported pharmacotherapeutic objectives, high-level training, and external evaluation of the care received.
It is noteworthy that the most valued initiative was enhancing the visibility of the role of the profession at key events, in contrast to “integration in multidisciplinary teams”, which was the most valued initiative at the first conference held in 2016.6 The implementation and development of the MAPEX initiatives has had a positive impact on the development of all outpatient PC settings,16 as described in the study by Vicente-Escrig et al. Having addressed this aspect, the HP group now plans to improve by building on the understanding that other professionals have of the new approach to their professional work.17
To facilitate this initiative, a “context analysis” will need to be conducted to review the current situation in detail and identify the key scientific events where the presence of HP specialists would have the greatest impact. It is also important to set clear objectives and specific measurable targets for their active participation in these forums. This should be supported by the identification of available human, financial, and logistic resources. A participation strategy should be developed to maximise the visibility of the profession. This involves preparing any form of participation that allows the role of profession to be disseminated among healthcare stakeholders. Likewise, alliances and collaboration should be established with other institutions in the sector to strengthen their presence and impact. In addition, continuous evaluation is required to measure the success of this initiative through predefined indicators. Continuous improvement adjustments should also be implemented based on the results obtained. Finally, further dissemination efforts and follow-up actions with stakeholders should be undertaken to maintain connections and sustain interest in the contributions of HP to the healthcare field.
The consensus also helped to identify other priority lines for action for the period 2024–2027. These include promoting the continuous improvement of patient care, as well as extending and implementing the overall model (CMO) to other diseases not yet addressed, in order to homogenise decision-making, standardise the recording of information, exploit data, and evaluate and improve outcomes. Studies conducted on the use of this approach have shown that it is superior to traditional monitoring, which has likely been a determining factor in its prioritisation.18,19
These initiatives should serve as a reference for monitoring and evaluating the quality of care, guiding management and decision-making, and establishing a system of continuous improvement. Their measurement and follow-up should involve the direct and indirect participation of the professionals involved, the patients, or their associations.
It would be ideal for each HPS to adapt these initiatives at a local level to better represent their specific circumstances and progress, as was done in the analysis for the previous conference. In recent years, several measures have been implemented to improve PC, such as specialised outpatient consultations, improved dispensing systems, and humanisation activities.20,21 These measures include the reorganisation of care, multidisciplinary and interlevel pharmaceutical interventions, and the promotion of counselling on the patients' relationships with their pharmacotherapy. In addition, we are considering the implementation of new technologies, particularly telepharmacy, for the continuous monitoring and evaluation of the effectiveness of pharmaceutical interventions based on dual PC.22
However, in order to meet the specific challenges of PC, we need to fully understand and align with the broader hospital setting.23 In the coming years, improving the organisation of healthcare and long-term care will be crucial.24 In addition, there is a clear commitment to improving patient experience and shared decision-making. Other challenges include adopting an approach that values integrated care with patient involvement, and adapting hospitals to serve as hubs for coordinated health management and activities in networked research and innovation.25 There are also the first signs of a shift toward future hospitals “without boundaries”, where care will be provided on the basis of the digitisation of home care processes.23 These challenges require a reevaluation of traditional approaches and the adoption of innovative strategies to ensure both the quality and accessibility of healthcare in general and PC in particular.
It is noteworthy that addressing the impact of AI was not prioritised, nor was there a high level of consensus on any aspects related to innovation or anticipating the future, including telepharmacy.
The set of initiatives envisaged should be capable of capturing the current and future state of PC. Therefore, just as this second edition of the Consensus Conference on initiatives represents a leap forward from the previous one, it is hoped that these lines of work will be updated over the next few years based on new scientific evidence and the evolving state of HPSs.
This study has several limitations, including the small number of votes received compared to the total SEFH membership. However, although the sample size was not determined, it was considered appropriate to include at least the same number of participants as at the Consensus Conference I held in 2016.
As in 2016 and 2021,6 future lines of research will include cross-sectional studies on the state of HPSs in Spain, assess the various defined lines of action implemented over specific time periods, and identify factors related to their achievement.
In conclusion, the priority initiatives aim to enhance outpatient care based on individualising care, improving efficiency, prioritising quality of care, and improving the training of professionals to achieve the best possible health outcomes for patients and the health system.
Contribution to the scientific literatureImproving the quality of care and PC of patients seen in HP outpatient consultations through a proactive and comprehensive approach is a priority objective in current healthcare improvement strategies and has been a central focus of the MAPEX-SEFH project since its inception.
The selected initiatives are intended to guide HP specialists, heads of service, and health decision-makers in decision-making and to facilitate the implementation, measurement, and assessment of key aspects aimed at improving the quality of PC in outpatient consultations. These initiatives include improving the visibility of the profession, coordinating care teams, expanding care activities, monitoring clinical and patient-reported pharmacotherapeutic objectives, high-level training, and external evaluation of the care received.
FundingNone declared.
Statement of AuthorshipAll authors contributed to developing the original idea and designing the study. Ramón Morillo-Verdugo was responsible for drafting the manuscript, which was reviewed by all authors, who approved the final version for publication.
CRediT authorship contribution statementRamón Morillo Verdugo: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision, Resources, Project administration, Methodology, Investigation, Formal analysis, Conceptualization. Beatriz Bernardez Ferrán: Writing – review & editing, Visualization, Validation. Aurora Fernández Polo: Writing – review & editing, Visualization, Validation. Luis Margusino Framiñan: Writing – review & editing, Writing – original draft, Validation, Supervision, Methodology, Conceptualization. José Manuel Martínez Sesmero: Writing – review & editing, Visualization, Validation. Manuel Velez-Diaz-Pallarés: Writing – review & editing, Visualization, Validation. Esther Vicente-Escrig: Writing – review & editing, Writing – original draft, Visualization, Validation, Methodology, Investigation, Conceptualization.
We would like to thank all the participants in the 2 consensus rounds for the development of the MAPEX-SEFH II project consensus conference, as well as the SEFH board of directors and SEFH governing board for supporting the project.
Representing the MAPEX-SEFH project ambassadors committee for the Consensus Conference II (in alphabetical order of surname):
Xabier Abasolo Tamayo, Amaya Arrondo Velasco, Javier Casas Arrate, Carmen Carriles, Ana Colón Lopez de Dicastillo, Pilar Diaz Ruiz, Esperanza Gutierrez Gutierrez, Alicia Lazaro Lopez, Alba León Barbosa, Gabriel Mercadal Orfila, Almudena Mancebo Gonzalez, Raquel Medina Comas, Herminia Navarro Aznarez, Carmen Obaldia Alaña, Elena Sanchez Yañez.